Choosing the best day to start GLP-1 receptor agonist therapy is a common question for patients beginning treatment for type 2 diabetes or weight management. Whilst there is no medical evidence that one day offers superior clinical outcomes over another, practical considerations can influence your experience during the initial phase of treatment. Many patients find it helpful to commence therapy at a weekend or during a period with fewer commitments, allowing time to monitor early side effects such as nausea. This article explores the factors to consider when timing your first GLP-1 dose, helping you make an informed decision in consultation with your healthcare team.
Summary: There is no clinically superior day to start GLP-1 receptor agonist therapy, but beginning at a weekend or during reduced commitments allows time to monitor initial side effects.
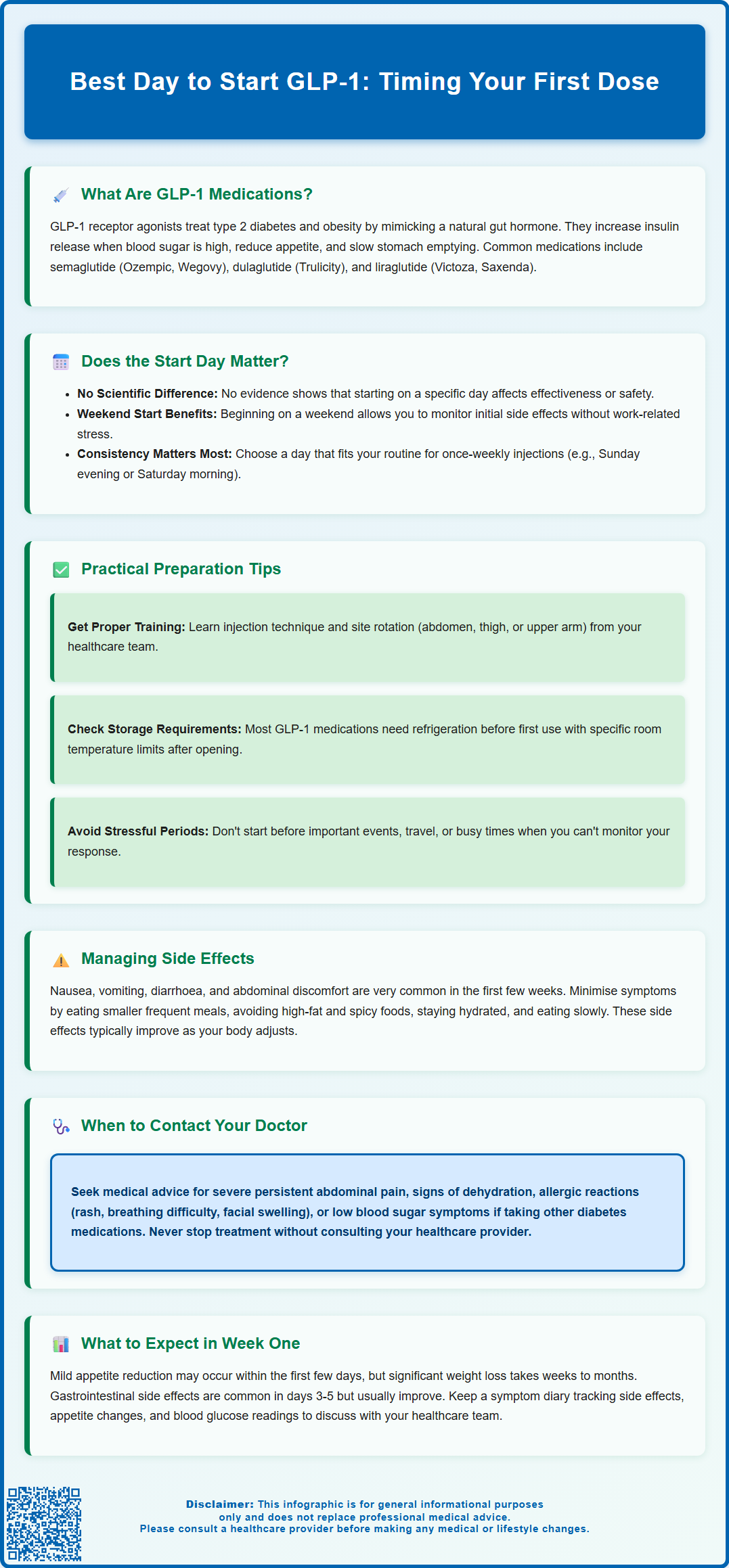
- GLP-1 receptor agonists are injectable medications for type 2 diabetes and weight management that mimic the incretin hormone GLP-1.
- The medication's efficacy depends on consistent administration and gradual dose escalation, not the specific day of initiation.
- Starting during a weekend or less busy period allows patients to manage common gastrointestinal side effects such as nausea without work pressures.
- Once-weekly formulations require choosing a consistent day that fits your routine to maintain adherence and therapeutic effect.
- Dose escalation follows evidence-based protocols over several weeks to minimise adverse effects and should not be accelerated without medical supervision.
- Contact your GP or diabetes specialist nurse if you experience severe abdominal pain, persistent vomiting, allergic reactions, or hypoglycaemia symptoms.
Table of Contents
What Are GLP-1 Receptor Agonists and How Do They Work?
GLP-1 receptor agonists are a class of medications primarily used to manage type 2 diabetes mellitus and, more recently, for weight management in adults with obesity or overweight with weight-related comorbidities. These medicines mimic the action of glucagon-like peptide-1 (GLP-1), a naturally occurring incretin hormone produced in the intestine in response to food intake.
The mechanism of action involves several physiological pathways. GLP-1 receptor agonists bind to GLP-1 receptors on pancreatic beta cells, stimulating glucose-dependent insulin secretion. This means insulin is released only when blood glucose levels are elevated, thereby reducing the risk of hypoglycaemia compared to some other diabetes medications. Additionally, these agents suppress glucagon secretion from pancreatic alpha cells, which helps prevent excessive glucose production by the liver. They also slow gastric emptying, prolonging the sensation of fullness after meals, and act on appetite centres in the brain to reduce hunger and food intake.
Commonly prescribed GLP-1 receptor agonists in the UK include semaglutide (Ozempic for diabetes; Wegovy for weight management; Rybelsus as an oral tablet for diabetes), dulaglutide (Trulicity for diabetes), liraglutide (Victoza for diabetes; Saxenda for weight management), and exenatide (Byetta, Bydureon for diabetes). Most are administered via subcutaneous injection, with dosing frequencies ranging from once daily to once weekly, depending on the specific formulation.
According to NICE guidance (NG28 for diabetes; TA875 for semaglutide and TA664 for liraglutide in weight management), GLP-1 receptor agonists are recommended as part of a comprehensive treatment strategy that includes dietary modification, increased physical activity, and other glucose-lowering therapies when appropriate. For weight management, these medications should be prescribed within specialist weight management services. GLP-1 receptor agonists are not indicated for type 1 diabetes or diabetic ketoacidosis.
Importantly, these medications should be used with caution in certain populations. They are not recommended during pregnancy or breastfeeding, and women of childbearing potential should use effective contraception. Semaglutide should be discontinued at least 2 months before a planned pregnancy. Some GLP-1 receptor agonists have restrictions in renal impairment (e.g., exenatide is not recommended if eGFR <30 mL/min/1.73 m²).
Does the Day You Start GLP-1 Treatment Matter?
From a pharmacological perspective, there is no official evidence suggesting that starting GLP-1 therapy on a particular day of the week confers any clinical advantage in terms of efficacy or safety. The medication's therapeutic effects depend on consistent administration and gradual dose escalation rather than the specific day of initiation. GLP-1 receptor agonists work by establishing steady-state concentrations in the body over time, and their glucose-lowering and appetite-suppressing effects develop progressively over several weeks.
However, practical considerations may influence the optimal day to commence treatment for individual patients. Many healthcare professionals and patients find it helpful to start GLP-1 therapy at the beginning of a weekend or during a period of reduced work or social commitments. This approach allows patients to monitor their initial response to the medication, particularly any gastrointestinal side effects such as nausea or diarrhoea, without the added stress of work obligations or important social events.
For once-weekly formulations (such as semaglutide or dulaglutide), choosing a consistent day that fits into your routine is more important than the specific day itself. Some patients prefer administering their injection on the same day each week when they have time to prepare, such as a Sunday evening or Saturday morning. This consistency helps establish a routine and reduces the likelihood of missed doses.
If you do miss a dose of a weekly GLP-1 medication, follow the product-specific guidance. For semaglutide (Ozempic, Wegovy), take the missed dose within 5 days of the scheduled time; if more than 5 days have passed, skip that dose and take the next one as scheduled. For dulaglutide (Trulicity), take the missed dose as soon as possible if there are at least 3 days (72 hours) until your next scheduled dose. Setting reminders on your phone or calendar can help maintain consistency.
There is no medical contraindication to starting GLP-1 therapy on any particular day. The decision should be individualised based on your personal schedule, support network availability, and when you feel most prepared to begin a new medication regimen. Discuss your preferences with your prescribing clinician, who can provide guidance tailored to your circumstances and help you establish a sustainable administration schedule.
Practical Considerations for Starting GLP-1 Medication
Preparation before your first dose is essential for a smooth initiation of GLP-1 therapy. Ensure you have received proper training from your healthcare team on injection technique, including site rotation (typically abdomen, thigh, or upper arm), needle disposal, and pen device operation. Most GLP-1 medications require refrigeration before first use, with product-specific room temperature storage limits after opening (e.g., Ozempic: 6 weeks; Trulicity: 14 days; Wegovy: 28 days). Check your specific product's SmPC or patient information leaflet for storage requirements.
Timing your first dose should account for several practical factors:
-
Dietary planning: Consider starting when you can maintain a regular eating pattern and have access to light, easily digestible meals, as gastrointestinal side effects are most common initially
-
Monitoring capability: Choose a time when you can observe your body's response and have access to medical advice if needed
-
Social calendar: Avoid starting immediately before important events, travel, or periods of high stress
-
Support availability: Begin when family members or carers are available to assist if you experience side effects
Dose escalation protocols are standard with GLP-1 therapy to minimise adverse effects. Treatment typically begins at a low dose, with gradual increases according to product-specific schedules. For example:
-
Semaglutide for diabetes (Ozempic): Start at 0.25 mg weekly for 4 weeks, increase to 0.5 mg, then potentially to 1 mg or 2 mg at 4-week intervals
-
Semaglutide for weight management (Wegovy): Start at 0.25 mg weekly, increasing through 0.5 mg, 1.0 mg, 1.7 mg to 2.4 mg at approximately 4-week intervals
-
Liraglutide for weight management (Saxenda): Start at 0.6 mg daily, increasing by 0.6 mg increments weekly to a target of 3.0 mg daily
This titration schedule is evidence-based and should not be accelerated without medical supervision. Never switch between different GLP-1 products or adjust doses without consulting your prescriber.
Medication interactions should be reviewed before starting. GLP-1 receptor agonists can delay gastric emptying, potentially affecting the absorption of oral medications. If you take other diabetes medications, particularly insulin or sulfonylureas, dose adjustments may be necessary to prevent hypoglycaemia. If you take warfarin, more frequent INR monitoring may be needed initially. Most oral contraceptives are not significantly affected by semaglutide. If you drive and are taking GLP-1 therapy with insulin or sulfonylureas, be aware of hypoglycaemia risk and follow DVLA guidance. Inform your prescriber of all medications, including over-the-counter products and supplements.
Managing Side Effects When Beginning GLP-1 Therapy
Gastrointestinal side effects are very common when initiating GLP-1 receptor agonist therapy. These typically include nausea, vomiting, diarrhoea, constipation, and abdominal discomfort. The symptoms are usually most pronounced during the first few weeks of treatment and following dose increases, generally improving as your body adapts to the medication.
Strategies to minimise nausea and gastrointestinal upset include:
-
Dietary modifications: Eat smaller, more frequent meals rather than large portions; avoid high-fat, greasy, or heavily spiced foods; stay well-hydrated with small sips of water throughout the day
-
Meal timing: Allow adequate time between eating and lying down; avoid eating close to bedtime
-
Ginger and bland foods: Some patients find ginger tea or bland foods (toast, crackers, rice) helpful during episodes of nausea
-
Slow eating: Chew food thoroughly and eat slowly to reduce gastric distress
If nausea is severe or persistent, contact your GP or diabetes specialist nurse. Anti-emetic medications may be prescribed temporarily, or your dose escalation schedule may be slowed. Do not discontinue the medication without medical advice, as symptoms often improve with continued use.
Other potential side effects to be aware of include injection site reactions (redness, itching, or swelling), headache, fatigue, and dizziness. These are generally mild and self-limiting. More serious but rare adverse effects include pancreatitis, gallbladder problems, and changes in vision. If you have pre-existing diabetic retinopathy, rapid improvements in blood glucose with semaglutide may temporarily worsen your condition, so report any visual changes promptly.
When to seek urgent medical attention:
-
Severe, persistent abdominal pain that does not resolve (if pancreatitis is suspected, stop taking the medication and seek immediate medical assessment)
-
Signs of dehydration from persistent vomiting or diarrhoea (which can lead to acute kidney injury)
-
Allergic reactions (rash, difficulty breathing, swelling of face or throat)
-
Symptoms of hypoglycaemia if taking other glucose-lowering medications (shakiness, confusion, sweating)
Regular follow-up with your healthcare team is essential to monitor your response to treatment, adjust doses appropriately, and address any concerns promptly. Report any suspected side effects to your healthcare professional and consider using the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
What to Expect in Your First Week on GLP-1
During the initial days of GLP-1 therapy, most patients notice relatively subtle changes, as the medication requires time to reach therapeutic levels and exert its full effects. You may experience a mild reduction in appetite within the first few days, though significant weight loss typically does not occur immediately. Clinically meaningful weight loss usually develops over weeks to months, often becoming more noticeable after reaching higher maintenance doses. Some patients report feeling fuller more quickly during meals or experiencing reduced cravings for certain foods, particularly high-fat or sweet items.
Gastrointestinal adjustment is common in the first week. You may notice changes in bowel habits, mild nausea (particularly after meals), or a sensation of fullness that persists longer than usual. These effects are generally most noticeable in the first 3–5 days and often improve as your body adapts. Maintaining adequate hydration and following the dietary strategies mentioned previously can help manage these symptoms.
Blood glucose changes, if you have diabetes, may begin within the first week, though optimal glycaemic control typically develops over several weeks. If you are monitoring your blood glucose at home, continue your usual testing schedule and record your results according to your diabetes care plan. If you experience hypoglycaemia (blood glucose below 4 mmol/L), treat it promptly with 15-20g of fast-acting carbohydrate (e.g., glucose tablets, fruit juice), recheck after 15 minutes, and follow with a longer-acting carbohydrate if your next meal is not due soon. Report any episodes to your healthcare team, particularly if you are taking other diabetes medications that may require dose adjustment.
Energy levels and daily activities can usually be maintained normally during your first week on GLP-1 therapy. However, if you experience significant nausea or fatigue, it is reasonable to avoid strenuous exercise or demanding activities until symptoms settle. Gentle physical activity, such as walking, is generally well-tolerated and may help with any gastrointestinal discomfort.
Monitoring and follow-up should be arranged according to your healthcare team's recommendations. Keep a symptom diary noting any side effects, changes in appetite, and blood glucose readings if applicable. Contact your GP or diabetes specialist nurse if you have concerns about side effects, are unable to tolerate the medication, or experience any warning signs requiring medical attention. Most patients find that any initial discomfort is manageable and improves significantly after the first 1–2 weeks, with the therapeutic benefits becoming more apparent over the following months.
Frequently Asked Questions
Can I start GLP-1 therapy on any day of the week?
Yes, there is no medical contraindication to starting GLP-1 therapy on any particular day. The decision should be based on your personal schedule and when you feel most prepared to manage potential side effects.
What should I do if I miss my weekly GLP-1 injection?
For semaglutide, take the missed dose within 5 days of the scheduled time; if more than 5 days have passed, skip that dose and resume your normal schedule. For dulaglutide, take the missed dose if there are at least 3 days until your next scheduled dose.
How long does it take for GLP-1 side effects to improve?
Gastrointestinal side effects such as nausea are typically most pronounced during the first few weeks and following dose increases, generally improving as your body adapts to the medication over 1–2 weeks.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript