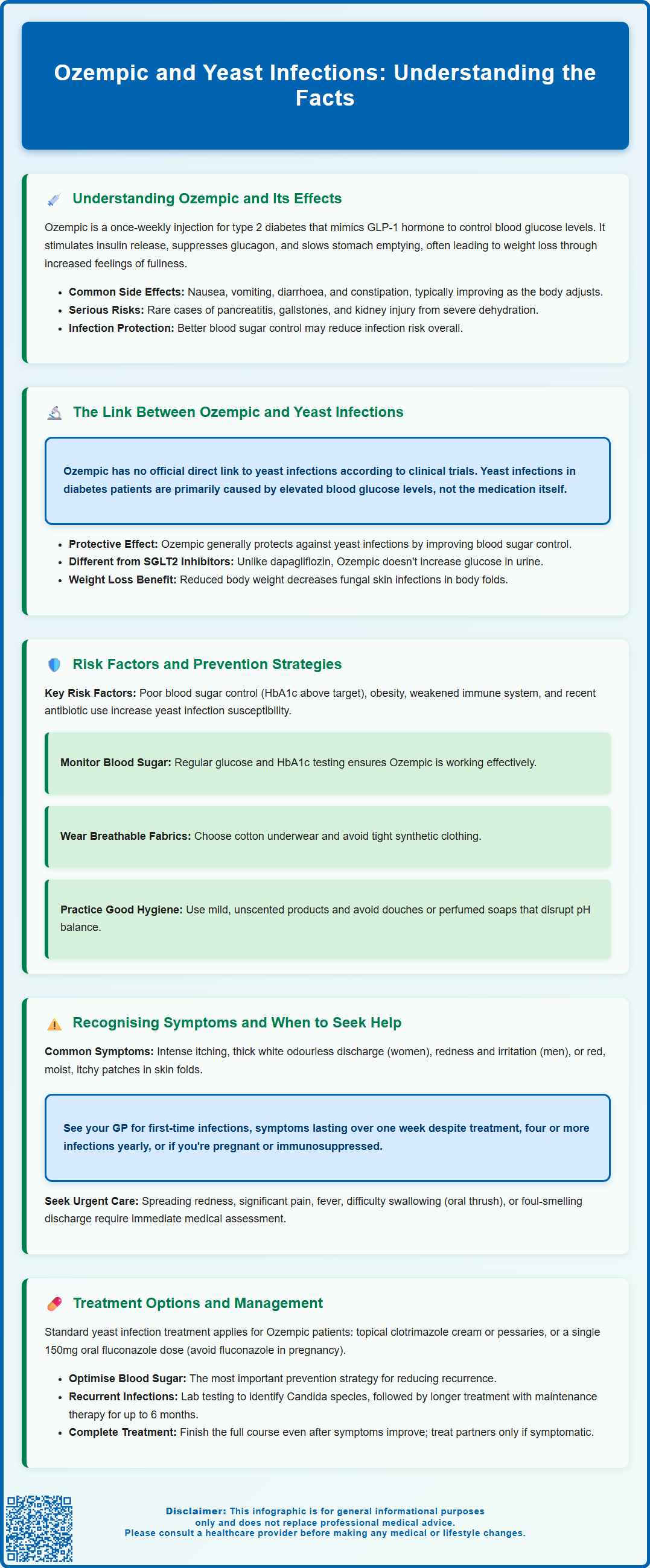
Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for managing type 2 diabetes mellitus. Whilst patients may be concerned about ozempic and yeast infections, there is no established direct link between this medication and increased candidiasis risk. Unlike SGLT2 inhibitors, which are associated with genital fungal infections, Ozempic typically improves glycaemic control, potentially reducing infection susceptibility. Understanding the relationship between diabetes medications and yeast infections helps patients make informed decisions about their treatment and recognise when preventive measures or medical advice may be needed.
Summary: Ozempic does not directly cause yeast infections and may actually reduce risk by improving blood glucose control in type 2 diabetes patients.
- Ozempic is a GLP-1 receptor agonist licensed for type 2 diabetes, not associated with increased candidiasis risk in clinical trials or regulatory guidance.
- Improved glycaemic control from Ozempic typically reduces yeast infection susceptibility, unlike SGLT2 inhibitors which increase genital mycotic infection risk.
- Poorly controlled diabetes creates glucose-rich environments conducive to Candida growth in bodily fluids and skin folds.
- Prevention focuses on optimising HbA1c levels, maintaining personal hygiene, wearing breathable clothing, and monitoring blood glucose regularly.
- Recurrent yeast infections despite good glycaemic control warrant GP review and possible further investigation of diabetes management.
Table of Contents
Understanding Ozempic and Its Effects on the Body
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Administered as a once-weekly subcutaneous injection, it works by mimicking the action of the naturally occurring hormone GLP-1, which plays a crucial role in glucose regulation and appetite control.
The mechanism of action of Ozempic involves several physiological processes. It stimulates insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning insulin is released only when blood glucose levels are elevated. Simultaneously, it suppresses glucagon secretion, reducing hepatic glucose production. Additionally, Ozempic slows gastric emptying, which helps to moderate post-prandial glucose spikes and promotes satiety, often leading to weight loss—a beneficial effect for many patients with type 2 diabetes.
Common adverse effects associated with Ozempic include gastrointestinal symptoms such as nausea, vomiting, diarrhoea, and constipation, particularly during the initial titration phase. These effects typically diminish over time as the body adjusts to the medication. Other side effects may include injection site reactions. Serious adverse effects, though rare, may include pancreatitis, diabetic retinopathy complications, hypoglycaemia when used with other glucose-lowering agents, cholelithiasis (gallstones), and dehydration or acute kidney injury associated with severe gastrointestinal symptoms.
Understanding how Ozempic affects metabolic processes is essential when considering its broader impact on health, including potential influences on infection susceptibility. The medication's effect on blood glucose control is particularly relevant, as elevated glucose levels can create an environment conducive to certain types of infections, including fungal overgrowth.
It's important to note that while Ozempic may lead to weight loss, it is licensed specifically for type 2 diabetes management. Semaglutide for weight management is marketed as Wegovy in the UK.
If you experience any suspected side effects, report them to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or via the Yellow Card app).
The Link Between Ozempic and Yeast Infections
The relationship between Ozempic and yeast infections is not straightforward, and there is no official direct link established in clinical trials or regulatory guidance from the MHRA or EMA. Ozempic is not known to directly increase the risk of candidiasis according to its product information.
Yeast infections, most commonly caused by Candida albicans, thrive in environments with elevated glucose levels. Patients with poorly controlled diabetes are at increased risk of candidal infections, particularly vulvovaginal candidiasis in women and balanitis in men. The primary connection between diabetes medications and yeast infections relates to glycaemic control rather than the medication itself. When blood glucose levels remain elevated despite treatment, the excess glucose in bodily fluids—including urine, vaginal secretions, and skin moisture—creates an ideal environment for fungal proliferation.
Ozempic's role in this context is generally protective rather than causative. By improving glycaemic control and reducing HbA1c levels, Ozempic should theoretically decrease the risk of yeast infections compared to poorly controlled diabetes. However, during the initial treatment period or dose adjustments, some patients may experience fluctuations in blood glucose levels that could temporarily affect infection susceptibility.
It's important to distinguish GLP-1 receptor agonists like Ozempic from another class of diabetes medications—SGLT2 inhibitors (such as dapagliflozin, empagliflozin, and canagliflozin). SGLT2 inhibitors are associated with an increased risk of genital mycotic infections due to their mechanism of action, which increases glucose excretion in the urine. This is not the case with GLP-1 receptor agonists like Ozempic.
Excess weight can increase the risk of fungal infections in skin folds (intertrigo), and weight loss generally helps reduce this risk by decreasing skin-fold moisture and friction.
Risk Factors and Prevention Strategies
Several risk factors increase the likelihood of developing yeast infections whilst taking Ozempic or any diabetes medication. The most significant factor remains suboptimal glycaemic control—patients with HbA1c levels above target are at substantially higher risk. Other predisposing factors include obesity, immunosuppression, antibiotic use, pregnancy, tight-fitting synthetic clothing, and poor personal hygiene practices.
For patients taking Ozempic, prevention strategies should focus on optimising diabetes management and maintaining good general health practices. Regular monitoring of blood glucose levels and HbA1c is essential to ensure the medication is achieving its therapeutic goals. Patients should work closely with their diabetes care team to adjust dosing appropriately and address any persistent hyperglycaemia.
Practical prevention measures include:
-
Maintaining excellent personal hygiene, particularly in the genital area, using mild, unscented products
-
Avoiding perfumed soaps, shower gels, and douches; consider using an emollient as a soap substitute
-
Wearing breathable, cotton underwear and avoiding tight-fitting synthetic clothing
-
Changing out of damp clothing (such as swimwear or exercise attire) promptly
-
Using antibiotics only when prescribed and clinically indicated
-
Focusing on achieving good overall glycaemic control through diet, exercise and medication
-
Staying well-hydrated to support overall health and immune function
-
Managing weight through diet and exercise, as recommended by healthcare providers
For women specifically, avoiding scented feminine hygiene products and prolonged use of panty liners can help maintain the natural vaginal pH and microbiome.
If recurrent infections occur despite good glycaemic control and preventive measures, further investigation may be warranted. This should include a review of diabetes control and consideration of diabetes testing in those not previously diagnosed, particularly in men with recurrent balanitis.
Recognising Symptoms and When to Seek Medical Advice
Recognising the symptoms of yeast infections early enables prompt treatment and prevents complications. Vulvovaginal candidiasis typically presents with intense itching and irritation of the vulva and vagina, accompanied by a thick, white, cottage cheese-like discharge that is usually odourless. Patients may also experience soreness, redness, swelling of the vulval tissues, and discomfort during urination or sexual intercourse. In men, candidal balanitis manifests as redness, itching, and irritation of the glans penis, sometimes with a white discharge beneath the foreskin.
Cutaneous candidiasis, which can occur in skin folds (particularly in patients with obesity), presents as red, moist, itchy patches with satellite lesions at the periphery. Common sites include under the breasts, in the groin, between the buttocks, and in abdominal folds. Oral thrush appears as white patches on the tongue, inner cheeks, or throat, often accompanied by soreness. Difficulty swallowing or pain on swallowing with oral thrush is a red flag requiring urgent assessment, especially in those who are immunosuppressed.
When to contact your GP:
-
First episode of suspected yeast infection requiring diagnosis confirmation
-
Symptoms persisting beyond one week despite over-the-counter treatment
-
Recurrent infections (four or more episodes within 12 months)
-
Severe symptoms including extensive redness, swelling, or skin breakdown
-
Unusual discharge with an offensive odour (suggesting bacterial rather than fungal infection)
-
Pregnancy or immunosuppression
-
Uncertainty about the diagnosis
Consider attending a sexual health clinic if you have risk factors for sexually transmitted infections or atypical discharge.
Seek urgent medical attention if you develop signs of severe infection or alternative diagnoses, including spreading redness, significant pain, fever, or if you feel generally unwell. Contact NHS 111 for urgent advice or attend an urgent treatment centre or A&E if severely unwell.
Patients taking Ozempic who experience recurrent yeast infections despite good glycaemic control should discuss this with their diabetes care team, as it may indicate the need for additional investigation or adjustment to their diabetes management plan.
Treatment Options and Management
Treatment for yeast infections in patients taking Ozempic follows standard antifungal protocols, with the primary goal of eradicating the infection whilst optimising diabetes control to prevent recurrence. For uncomplicated vulvovaginal candidiasis, first-line treatment typically involves topical azole antifungals such as clotrimazole pessaries or cream, available over the counter from pharmacies. A single dose of oral fluconazole 150mg is an effective alternative and may be preferred by some patients for convenience.
Important cautions:
-
Oral fluconazole should be avoided in pregnancy; topical azoles should be used for at least 7 days instead
-
Consult your pharmacist or GP about potential drug interactions, particularly if you take warfarin or other medications
For male genital candidiasis, topical clotrimazole cream applied twice daily for one to two weeks is usually sufficient. Cutaneous candidiasis in skin folds responds well to topical antifungal creams (such as clotrimazole or miconazole) combined with measures to keep the affected areas dry. In more extensive or resistant cases, oral antifungal therapy may be necessary.
For patients with recurrent vulvovaginal candidiasis (four or more episodes annually), management should include:
-
Microscopy and culture to identify the Candida species
-
An induction-maintenance regimen (e.g., fluconazole 150mg every 72 hours for three doses, followed by weekly maintenance for up to six months)
-
Thorough review of predisposing factors
Management strategies for patients on Ozempic should include:
-
Optimising glycaemic control as the cornerstone of prevention—reviewing HbA1c targets and adjusting diabetes medications as needed
-
Completing the full course of antifungal treatment even if symptoms resolve early
-
Treating sexual partners if they have symptoms (though routine partner treatment is not necessary for uncomplicated cases)
-
Reviewing and addressing modifiable risk factors
-
Considering prophylactic antifungal therapy for patients with frequent recurrences
Patients should be reassured that yeast infections, whilst uncomfortable, are treatable and that continuing Ozempic is appropriate provided diabetes control is optimised. However, if infections persist despite adequate treatment and good glycaemic control, further investigation for azole-resistant Candida or non-albicans Candida species may be warranted. If recurrent genital thrush persists, review any concomitant SGLT2 inhibitor therapy, as these medications (unlike GLP-1 receptor agonists) are associated with increased risk of genital mycotic infections.
Regular follow-up with the diabetes care team ensures that both the diabetes and any recurrent infections are managed effectively, maintaining overall health and quality of life.
Frequently Asked Questions
Does Ozempic increase the risk of yeast infections?
No, Ozempic does not directly increase yeast infection risk. By improving blood glucose control in type 2 diabetes, it may actually reduce susceptibility to candidiasis compared to poorly controlled diabetes.
How is Ozempic different from SGLT2 inhibitors regarding infection risk?
Unlike SGLT2 inhibitors (such as dapagliflozin or empagliflozin), which increase glucose in urine and are associated with genital mycotic infections, Ozempic works through a different mechanism and does not carry this specific risk.
When should I see my GP about yeast infections whilst taking Ozempic?
Contact your GP if you experience your first suspected yeast infection, symptoms persisting beyond one week despite treatment, recurrent infections (four or more annually), or if you have severe symptoms, pregnancy, or immunosuppression.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript