Many people prescribed Ozempic (semaglutide) for type 2 diabetes wonder what physical sensations to expect during treatment. This once-weekly injectable GLP-1 receptor agonist works by mimicking natural hormones that regulate blood sugar and appetite, which means you'll likely notice changes in how your body feels—particularly regarding hunger, fullness, and digestion. Most patients experience gastrointestinal effects such as nausea, early satiety, and changes in bowel habits, especially during the initial weeks as the dose gradually increases. Understanding these sensations, knowing which are normal, and recognising when to seek medical advice helps ensure safe, effective treatment. This guide explains the physical experiences associated with Ozempic and how to manage them throughout your treatment journey.
Summary: When taking Ozempic, most patients experience gastrointestinal effects including nausea, early fullness after meals, and changes in appetite, particularly during the first 4–8 weeks as the body adjusts to the medication.
- Ozempic is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes, administered as a once-weekly subcutaneous injection with gradual dose escalation.
- The medication slows gastric emptying and acts on brain appetite centres, causing reduced hunger and increased satiety alongside its glucose-lowering effects.
- Nausea is the most common side effect (affecting more than 1 in 10 people), typically mild to moderate and improving after 4–8 weeks as tolerance develops.
- Other frequent effects include diarrhoea, constipation, abdominal discomfort, headaches, and fatigue, with intensity varying considerably between individuals.
- Seek urgent medical attention for severe persistent vomiting, signs of pancreatitis (severe abdominal pain radiating to the back), allergic reactions, or symptoms of dehydration.
- Regular monitoring by your diabetes care team ensures appropriate dose adjustments and early identification of complications such as gallbladder problems or worsening diabetic retinopathy.
Table of Contents
What Is Ozempic and How Does It Work in Your Body?
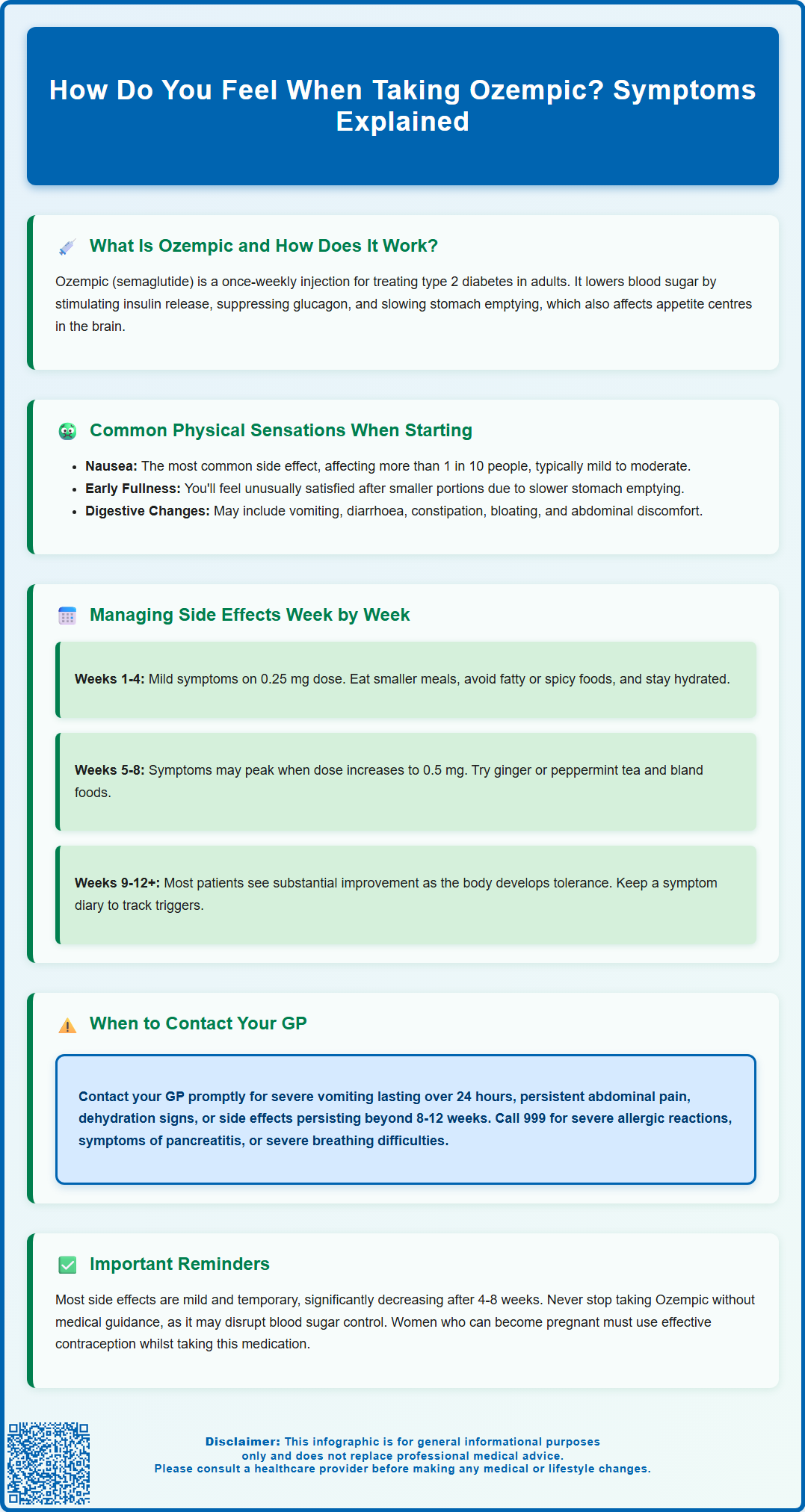
Ozempic (semaglutide) is a prescription medicine licensed in the UK specifically for the treatment of type 2 diabetes mellitus in adults. It belongs to a class of medications called glucagon-like peptide-1 (GLP-1) receptor agonists, which work by mimicking the action of a naturally occurring hormone in your body.
When you take Ozempic, the active ingredient semaglutide binds to GLP-1 receptors throughout your body, triggering several important metabolic effects. Firstly, it stimulates your pancreas to release insulin when blood glucose levels are elevated, helping to lower blood sugar in a glucose-dependent manner. Secondly, it suppresses the inappropriate secretion of glucagon (a hormone that raises blood glucose). This dual action means the medication works more actively when your blood sugar is high and reduces its effect when levels normalise, thereby lowering the risk of hypoglycaemia compared to some other diabetes medications.
Ozempic also slows gastric emptying—the rate at which food leaves your stomach and enters your small intestine. This delayed emptying contributes to increased feelings of fullness and satiety after meals, which is why many patients report changes in appetite. Additionally, the medication acts on areas of the brain involved in appetite regulation, further reducing hunger signals.
Ozempic is administered as a once-weekly subcutaneous injection, typically into the abdomen, thigh, or upper arm. The medication is gradually increased over several weeks, starting at 0.25 mg weekly for the first four weeks, then typically increasing to 0.5 mg, with potential further titration to 1 mg or 2 mg depending on glycaemic control and tolerability. This gradual dose escalation is designed to help your body adjust to the medication and minimise side effects.
It's important to note that Ozempic is not licensed for weight management (a different semaglutide product called Wegovy is approved for this purpose), nor is it suitable for type 1 diabetes. Ozempic is not recommended during pregnancy or breastfeeding, and women of childbearing potential should use effective contraception during treatment.
Common Physical Sensations When Starting Ozempic
When beginning Ozempic treatment, most patients experience some physical changes as their body adjusts to the medication. The most commonly reported sensations relate to the gastrointestinal system, reflecting the drug's mechanism of slowing gastric emptying and affecting gut motility.
Nausea is the most frequent side effect, occurring very commonly (affecting more than 1 in 10 people). This typically manifests as a mild to moderate queasiness, often most noticeable after meals or in the morning. The sensation usually improves over time as your body adapts to the medication. Alongside nausea, many patients report feeling unusually full after eating smaller portions than usual—a sensation of early satiety that can feel quite pronounced initially. Some describe this as a persistent feeling of fullness or a lack of interest in food that differs from their normal appetite patterns.
Other common gastrointestinal effects (affecting between 1 in 10 and 1 in 100 people) include vomiting, diarrhoea, constipation, abdominal pain, bloating, dyspepsia (indigestion), and eructation (belching). These varying effects reflect individual differences in how the medication affects gut motility. Some patients also report increased flatulence or changes in bowel habits during the adjustment period.
At the injection site, you may notice mild reactions such as redness, itching, or slight swelling, though these are generally minimal and resolve quickly. Headaches and fatigue are also commonly reported, typically mild and transient. It's important to stay well-hydrated while taking Ozempic, as dehydration from gastrointestinal side effects can potentially lead to acute kidney injury, particularly in those with existing kidney problems.
Less commonly, some patients may experience gallbladder problems such as gallstones or inflammation of the gallbladder. Seek medical advice if you develop pain in the upper right side of your abdomen, particularly if accompanied by fever or yellowing of the skin or eyes.
It's important to note that not everyone experiences these sensations, and their intensity varies considerably between individuals. Many patients report minimal side effects, particularly when the dose is increased gradually as recommended. These initial sensations generally diminish significantly after the first 4-8 weeks of treatment as your body adjusts to the medication.
Managing Side Effects: What to Expect Week by Week
Understanding the typical timeline of Ozempic side effects can help you prepare and manage symptoms effectively. The experience varies individually, but there are common patterns that emerge during the dose escalation period.
Weeks 1-4 (0.25 mg dose): During this initial phase, side effects are typically mild as you're on the lowest dose. You may notice subtle changes in appetite and occasional mild nausea, particularly after larger meals. This is an important adjustment period where your body begins adapting to the medication. To minimise discomfort during this phase:
-
Eat smaller, more frequent meals rather than three large meals
-
Avoid high-fat, greasy, or heavily spiced foods that may exacerbate nausea
-
Stay well-hydrated, sipping water throughout the day
-
Eat slowly and stop when you feel comfortably satisfied, not full
Weeks 5-8 (0.5 mg dose): When the dose increases, you may experience a temporary resurgence of gastrointestinal symptoms. Nausea may become more noticeable, and the feeling of fullness more pronounced. This is the period when side effects typically peak. Practical management strategies include:
-
Consider ginger or peppermint tea, which some patients find helpful for nausea
-
Avoid lying down immediately after eating
-
Choose bland, easily digestible foods if nausea is troublesome
-
Maintain adequate fibre intake to prevent constipation
-
Time your injection for a day when you can rest if needed
Weeks 9-12 and beyond: For most patients, side effects substantially improve during this period as tolerance develops. Your appetite changes may persist—this is part of the medication's therapeutic effect—but the uncomfortable sensations of nausea and bloating typically diminish. If you progress to the 1 mg or 2 mg dose, you may experience a brief recurrence of symptoms, though usually less severe than the initial dose increases.
If you're also taking sulfonylureas (like gliclazide) or insulin, your doctor may reduce these doses when starting Ozempic to minimise the risk of hypoglycaemia (low blood sugar).
Throughout treatment, keep a symptom diary noting what you eat, when symptoms occur, and their severity. This information is valuable for identifying triggers and discussing your experience with your GP or diabetes specialist nurse. If side effects remain troublesome beyond 8-12 weeks, your healthcare provider may consider adjusting your dose or exploring alternative management strategies. If you're unable to maintain adequate nutrition or hydration due to side effects, contact your healthcare provider promptly.
When to Contact Your GP About Ozempic Symptoms
Whilst most Ozempic side effects are mild and self-limiting, certain symptoms require prompt medical attention. Knowing when to seek help is crucial for your safety and ensures any serious complications are identified early.
Contact your GP or diabetes care team promptly if you experience:
-
Severe or persistent nausea and vomiting that prevents you from keeping down food or fluids for more than 24 hours, as this may lead to dehydration and potentially acute kidney injury
-
Abdominal pain, particularly if it's persistent or severe
-
Signs of dehydration including dark urine, dizziness, dry mouth, or reduced urination
-
Persistent diarrhoea lasting more than 48 hours
-
Visual changes or eye problems—particularly if you have pre-existing diabetic retinopathy, as rapid improvements in blood glucose can sometimes worsen this condition temporarily
-
Symptoms of hypoglycaemia (low blood sugar) such as trembling, sweating, confusion, or rapid heartbeat—particularly if you're taking Ozempic alongside other diabetes medications like sulphonylureas or insulin
-
Pain in the upper right side of your abdomen, especially if accompanied by fever or yellowing of the skin or eyes, which could indicate gallbladder problems
Seek immediate medical attention (call 999 or attend A&E) if you develop:
-
Severe allergic reactions including difficulty breathing, swelling of the face, lips, tongue, or throat, or severe skin rash
-
Symptoms suggesting pancreatitis: severe, persistent abdominal pain that may radiate to your back, often accompanied by nausea and vomiting—if pancreatitis is suspected, stop taking Ozempic and seek urgent medical care; if confirmed, the medication should not be restarted
-
Severe difficulty breathing or swallowing requiring immediate intervention
For other concerns, such as a lump or swelling in your neck, hoarseness, or mild difficulty swallowing without breathing problems, arrange an urgent GP appointment rather than attending A&E.
Additionally, contact your healthcare provider for routine concerns such as side effects that don't improve after 8-12 weeks, injection site reactions that worsen or don't resolve, or if you're struggling to maintain adequate nutrition due to reduced appetite. Your diabetes team can provide guidance on dose adjustments, dietary modifications, or anti-nausea medications if appropriate.
Regular monitoring through scheduled appointments allows your healthcare provider to assess your response to treatment, review your HbA1c levels, and ensure Ozempic remains appropriate and well-tolerated for your individual circumstances. Never discontinue Ozempic without consulting your prescriber, as abrupt cessation may affect your glycaemic control.
If you suspect you've experienced a side effect from Ozempic, you can report it directly to the MHRA through the Yellow Card scheme at yellowcard.mhra.gov.uk or via the Yellow Card app.
Frequently Asked Questions
Does nausea from Ozempic go away?
Yes, nausea typically improves significantly after 4–8 weeks as your body adjusts to Ozempic. Eating smaller meals, avoiding high-fat foods, and staying well-hydrated can help manage symptoms during the initial adjustment period.
Why do I feel so full after eating on Ozempic?
Ozempic slows gastric emptying (the rate food leaves your stomach) and acts on brain appetite centres, causing early satiety and prolonged fullness. This is part of the medication's therapeutic mechanism and helps with glycaemic control.
When should I contact my GP about Ozempic side effects?
Contact your GP promptly if you experience severe persistent vomiting preventing fluid intake, signs of dehydration, severe abdominal pain, visual changes, or symptoms of low blood sugar. Seek immediate medical attention for severe allergic reactions or symptoms suggesting pancreatitis.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript