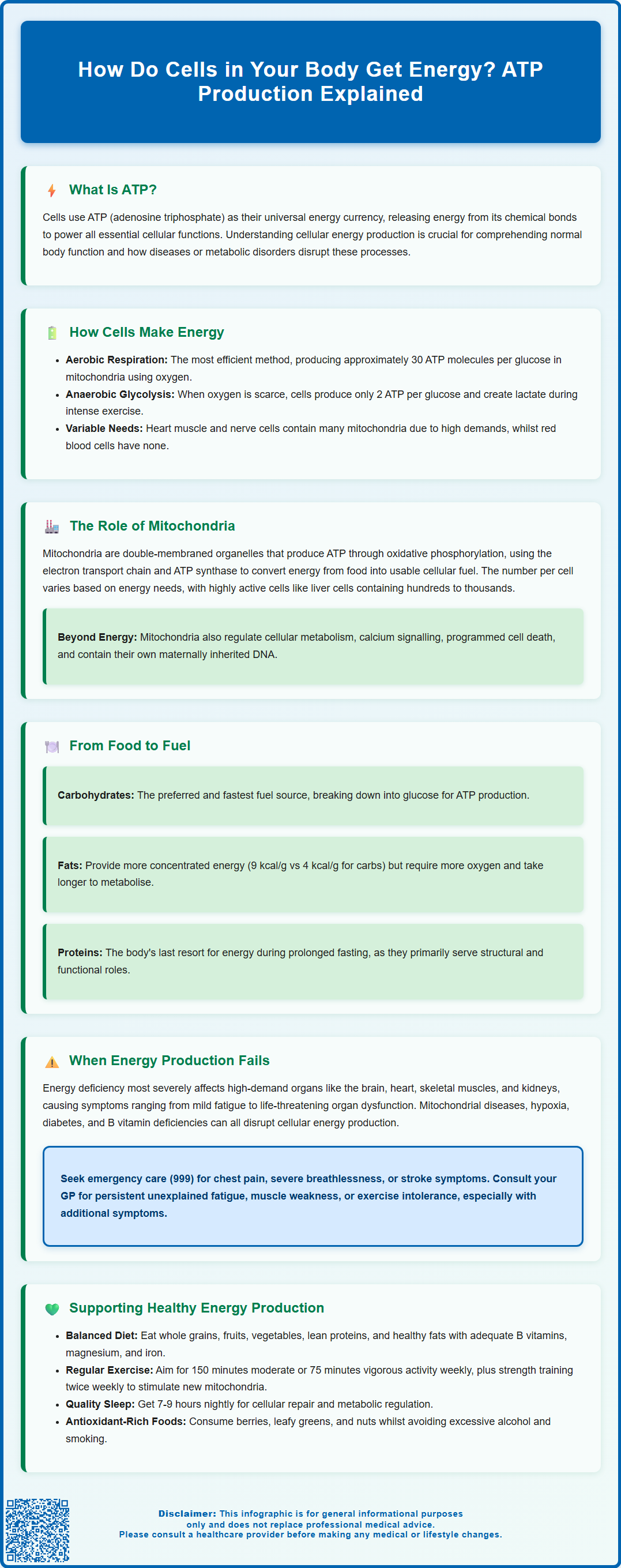
Every cell in your body requires energy to function, from contracting muscles to transmitting nerve signals. This energy comes primarily from adenosine triphosphate (ATP), produced through cellular respiration in structures called mitochondria. By breaking down nutrients—especially glucose from carbohydrates—in the presence of oxygen, cells generate the ATP needed for life. When oxygen is limited, cells can use less efficient anaerobic pathways. Understanding how cells produce energy is fundamental to appreciating normal body function and recognising when metabolic disorders disrupt these vital processes.
Summary: Cells in your body get energy primarily by producing ATP through cellular respiration in mitochondria, breaking down glucose and other nutrients in the presence of oxygen.
- ATP (adenosine triphosphate) is the universal energy currency that powers all cellular processes including muscle contraction and nerve transmission.
- Mitochondria carry out oxidative phosphorylation, the most efficient energy-producing process, generating approximately 30 ATP molecules per glucose molecule.
- When oxygen is limited, cells use anaerobic glycolysis, producing only 2 ATP molecules per glucose but allowing continued function during intense exercise.
- Carbohydrates, fats, and proteins all contribute to energy production through distinct metabolic pathways coordinated by the liver.
- Mitochondrial dysfunction, hypoxia, metabolic disorders, and nutritional deficiencies can impair cellular energy production, particularly affecting high-demand organs like the brain and heart.
- Persistent unexplained fatigue warrants GP consultation for baseline investigations including full blood count, thyroid function, and blood glucose testing.
Table of Contents
How Do Cells in Your Body Get Energy?
Every cell in your body requires a constant supply of energy to perform essential functions, from muscle contraction and nerve signal transmission to protein synthesis and cell division. This energy is derived primarily through a molecule called adenosine triphosphate (ATP), often described as the universal energy currency of cells. ATP stores energy in its chemical bonds, and when these bonds are broken, energy is released to power cellular processes.
The production of ATP occurs through several interconnected metabolic pathways, with the most efficient being cellular respiration. This process takes place predominantly in specialised structures within cells called mitochondria. Cellular respiration involves breaking down nutrients—primarily glucose from carbohydrates—in the presence of oxygen to generate ATP. A single glucose molecule can yield around 30 ATP molecules through complete aerobic respiration, though this varies by cell type and metabolic conditions.
When oxygen is limited or unavailable, cells can also produce energy through anaerobic glycolysis, though this is far less efficient, generating only 2 ATP molecules per glucose molecule. This pathway is particularly important in muscle cells during intense exercise when oxygen demand exceeds supply, resulting in the production of lactate as a by-product.
Different cell types have varying energy requirements. For instance, cardiac muscle cells and neurons have exceptionally high energy demands and contain abundant mitochondria, whilst mature red blood cells lack mitochondria entirely and rely solely on anaerobic glycolysis. Understanding how cells generate energy is fundamental to appreciating how the body functions and what happens when these processes are disrupted by disease or metabolic disorders.
The Role of Mitochondria in Energy Production
Mitochondria are often referred to as the 'powerhouses of the cell' due to their central role in ATP production. These double-membraned organelles are present in nearly all human cells, with their numbers varying according to the cell's energy requirements. A single liver cell, for example, may contain hundreds to thousands of mitochondria, whilst less metabolically active cells contain far fewer.
The primary function of mitochondria is to carry out oxidative phosphorylation, the final and most productive stage of cellular respiration. This process occurs across the inner mitochondrial membrane and involves two key components: the electron transport chain and ATP synthase. As electrons are passed along a series of protein complexes in the electron transport chain, energy is released and used to pump hydrogen ions across the membrane, creating an electrochemical gradient. ATP synthase then harnesses this gradient to synthesise ATP from adenosine diphosphate (ADP) and inorganic phosphate.
Mitochondria also play crucial roles beyond energy production. They are involved in regulating cellular metabolism, calcium signalling, programmed cell death (apoptosis), and the production of reactive oxygen species. Interestingly, mitochondria contain their own DNA (mtDNA), which is almost exclusively maternally inherited, and this genetic material encodes some of the proteins essential for energy production.
Mitochondrial dysfunction can have profound effects on health, as impaired energy production affects high-demand tissues first, particularly the brain, heart, and muscles. Conditions such as mitochondrial myopathies, certain neurodegenerative diseases, and aspects of ageing have been linked to mitochondrial impairment. Regular physical activity and a balanced diet according to the NHS Eatwell Guide can support overall cellular function and health.
How Food Is Converted Into Cellular Energy
The conversion of food into cellular energy is a complex, multi-stage process that begins in the digestive system and culminates in ATP production within cells. The three main macronutrients—carbohydrates, fats, and proteins—each follow distinct pathways to contribute to energy production, though carbohydrates are typically the body's preferred and most readily available fuel source.
Carbohydrate metabolism begins with digestion, where complex carbohydrates are broken down into simple sugars, primarily glucose. Once absorbed into the bloodstream, glucose enters cells and undergoes glycolysis in the cytoplasm, a process that splits one glucose molecule into two pyruvate molecules, generating 2 ATP molecules and electron carriers. In the presence of oxygen, pyruvate enters the mitochondria and is converted to acetyl-CoA, which then enters the citric acid cycle (also known as the Krebs cycle). This cycle generates additional electron carriers and a small amount of ATP whilst releasing carbon dioxide as a waste product. The electron carriers then feed into the electron transport chain, where the majority of ATP is produced.
Fat metabolism provides a more concentrated energy source. Fatty acids undergo beta-oxidation in the mitochondria, breaking down into multiple acetyl-CoA molecules that enter the citric acid cycle. Whilst fat metabolism yields more ATP per gram than carbohydrates (approximately 9 kcal/g versus 4 kcal/g), the process is slower and requires more oxygen. During fasting or low carbohydrate intake, the liver produces ketone bodies that serve as alternative fuel for the brain, heart, and muscles.
Protein metabolism contributes to energy production during prolonged fasting, illness, or endurance exercise. Amino acids from proteins can be converted into intermediates that enter either glycolysis or the citric acid cycle, with nitrogen being excreted as urea. However, this is not the body's preferred energy pathway, as proteins serve primarily structural and functional roles. The liver plays a central coordinating role in managing these metabolic pathways, ensuring a steady supply of fuel to cells throughout the body according to physiological demands.
What Happens When Cells Cannot Produce Enough Energy
When cellular energy production is compromised, the effects can range from mild fatigue to life-threatening organ dysfunction, depending on the severity and tissues affected. Energy deficiency particularly impacts organs with high metabolic demands, including the brain, heart, skeletal muscles, and kidneys.
Several conditions can impair cellular energy production. Mitochondrial diseases are a group of genetic disorders affecting mitochondrial function, resulting in inadequate ATP production. Symptoms may include muscle weakness, exercise intolerance, neurological problems, cardiac dysfunction, and developmental delays. These conditions are often progressive and currently have no cure, though management focuses on symptomatic treatment and nutritional support. Patients with suspected mitochondrial disease are typically referred to specialist services via neurology or clinical genetics.
Hypoxia (insufficient oxygen supply) severely impairs aerobic respiration, forcing cells to rely on less efficient anaerobic pathways. This occurs in conditions such as chronic obstructive pulmonary disease (COPD), severe anaemia, or during cardiac arrest. Prolonged hypoxia can lead to cellular damage and tissue death, particularly in the brain and heart where oxygen demands are highest.
Metabolic disorders such as diabetes mellitus disrupt normal fuel utilisation. In poorly controlled diabetes, certain tissues cannot effectively use glucose despite its abundance in the bloodstream, leading to energy deficiency at the cellular level and compensatory breakdown of fats and proteins. Nutritional deficiencies, particularly of B vitamins (which serve as cofactors in energy metabolism), can also impair ATP production.
When to seek medical advice: NICE Clinical Knowledge Summary on tiredness/fatigue in adults advises that persistent unexplained fatigue should be investigated with baseline tests (typically including full blood count, kidney and liver function, thyroid function, blood glucose, inflammatory markers, and iron status). Call 999 immediately for chest pain, severe breathlessness, or stroke symptoms. Use NHS 111 for urgent advice. Consult your GP for persistent unexplained fatigue, muscle weakness, or exercise intolerance, particularly when accompanied by other symptoms.
Supporting Healthy Cellular Energy Production
Maintaining optimal cellular energy production involves several evidence-based lifestyle and nutritional strategies. Whilst the body's energy systems are remarkably resilient, certain practices can support metabolic health and efficiency.
Balanced nutrition forms the foundation of healthy energy metabolism. A diet rich in whole grains, fruits, vegetables, lean proteins, and healthy fats provides the macronutrients and micronutrients necessary for efficient ATP production. B vitamins (particularly B1, B2, B3, and B5) serve as essential cofactors in energy metabolism, whilst magnesium is required for ATP synthesis. Iron is crucial for oxygen transport and electron transport chain function. The NHS Eatwell Guide provides practical recommendations for achieving nutritional balance.
Regular physical activity paradoxically improves cellular energy production despite increasing immediate energy demands. Exercise stimulates mitochondrial biogenesis—the creation of new mitochondria—particularly in muscle tissue. Both aerobic exercise and resistance training have been shown to enhance metabolic flexibility. Current UK Chief Medical Officers' guidelines recommend at least 150 minutes of moderate-intensity activity or 75 minutes of vigorous-intensity activity weekly, plus muscle-strengthening activities on at least 2 days per week, and minimising sedentary time.
Adequate sleep is essential for cellular repair and metabolic regulation. During sleep, the body undergoes important restorative processes. Chronic sleep deprivation has been associated with metabolic dysfunction and impaired energy production. Adults should aim for 7–9 hours of quality sleep per night, according to NHS guidance.
Managing oxidative stress supports overall cellular health. Whilst some reactive oxygen species are normal by-products of energy production, excessive oxidative stress can damage cells. Consuming antioxidant-rich foods (berries, leafy greens, nuts) and avoiding excessive alcohol and smoking helps maintain this balance. There is no good evidence that high-dose antioxidant supplements improve energy in healthy adults, and high doses may be harmful.
If you experience persistent fatigue despite adequate sleep, nutrition, and physical activity, consult your GP to exclude underlying medical conditions such as thyroid disorders, anaemia, or chronic fatigue syndrome. Always consult a pharmacist or GP before starting any supplements, especially if you are pregnant, breastfeeding, or taking medicines. Report any suspected side effects from medicines, vaccines, or supplements via the MHRA Yellow Card Scheme.
Frequently Asked Questions
What is ATP and why is it important for cellular energy?
ATP (adenosine triphosphate) is the universal energy currency of cells, storing energy in chemical bonds that, when broken, release energy to power essential cellular processes such as muscle contraction, nerve signal transmission, and protein synthesis.
Can cells produce energy without oxygen?
Yes, cells can produce energy without oxygen through anaerobic glycolysis, though this generates only 2 ATP molecules per glucose molecule compared to approximately 30 ATP through aerobic respiration. This pathway is particularly important in muscle cells during intense exercise when oxygen supply is limited.
When should I see a GP about persistent fatigue?
Consult your GP if you experience persistent unexplained fatigue despite adequate sleep, nutrition, and physical activity, or if fatigue is accompanied by muscle weakness, exercise intolerance, or other concerning symptoms. NICE guidance recommends baseline investigations including blood tests to exclude underlying conditions such as anaemia, thyroid disorders, or diabetes.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript