Should you take GLP-1 in the morning or night? The answer depends primarily on the specific medication and formulation prescribed. GLP-1 receptor agonists are increasingly used to manage type 2 diabetes and support weight management in the UK. Whilst once-weekly preparations such as semaglutide and dulaglutide can be administered at any time of day, other formulations have more specific timing requirements. Understanding the optimal dosing schedule for your particular GLP-1 medication—alongside practical considerations such as meal patterns, side effects, and daily routine—can help maximise therapeutic benefit and improve adherence to treatment.
Summary: The optimal timing for GLP-1 medications depends on the specific formulation: once-weekly preparations can be taken at any time of day, whilst oral semaglutide must be taken on an empty stomach in the morning.
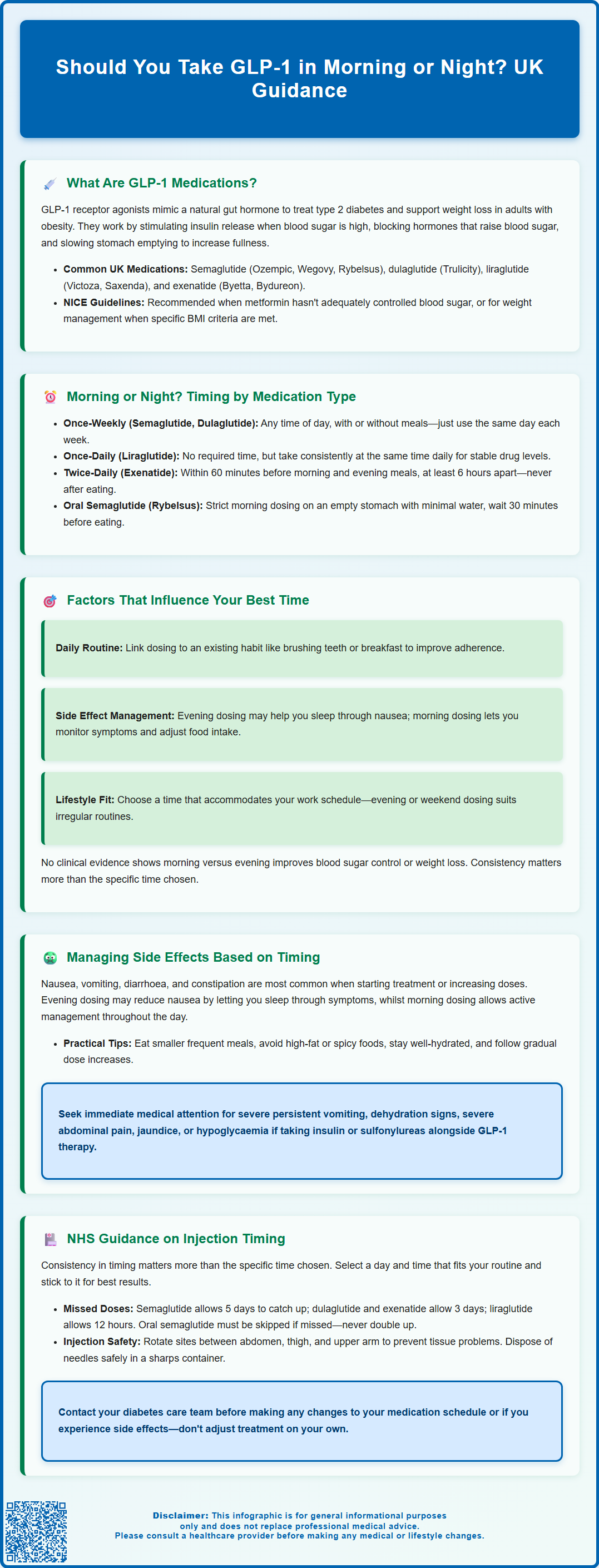
- GLP-1 receptor agonists stimulate insulin secretion, suppress glucagon release, and slow gastric emptying to control blood glucose and support weight management.
- Once-weekly injectable formulations such as semaglutide and dulaglutide can be administered at any time of day, provided consistency is maintained.
- Oral semaglutide (Rybelsus) must be taken on an empty stomach upon waking with a small sip of water, waiting at least 30 minutes before eating.
- Twice-daily exenatide should be administered within 60 minutes before morning and evening meals for optimal post-meal glucose control.
- Common side effects include nausea and gastrointestinal symptoms; strategic timing and dose escalation can improve tolerability.
- NHS guidance emphasises consistency over specific timing, with individualised advice from diabetes care teams recommended for optimal adherence.
Table of Contents
What Are GLP-1 Medications and How Do They Work?
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications primarily used to manage type 2 diabetes mellitus and, more recently, for weight management in adults with obesity or overweight with weight-related comorbidities. These medicines mimic the action of the naturally occurring hormone GLP-1, which is released from the gut in response to food intake.
GLP-1 medications work through several complementary mechanisms. They stimulate insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning insulin is only released when blood glucose levels are elevated. This reduces the risk of hypoglycaemia compared to some other diabetes medications. Simultaneously, they suppress glucagon release, a hormone that raises blood glucose, thereby preventing excessive glucose production by the liver. Additionally, GLP-1 receptor agonists slow gastric emptying, which prolongs the feeling of fullness after meals and helps regulate post-meal blood glucose spikes.
Commonly prescribed GLP-1 medications in the UK include semaglutide (available as injectable Ozempic, Wegovy and oral tablet Rybelsus), dulaglutide (Trulicity), liraglutide (Victoza, Saxenda), and exenatide (Byetta, Bydureon). Most are administered via subcutaneous injection, with dosing frequencies ranging from twice daily to once weekly, depending on the specific formulation. Oral semaglutide (Rybelsus) is the only tablet formulation currently available.
NICE guidance (NG28) recommends GLP-1 receptor agonists for type 2 diabetes in specific clinical circumstances, typically when metformin and other treatments have not achieved glycaemic targets. For weight management, NICE technology appraisals specify eligibility criteria including minimum BMI thresholds and require initiation within specialist weight management services.
Understanding how these medications function is essential for optimising their use, including determining the most appropriate time of day for administration to maximise therapeutic benefit and minimise adverse effects.
Should You Take GLP-1 in the Morning or Night?
The optimal timing for GLP-1 medication depends primarily on the specific medication and formulation you have been prescribed. For once-weekly preparations such as semaglutide (Ozempic, Wegovy) and dulaglutide (Trulicity), the time of day is generally less critical because these long-acting formulations maintain steady drug levels throughout the week. According to their SmPCs, patients can inject these medications at any time of day, with or without meals, provided they maintain consistency with their chosen day of the week.
For once-daily GLP-1 medications like liraglutide (Victoza, Saxenda), there is similarly no absolute requirement to inject at a specific time. However, establishing a consistent routine—whether morning or evening—helps ensure adherence and maintains stable therapeutic levels. Some patients prefer morning administration to align with their daily routine, whilst others find evening dosing more convenient.
Twice-daily formulations such as immediate-release exenatide (Byetta) have more specific timing requirements. These should be administered within 60 minutes before morning and evening meals (or the two main meals of the day, at least 6 hours apart) and should not be taken after meals. This timing optimises the medication's effect on post-meal glucose control and takes advantage of its gastric-emptying properties.
Oral semaglutide (Rybelsus) has strict timing requirements. It must be taken on an empty stomach upon waking with a small sip of water (up to 120 ml), then waiting at least 30 minutes before consuming any food, drink, or other oral medications. This specific morning administration is essential for proper absorption.
It is important to note that there is no official clinical evidence suggesting that morning or night dosing provides superior glycaemic control or weight loss outcomes for most injectable GLP-1 preparations. The manufacturer's guidance and your prescriber's instructions should always take precedence. If you are uncertain about the best timing for your specific medication, consult your GP, practice nurse, or diabetes specialist nurse for personalised advice tailored to your treatment regimen and lifestyle.
Factors That Influence the Best Time to Take GLP-1
Several practical and clinical factors can help determine the most suitable time for your individual circumstances. Personal routine and adherence are paramount—choosing a time that fits seamlessly into your daily schedule significantly improves medication compliance. Many patients find that linking their medication to an existing habit, such as brushing teeth or preparing breakfast, serves as an effective reminder.
Meal timing and dietary patterns may influence your decision, particularly if you experience gastrointestinal side effects. Since GLP-1 medications slow gastric emptying and can cause nausea, some patients report that evening dosing helps them manage these symptoms overnight. Conversely, others find morning dosing preferable, allowing them to monitor how they feel throughout the day and adjust food intake accordingly.
Work schedule and lifestyle considerations are equally important. Healthcare workers on shift patterns, frequent travellers, or individuals with irregular routines may benefit from evening dosing when their schedule is more predictable. For once-weekly injections, selecting a day when you have time to manage the injection calmly—such as a weekend morning—can reduce stress and improve technique.
Concurrent medications should also be considered. If you take other diabetes medications, particularly insulin or sulfonylureas, there is an increased risk of hypoglycaemia. Dose adjustments of these medications may be required when starting GLP-1 therapy, regardless of timing. Additionally, the delayed gastric emptying caused by GLP-1 medications may affect the absorption of some oral medicines, so follow product-specific guidance and consult your healthcare provider about potential interactions.
Finally, individual response to side effects varies considerably. Some patients find that evening dosing helps them manage daytime nausea, whilst others find morning administration allows them to eat lighter evening meals, which may further support weight management goals. There is no one-size-fits-all approach; the best time is ultimately the one that you can maintain consistently whilst managing any adverse effects effectively.
Managing Side Effects Based on Dosing Time
Gastrointestinal side effects—particularly nausea, vomiting, diarrhoea, and constipation—are the most commonly reported adverse effects of GLP-1 medications, especially during the initial weeks of treatment or following dose escalation. Strategic timing of your medication can help mitigate these symptoms and improve tolerability.
For patients experiencing significant nausea, some find that evening dosing may be advantageous. Some patients report that taking their medication before bed means they may experience less discomfort during sleep. However, if nausea persists into the following day, morning dosing might be preferable, enabling you to manage symptoms actively and adjust meal sizes and composition throughout the day.
Appetite suppression is both a therapeutic effect and a potential challenge. If you find that reduced appetite interferes with adequate nutrition, consider timing your medication to align with your eating patterns. For instance, if you struggle to eat breakfast, evening dosing may allow for a more substantial morning meal.
Other strategies to manage side effects include:
-
Eating smaller, more frequent meals rather than large portions
-
Avoiding high-fat, greasy, or spicy foods that may exacerbate nausea
-
Staying well-hydrated, particularly if experiencing vomiting or diarrhoea
-
Gradually escalating the dose as prescribed, allowing your body time to adjust
When to seek medical advice: Contact your GP or diabetes care team promptly if you experience severe or persistent vomiting that prevents adequate fluid intake, signs of dehydration, severe abdominal pain (which could indicate pancreatitis or gallbladder problems), or jaundice. If you are taking insulin or sulfonylureas alongside GLP-1 therapy and experience hypoglycaemia, discuss dose adjustments with your healthcare provider. Patients with pre-existing diabetic retinopathy should be aware that rapid improvement in blood glucose control may temporarily worsen retinopathy, particularly with semaglutide.
If side effects significantly impair your quality of life despite timing adjustments, your prescriber may consider dose modification or alternative treatment options. Report any suspected side effects to the MHRA through the Yellow Card scheme (yellowcard.mhra.gov.uk).
NHS Guidance on GLP-1 Injection Timing
The NHS and NICE provide evidence-based guidance on GLP-1 receptor agonist use, though specific recommendations on timing generally align with manufacturer instructions rather than prescriptive clinical protocols. NICE guideline NG28 for type 2 diabetes and technology appraisals for weight management formulations emphasise the importance of patient education and individualised care when initiating GLP-1 therapy.
NHS patient information resources stress that consistency is more important than the specific time chosen. For once-weekly preparations, patients are advised to select a day and approximate time that suits their routine and maintain this schedule. If a dose is missed, product-specific guidance applies:
-
For semaglutide (Ozempic, Wegovy): Administer within 5 days of the missed dose, then resume the regular schedule. If more than 5 days have passed, skip the missed dose.
-
For dulaglutide (Trulicity) and exenatide (Bydureon): Administer within 3 days of the missed dose, then resume the regular schedule. If more than 3 days have passed, skip the missed dose.
For once-daily formulations like liraglutide (Victoza, Saxenda), the NHS advises taking the injection at approximately the same time each day. If a dose is missed and fewer than 12 hours have elapsed since the usual time, it can still be administered. Beyond this window, patients should skip the dose and continue with the next scheduled injection.
For oral semaglutide (Rybelsus), strict morning administration is essential. If a dose is missed, skip that day's dose and take a single dose the following morning. Never take a double dose to make up for a missed one.
Healthcare professional support is integral to successful GLP-1 therapy. Practice nurses and diabetes specialist nurses typically provide initial training, covering proper technique, site rotation for injections (abdomen, thigh, or upper arm), and safe disposal of sharps. They can offer personalised advice on timing based on your lifestyle, work patterns, and any side effects experienced.
Patients should be aware that GLP-1 medications are initiated and monitored within specialist or primary care diabetes services. Regular review appointments assess treatment response, tolerability, and continuation criteria. If you have concerns about timing, side effects, or treatment efficacy, contact your diabetes care team rather than making changes independently. Report any suspected side effects to the MHRA through the Yellow Card scheme (yellowcard.mhra.gov.uk).
Scientific References
Frequently Asked Questions
Can I take my once-weekly GLP-1 injection at any time of day?
Yes, once-weekly preparations such as semaglutide (Ozempic, Wegovy) and dulaglutide (Trulicity) can be administered at any time of day, with or without meals. The key is to maintain consistency with your chosen day and approximate time each week.
Does morning or evening dosing affect GLP-1 side effects?
Some patients find that evening dosing helps manage daytime nausea, whilst others prefer morning administration to monitor symptoms throughout the day. Individual response varies, so choose a time that helps you manage side effects most effectively.
What should I do if I miss a dose of my GLP-1 medication?
For once-weekly semaglutide, administer within 5 days of the missed dose; for dulaglutide and exenatide, within 3 days. If more time has passed, skip the missed dose and resume your regular schedule. Never take a double dose.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript