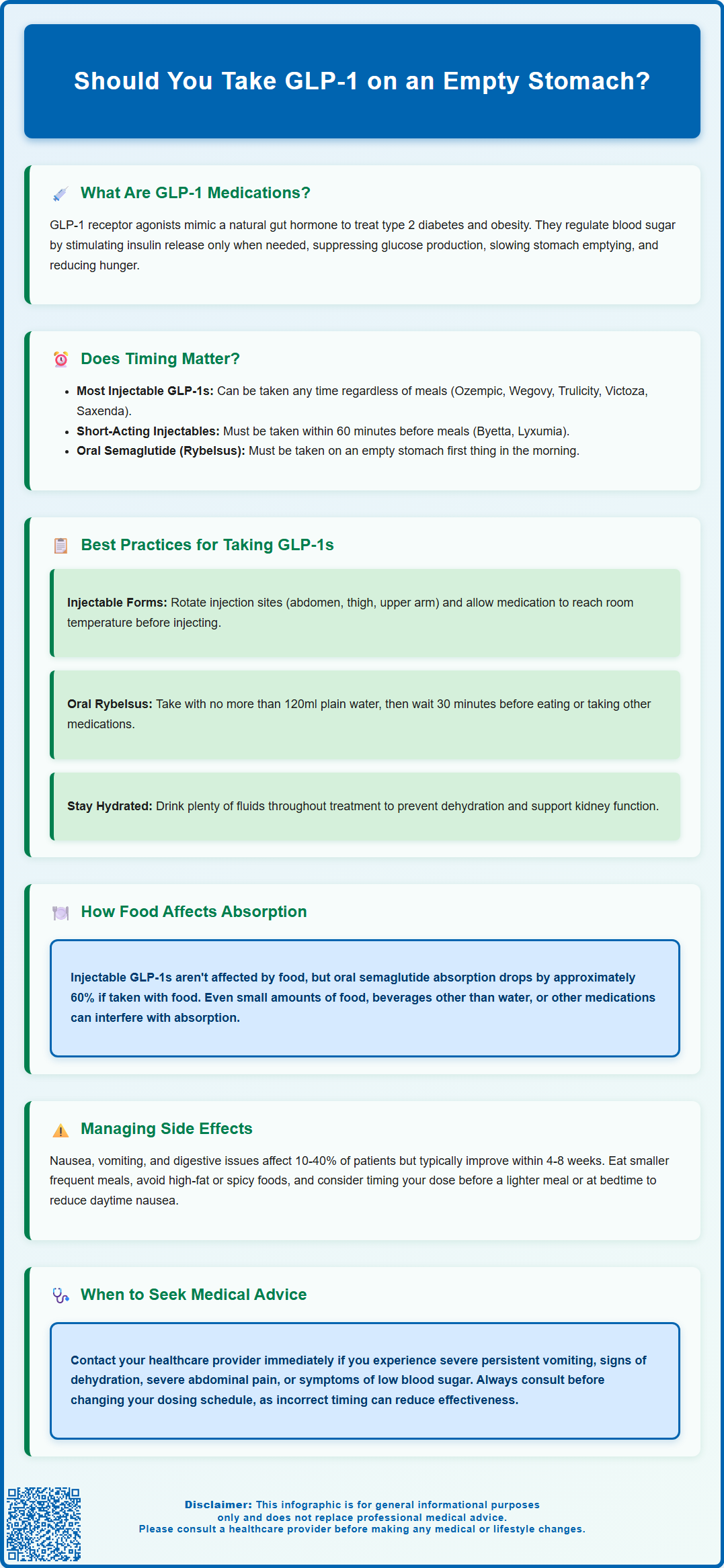
Should you take GLP-1 on an empty stomach? The answer depends entirely on which GLP-1 receptor agonist you have been prescribed. Most injectable formulations—such as semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda)—can be administered at any time, regardless of meals. However, oral semaglutide (Rybelsus) must be taken on an empty stomach with strict fasting requirements to ensure adequate absorption. Short-acting injectables like exenatide (Byetta) and lixisenatide (Lyxumia) require specific pre-meal timing. Understanding your medication's administration requirements is essential for optimal therapeutic benefit and glycaemic control. Always follow the instructions provided with your prescribed GLP-1 medication and consult your GP or pharmacist if uncertain.
Summary: Most injectable GLP-1 medications can be taken at any time regardless of meals, but oral semaglutide (Rybelsus) must be taken on an empty stomach with at least 30 minutes before food.
- GLP-1 receptor agonists are used to manage type 2 diabetes and obesity by stimulating insulin secretion, suppressing glucagon, and slowing gastric emptying.
- Injectable formulations (semaglutide, dulaglutide, liraglutide) are absorbed subcutaneously and do not require fasting or meal coordination.
- Oral semaglutide (Rybelsus) requires strict fasting: take on an empty stomach with ≤120ml water, wait 30 minutes before eating or taking other medications.
- Short-acting GLP-1 medications (exenatide immediate-release, lixisenatide) must be administered within 60 minutes before meals for optimal post-prandial glucose control.
- Food reduces oral semaglutide bioavailability by approximately 60%, making adherence to fasting requirements essential for therapeutic effectiveness.
- Common gastrointestinal side effects (nausea, vomiting, diarrhoea) typically diminish within 4–8 weeks; severe or persistent symptoms require medical review.
Table of Contents
What Are GLP-1 Medications and How Do They Work?
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications primarily used to manage type 2 diabetes mellitus and, more recently, obesity. These medicines mimic the action of naturally occurring GLP-1, a hormone produced in the intestine that plays a crucial role in glucose regulation and appetite control.
GLP-1 medications work through several complementary mechanisms. They stimulate insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning insulin is released only when blood glucose levels are elevated. This reduces the risk of hypoglycaemia compared to some other diabetes treatments. Simultaneously, they suppress glucagon release, a hormone that raises blood glucose, thereby preventing excessive glucose production by the liver. Additionally, GLP-1 receptor agonists slow gastric emptying, which moderates the rate at which nutrients enter the bloodstream after eating, and they act on appetite centres in the brain to promote satiety and reduce food intake.
Commonly prescribed GLP-1 medications in the UK include semaglutide (Ozempic, Wegovy, Rybelsus), dulaglutide (Trulicity), liraglutide (Victoza, Saxenda), lixisenatide (Lyxumia) and exenatide (Byetta, Bydureon). These are available in different formulations: most are administered as subcutaneous injections (once weekly or once daily), whilst semaglutide is also available as an oral tablet (Rybelsus). Some short-acting GLP-1 medications require specific meal-related timing.
NICE guidelines (NG28) support the use of GLP-1 receptor agonists for type 2 diabetes when glycaemic targets are not achieved with other therapies, and for weight management in specific circumstances (TA875 for Wegovy, TA664 for Saxenda). Understanding how these medications work helps patients appreciate why administration timing and food intake may influence their effectiveness and tolerability.
Should You Take GLP-1 on an Empty Stomach?
The answer to whether you should take GLP-1 medications on an empty stomach depends entirely on the specific formulation you have been prescribed. Different GLP-1 receptor agonists have distinct administration requirements, and following the correct instructions is essential for optimal therapeutic benefit.
Most injectable GLP-1 medications (such as semaglutide injections [Ozempic, Wegovy], dulaglutide [Trulicity], and liraglutide [Victoza, Saxenda]) can be administered at any time of day, regardless of meals. These subcutaneous injections do not require you to be fasting or to coordinate administration with food intake. The medication is absorbed directly into the bloodstream from subcutaneous tissue, bypassing the gastrointestinal tract, which means food in your stomach does not interfere with absorption.
However, there are important exceptions. Short-acting GLP-1 receptor agonists including exenatide immediate-release (Byetta) should be injected within 60 minutes before morning and evening meals, and lixisenatide (Lyxumia) should be administered within 1 hour before any meal of the day. This timing helps optimise their effect on post-meal blood glucose levels.
Oral semaglutide (Rybelsus) has very specific requirements and must be taken on an empty stomach. According to the MHRA-approved Summary of Product Characteristics (SmPC), Rybelsus should be taken first thing in the morning, with no more than 120ml of plain water, at least 30 minutes before any food, drink, or other oral medications. This is because oral semaglutide has relatively poor bioavailability, and the presence of food significantly reduces the amount of medication absorbed into the bloodstream.
Patients should always follow the specific instructions provided with their prescribed medication and consult their GP or pharmacist if uncertain. Taking oral semaglutide incorrectly can substantially reduce its effectiveness, whilst injectable formulations have varying requirements regarding meal timing. Never adjust your dosing schedule without professional guidance, as this may compromise glycaemic control or weight management outcomes.
How Food Affects GLP-1 Absorption and Effectiveness
The interaction between food and GLP-1 medications varies significantly depending on the route of administration and specific product, and understanding these differences is important for achieving optimal therapeutic outcomes.
For most injectable GLP-1 receptor agonists (such as semaglutide injections, dulaglutide, and liraglutide), food has minimal impact on drug absorption because the medication is delivered directly into subcutaneous tissue and absorbed into the systemic circulation independently of the gastrointestinal tract. Clinical studies have demonstrated that these injectable formulations maintain consistent pharmacokinetic profiles regardless of whether they are administered in fasted or fed states.
Short-acting GLP-1 receptor agonists like exenatide immediate-release (Byetta) and lixisenatide (Lyxumia) are specifically timed before meals. While food does not significantly alter their absorption, this pre-meal timing optimises their effect on post-prandial glucose control. For exenatide immediate-release, other oral medicines that require complete absorption (such as contraceptives and antibiotics) should be taken at least 1 hour before the injection, as the slowing of gastric emptying may affect their absorption.
Oral semaglutide (Rybelsus) presents a markedly different scenario. This formulation contains an absorption enhancer (SNAC) that facilitates uptake across the gastric mucosa, but this process is highly sensitive to gastric contents. When taken with food or shortly before eating, the bioavailability of oral semaglutide decreases by approximately 60%, according to the MHRA-approved SmPC. Even small amounts of food, beverages other than water, or other medications can interfere with absorption. This is why the strict fasting requirement exists: taking Rybelsus on an empty stomach, with only a small amount of plain water (up to 120ml), and waiting at least 30 minutes before consuming anything else maximises the amount of active drug that enters the bloodstream.
It is worth noting that whilst food does not affect the absorption of most injectable GLP-1 medications, the therapeutic effects of all GLP-1 receptor agonists inherently involve interactions with food intake. These medications slow gastric emptying and reduce appetite, which means patients often experience changes in their eating patterns, portion sizes, and food preferences. Some individuals find that eating smaller, more frequent meals helps manage gastrointestinal side effects, but this relates to tolerability rather than drug absorption.
Best Practices for Taking GLP-1 Medications
Adhering to best practices when taking GLP-1 medications ensures you receive the full therapeutic benefit whilst minimising potential side effects. The following guidance reflects current clinical recommendations and patient safety advice.
For injectable GLP-1 medications:
-
Timing requirements: For once-weekly injections (semaglutide [Ozempic, Wegovy], dulaglutide [Trulicity], exenatide extended-release), administration can occur at any time of day, with or without food. For short-acting formulations, follow specific timing: exenatide immediate-release (Byetta) should be injected within 60 minutes before morning and evening meals; lixisenatide (Lyxumia) should be given within 1 hour before any meal.
-
Injection technique: Rotate injection sites (abdomen, thigh, or upper arm) to reduce the risk of lipohypertrophy (fatty lumps under the skin). Ensure the medication has reached room temperature before injecting to improve comfort.
-
Storage: Keep unused pens in the refrigerator (2–8°C). Once in use, most pens can be stored at room temperature (below 30°C) for a specified period—check your patient information leaflet.
-
Missed doses: Follow product-specific guidance. For semaglutide (Ozempic), take within 5 days of the missed dose; for dulaglutide, within 3 days; for Wegovy, additional rules apply for consecutive missed doses. Always refer to your product's patient information leaflet for exact instructions.
-
Safety: Never share pens with others, even if the needle is changed. Dispose of used needles in a proper sharps container.
For oral semaglutide (Rybelsus):
-
Strict fasting protocol: Take your tablet first thing in the morning on an empty stomach with no more than 120ml of plain water.
-
30-minute wait: Do not eat, drink anything other than water, or take other oral medications for at least 30 minutes after taking Rybelsus. Some patients find setting an alarm helpful.
-
Swallow whole: Do not split, crush, or chew the tablet, as this affects the absorption enhancer.
-
Missed dose: If you miss a dose, skip that day's dose and take your next tablet the following day. Do not take an extra tablet to make up for the missed dose.
General advice for all GLP-1 medications:
-
Gradual dose escalation: Your prescriber will typically start you on a low dose and increase gradually over several weeks. This approach minimises gastrointestinal side effects.
-
Hydration: Maintain adequate fluid intake, particularly if experiencing nausea or vomiting, to prevent dehydration and potential kidney problems.
-
Blood glucose monitoring: If you have diabetes, continue monitoring your blood glucose as advised, particularly when starting treatment or adjusting doses. If you also take insulin or sulfonylureas, your doctor may reduce these doses to prevent hypoglycaemia.
-
Pregnancy and breastfeeding: GLP-1 medications are generally not recommended during pregnancy or breastfeeding. Discuss effective contraception with your healthcare provider if you are of childbearing potential.
-
Regular follow-up: Attend scheduled appointments with your GP or diabetes specialist nurse to assess treatment response, adjust doses, and monitor for adverse effects.
Common Side Effects and How Timing Can Help
GLP-1 receptor agonists are generally well tolerated, but gastrointestinal side effects are common, particularly when initiating treatment or increasing doses. Understanding these effects and how administration timing may influence them can improve your treatment experience.
The most frequently reported side effects include:
-
Nausea (affecting approximately 10–40% of patients, depending on the specific medication)
-
Vomiting
-
Diarrhoea
-
Constipation
-
Abdominal discomfort or bloating
-
Reduced appetite
These effects typically occur because GLP-1 medications slow gastric emptying and affect gut motility. Most patients find that gastrointestinal symptoms diminish over time as the body adjusts to the medication, usually within 4–8 weeks. The gradual dose escalation protocols are specifically designed to minimise these effects.
How timing strategies can help manage side effects:
For injectable formulations that can be taken regardless of meals (such as semaglutide injections, dulaglutide, liraglutide), some patients find that timing their injection relative to meals can influence tolerability. For example, administering your weekly injection before a lighter meal or in the evening before bed may reduce daytime nausea. However, there is no official guidance mandating specific meal timing for these injections—this is about individual preference and symptom management.
With oral semaglutide, the mandatory fasting period means you take the medication on an empty stomach, which some patients initially find challenging if they experience morning nausea. However, maintaining this routine is essential for drug effectiveness.
Additional strategies to manage side effects:
-
Eat smaller, more frequent meals rather than large portions
-
Avoid high-fat, greasy, or spicy foods that may exacerbate nausea
-
Stay well hydrated to prevent dehydration and potential kidney problems
-
Eat slowly and stop when you feel comfortably full
-
Consider ginger tea or other natural remedies for nausea (discuss with your pharmacist)
When to seek medical advice:
Contact your GP or healthcare provider if you experience:
-
Severe, persistent vomiting that prevents adequate fluid intake
-
Signs of dehydration (dark urine, dizziness, reduced urination) which may lead to acute kidney injury
-
Severe abdominal pain, particularly if accompanied by vomiting (potential pancreatitis)
-
Symptoms of hypoglycaemia if taking other diabetes medications
-
Visual changes or eye symptoms, particularly if you have pre-existing diabetic retinopathy
-
New or worsening mood changes, including thoughts of self-harm
-
Persistent side effects that significantly affect your quality of life
Rare but serious adverse effects include pancreatitis, gallbladder problems, and thyroid C-cell tumours (observed in animal studies, with uncertain relevance to humans). Report any suspected side effects via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk) or to your prescriber.
Frequently Asked Questions
Can I take injectable semaglutide (Ozempic or Wegovy) with food?
Yes, injectable semaglutide can be administered at any time of day, with or without food. The subcutaneous injection is absorbed directly into the bloodstream, so food does not affect its absorption or effectiveness.
Why must oral semaglutide (Rybelsus) be taken on an empty stomach?
Oral semaglutide has poor bioavailability, and food reduces absorption by approximately 60%. Taking it on an empty stomach with only plain water, and waiting at least 30 minutes before eating, maximises the amount of medication absorbed into the bloodstream.
What should I do if I experience nausea when taking GLP-1 medication?
Nausea is common when starting GLP-1 medications but typically improves within 4–8 weeks. Eat smaller, more frequent meals, avoid high-fat foods, stay well hydrated, and consider timing your injection before a lighter meal if using an injectable formulation. Contact your GP if nausea is severe or persistent.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript