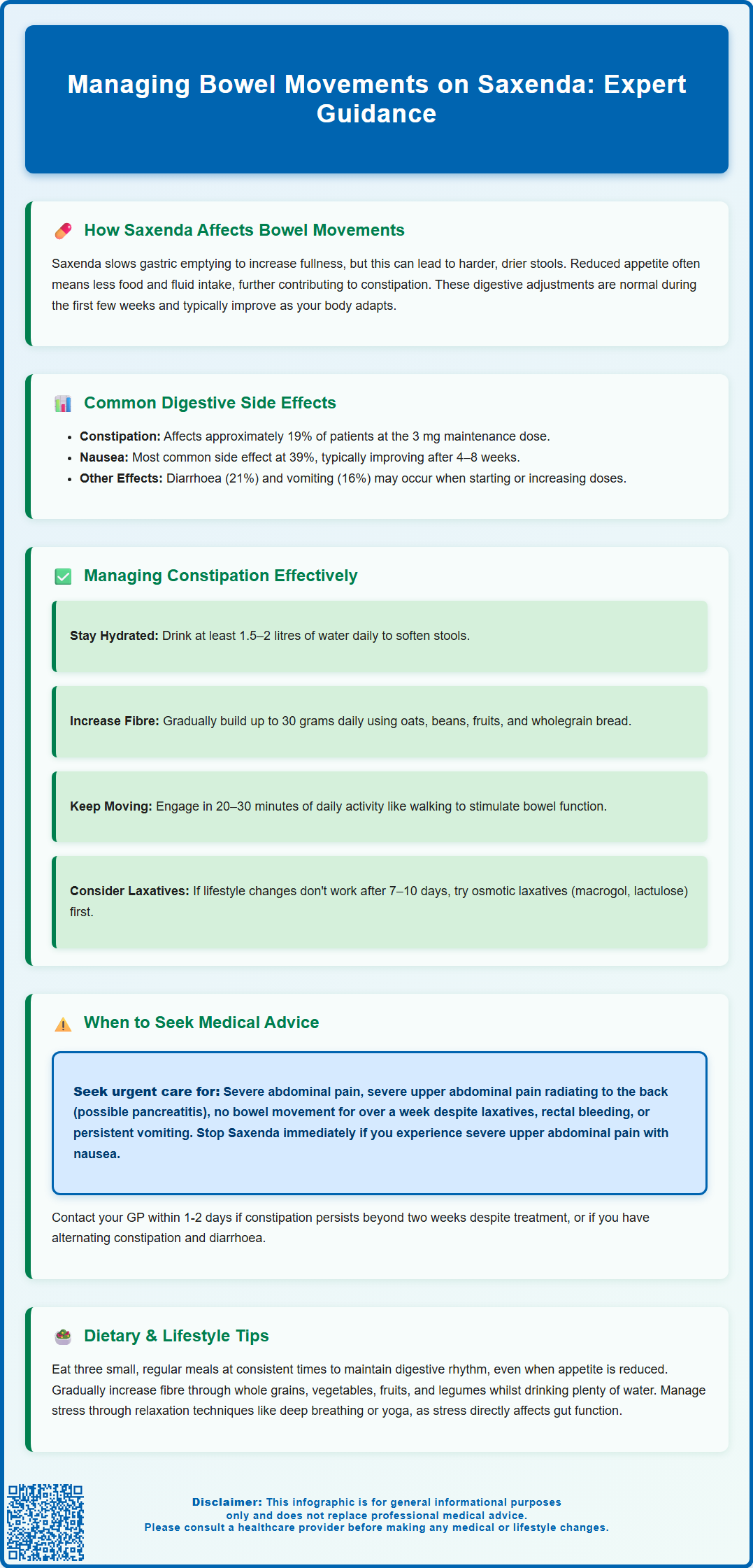
Saxenda (liraglutide) is a GLP-1 receptor agonist licensed in the UK for weight management in adults and adolescents with obesity. Whilst effective for weight loss, Saxenda commonly affects bowel function, with constipation reported in approximately 19% of patients. Understanding how this medication influences digestion—and implementing practical strategies to maintain regular bowel movements—can significantly improve treatment comfort and adherence. This article explores the mechanisms behind Saxenda-related bowel changes, common digestive side effects, evidence-based management approaches, and when to seek medical advice.
Summary: Saxenda (liraglutide) commonly causes constipation by slowing gastric emptying, which can be managed through increased hydration, dietary fibre, physical activity, and laxatives if needed.
- Saxenda is a GLP-1 receptor agonist that slows gastric emptying, contributing to constipation in approximately 19% of patients.
- Management includes drinking 1.5–2 litres of water daily, gradually increasing fibre to 30 grams, and regular physical activity.
- Osmotic laxatives (macrogol, lactulose) are first-line pharmacological treatment if conservative measures fail after 7–10 days.
- Seek urgent medical attention for severe abdominal pain, no bowel movement for over one week, rectal bleeding, or signs of pancreatitis.
- Most gastrointestinal side effects improve after 4–8 weeks as the body adapts to Saxenda treatment.
Table of Contents
How Saxenda Affects Bowel Movements
Saxenda (liraglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for weight management in adults with a BMI ≥30 kg/m², or ≥27 kg/m² with weight-related comorbidities. It is also licensed for weight management in adolescents aged 12 years and above with obesity. Understanding how this medication affects your digestive system is essential for managing expectations and maintaining comfort during treatment.
The mechanism by which Saxenda influences bowel function relates directly to its pharmacological action. Liraglutide works by mimicking the natural hormone GLP-1, which primarily slows gastric emptying—the rate at which food moves from your stomach into your small intestine. This delayed emptying, which occurs via effects on vagal and enteric neural pathways, contributes to increased satiety and reduced appetite, which are central to the medication's weight-loss effects. This same mechanism can impact bowel movements, though this effect may attenuate somewhat with continued treatment.
When gastric emptying slows, the digestive process becomes more gradual. Food remains in the stomach longer, which can affect overall gut transit time. This can result in harder, drier stools that are more difficult to pass. Additionally, as Saxenda reduces appetite, many patients naturally consume less food and fluid, which can further contribute to constipation.
It is important to recognise that these effects are a direct pharmacological consequence of how Saxenda works rather than an indication that the medication is unsuitable. Most patients experience some degree of digestive adjustment during the initial weeks of treatment, with symptoms often improving as the body adapts to the medication. Saxenda is not generally recommended for people with severe gastrointestinal disease, such as gastroparesis.
Common Digestive Side Effects of Saxenda
Gastrointestinal side effects are among the most frequently reported adverse reactions to Saxenda, affecting a substantial proportion of patients, particularly during dose escalation. According to clinical trial data and the Summary of Product Characteristics, constipation affects approximately 19% of patients taking the 3 mg maintenance dose.
The most common digestive side effects include:
-
Nausea (affecting approximately 39% of patients)—often the most prominent symptom during the first few weeks
-
Constipation (19%)—characterised by infrequent bowel movements, straining, or hard stools
-
Diarrhoea (21%)—some patients experience loose stools rather than constipation
-
Vomiting (16%)—particularly during dose escalation
-
Abdominal discomfort or bloating—related to delayed gastric emptying
-
Dyspepsia—indigestion or upper abdominal discomfort
-
Flatulence—increased gas production
These effects typically emerge or intensify when starting Saxenda or increasing the dose. The medication is initiated at 0.6 mg daily and gradually increased weekly to the maintenance dose of 3.0 mg daily. This titration schedule is specifically designed to minimise gastrointestinal side effects by allowing the digestive system time to adapt.
Most patients find that nausea and other digestive symptoms improve significantly after the first 4–8 weeks of treatment. However, constipation may persist throughout treatment if not actively managed. It is worth noting that whilst these side effects are common, they do not affect everyone equally. Some patients experience minimal digestive disruption, whilst others require specific management strategies.
Saxenda can also increase the risk of gallbladder problems such as gallstones, particularly during rapid weight loss. The severity of digestive symptoms does not correlate with the medication's effectiveness for weight loss. If digestive side effects become intolerable, your prescriber may recommend slowing the dose escalation or implementing additional management strategies before considering discontinuation.
Managing Constipation While Taking Saxenda
Proactive management of constipation whilst taking Saxenda can significantly improve comfort and treatment adherence. A structured, stepwise approach is recommended, beginning with conservative measures before considering pharmacological interventions.
Hydration is the cornerstone of constipation management. Aim for at least 1.5–2 litres of water daily, increasing this amount if you exercise or in warm weather. Adequate fluid intake helps soften stools and facilitates their passage through the intestines. Many patients on Saxenda inadvertently reduce their fluid intake alongside reduced food consumption, compounding constipation risk. If you have heart or kidney disease with fluid restrictions, consult your healthcare provider before increasing fluid intake.
Dietary fibre should be gradually increased to around 30 grams daily, as recommended in the UK. Soluble fibre sources include oats, beans, lentils, and fruits such as apples and pears. Insoluble fibre from wholegrain bread, brown rice, and vegetables adds bulk to stools. Introduce fibre slowly to avoid bloating and ensure you maintain adequate hydration, as fibre requires water to function effectively.
Physical activity stimulates intestinal motility. Even modest increases in activity—such as a daily 20–30 minute walk—can promote regular bowel function. Exercise also supports the weight-loss goals of Saxenda treatment.
If conservative measures prove insufficient after 7–10 days, over-the-counter laxatives may be appropriate:
-
Osmotic laxatives (macrogol, lactulose)—often first-line pharmacological treatment; macrogols typically work within 1–3 days, lactulose within 24–48 hours
-
Stimulant laxatives (senna, bisacodyl)—may be added if osmotic laxatives are insufficient; work within 6–12 hours
-
Bulk-forming laxatives (ispaghula husk, methylcellulose)—can be helpful but require adequate fluid intake; work within 2–3 days
Establish a regular toilet routine, allowing adequate time after meals when the gastrocolic reflex naturally stimulates bowel activity. Avoid ignoring the urge to defaecate, as this can worsen constipation. If symptoms persist beyond two weeks despite these interventions, consult your GP or prescribing clinician for further assessment.
When to Seek Medical Advice About Bowel Changes
Whilst constipation is a recognised side effect of Saxenda, certain symptoms warrant prompt medical evaluation to exclude more serious conditions or complications. Understanding when self-management is appropriate versus when professional assessment is needed ensures patient safety.
Seek urgent medical attention (contact 111 or attend A&E) if you experience:
-
Severe abdominal pain—particularly if constant, worsening, or accompanied by vomiting
-
Severe upper abdominal pain radiating to the back—may indicate pancreatitis; stop taking Saxenda immediately and seek urgent medical care
-
No bowel movement for more than one week despite laxative use
-
Rectal bleeding—blood in stools or on toilet paper
-
Persistent vomiting—inability to keep down fluids, which may lead to dehydration
-
Signs of bowel obstruction—severe bloating, inability to pass wind, vomiting faecal-smelling material
-
Right upper abdominal pain with fever or yellowing of skin/eyes—may indicate gallbladder problems
Contact your GP within 1–2 days if you notice:
-
Constipation persisting beyond two weeks despite appropriate management
-
Unexplained weight loss beyond expected Saxenda effects
-
Change in bowel habit with alternating constipation and diarrhoea
-
Persistent abdominal bloating or discomfort affecting daily activities
-
New or worsening symptoms after several months of stable treatment
-
Signs of dehydration (dark urine, dizziness, reduced urination) with ongoing diarrhoea or vomiting
It is particularly important to differentiate between expected medication side effects and symptoms that might indicate other gastrointestinal conditions. Saxenda can, rarely, cause pancreatitis—characterised by severe upper abdominal pain radiating to the back, often with nausea and vomiting. If you suspect pancreatitis, stop taking Saxenda immediately and seek urgent medical assessment.
Patients with pre-existing gastrointestinal conditions, such as inflammatory bowel disease or previous bowel surgery, should have a lower threshold for seeking advice. Similarly, if you are taking other medications that affect bowel function (such as opioid analgesics or certain antidepressants), discuss potential interactions with your prescriber. Regular follow-up appointments with your prescribing clinician provide opportunities to review bowel function and adjust management strategies as needed.
If you experience side effects from Saxenda, you can report them directly to the MHRA Yellow Card Scheme at yellowcard.mhra.gov.uk or via the Yellow Card app.
Dietary and Lifestyle Tips for Regular Bowel Function on Saxenda
Optimising your diet and lifestyle whilst taking Saxenda not only supports regular bowel function but also enhances the medication's weight-loss efficacy and improves overall wellbeing. A holistic approach addresses multiple factors influencing digestive health.
Structured meal timing helps regulate bowel patterns. Despite reduced appetite, aim for three small, regular meals daily rather than skipping meals entirely. This maintains digestive rhythm and stimulates the gastrocolic reflex. Eating at consistent times trains your bowel to function predictably.
Fibre-rich food choices should be incorporated thoughtfully:
-
Breakfast: porridge with berries and ground flaxseed; wholegrain toast
-
Lunch and dinner: include vegetables or salad with each meal; choose brown rice, wholemeal pasta, or quinoa
-
Snacks: fresh fruit, raw vegetables with hummus, a small handful of nuts
-
Legumes: beans, lentils, and chickpeas are excellent fibre sources that also provide protein
Remember to increase fibre gradually and maintain adequate fluid intake to prevent bloating or worsening constipation.
Probiotic foods may support digestive health, though evidence specifically for Saxenda-related constipation is limited. Natural yoghurt, kefir, sauerkraut, and other fermented foods contribute to a healthy gut microbiome.
Mindful eating practices are particularly valuable on Saxenda. Eat slowly, chewing thoroughly, which aids digestion and helps you recognise satiety signals. Avoid eating late in the evening, allowing at least 2–3 hours between your last meal and bedtime.
Stress management influences gut function through the gut-brain axis. Chronic stress can exacerbate constipation. Consider relaxation techniques such as deep breathing exercises, yoga, or meditation.
Sleep hygiene affects digestive function. Aim for 7–9 hours of quality sleep nightly, maintaining consistent sleep and wake times. Poor sleep can disrupt hormones that influence appetite and digestion.
Limit constipating foods where possible: excessive red meat, processed foods, refined carbohydrates, and high-fat foods can slow transit time. Moderate caffeine and alcohol intake, as both can contribute to dehydration. By integrating these dietary and lifestyle modifications, most patients can maintain comfortable bowel function throughout Saxenda treatment whilst achieving their weight-management goals.
Scientific References
- Saxenda 6 mg/mL solution for injection in pre-filled pen - Summary of Product Characteristics.
- Liraglutide for managing overweight and obesity. Technology Appraisal TA664.
- Saxenda: EPAR - Public assessment report.
- GLP-1 receptor agonists: reminder of the potential side effects and to be aware of the potential for misuse.
Frequently Asked Questions
Why does Saxenda cause constipation?
Saxenda slows gastric emptying by mimicking the natural GLP-1 hormone, which delays food movement through the digestive system and can result in harder, drier stools. Reduced appetite and fluid intake on Saxenda further contribute to constipation.
What laxatives are safe to use with Saxenda?
Osmotic laxatives such as macrogol or lactulose are typically first-line treatment for Saxenda-related constipation. Stimulant laxatives (senna, bisacodyl) may be added if osmotic laxatives prove insufficient, and bulk-forming laxatives can be helpful with adequate fluid intake.
When should I contact my doctor about bowel problems on Saxenda?
Seek urgent medical attention for severe abdominal pain (especially radiating to the back), no bowel movement for over one week despite laxatives, rectal bleeding, or persistent vomiting. Contact your GP within 1–2 days if constipation persists beyond two weeks despite management or if you experience unexplained symptoms.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript