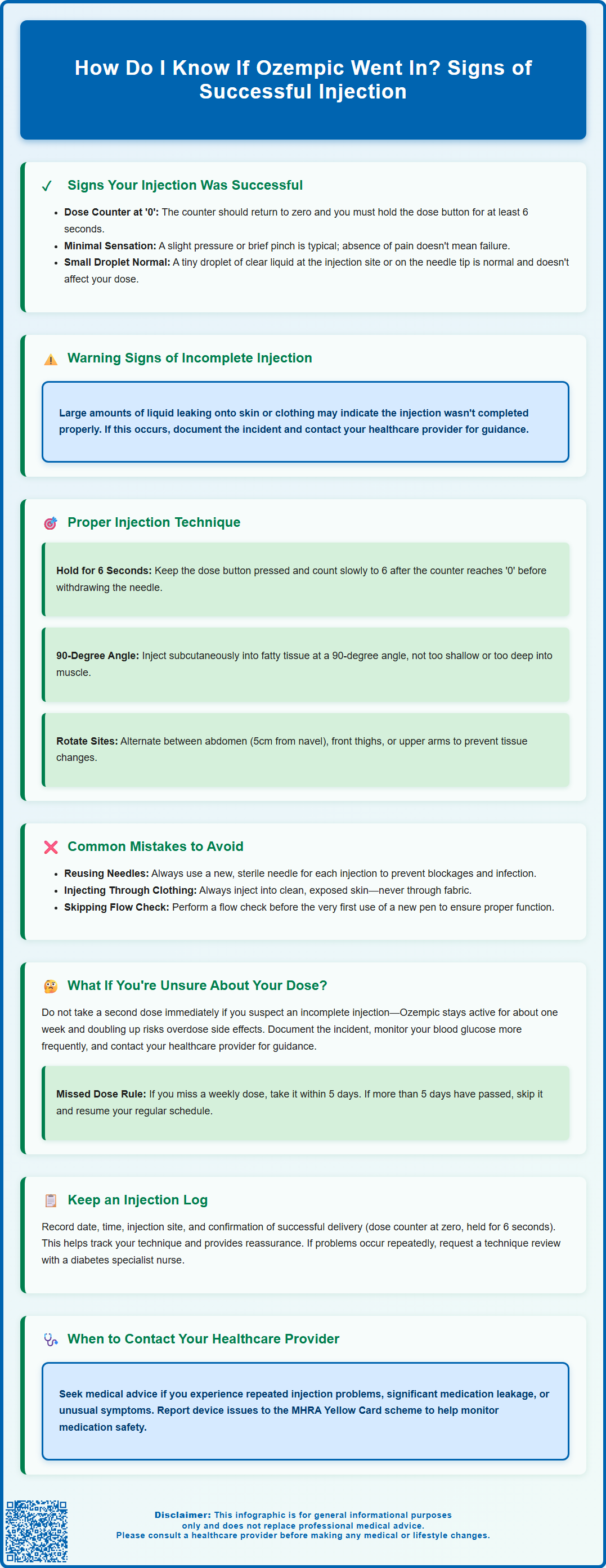
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist prescribed for type 2 diabetes management in the UK. Knowing whether your Ozempic injection was successful is essential for effective treatment. Key indicators include the dose counter returning to '0', maintaining pressure on the dose button for at least 6 seconds, and minimal liquid leakage at the injection site. Most patients experience only slight pressure during injection. If you're uncertain about dose delivery, do not administer a second injection immediately—contact your GP or diabetes specialist nurse for guidance. This article explains how to confirm successful administration and avoid common injection errors.
Summary: You can confirm your Ozempic injection was successful if the dose counter returned to '0' and you maintained pressure on the dose button for 6 seconds before withdrawing the needle.
- Ozempic is a GLP-1 receptor agonist administered subcutaneously once weekly for type 2 diabetes management in the UK.
- Successful injection indicators include the dose counter at '0', holding the button for 6 seconds, and minimal liquid leakage at the injection site.
- Common errors include premature needle withdrawal, incorrect injection depth, and reusing needles, which can compromise dose delivery.
- If uncertain about dose delivery, do not inject again immediately—contact your GP or diabetes specialist nurse for guidance.
- Missed doses can be taken within 5 days; if more than 5 days have passed, skip that dose and resume your regular schedule.
- Report suspected side effects or device problems to the MHRA via the Yellow Card scheme.
Table of Contents
Signs Your Ozempic Injection Was Successful
Understanding injection success is important for patients using Ozempic (semaglutide), a glucagon-like peptide-1 (GLP-1) receptor agonist prescribed for type 2 diabetes management in the UK. When administered correctly, Ozempic is delivered subcutaneously into the fatty tissue beneath the skin, where it is absorbed gradually into the bloodstream.
Reliable indicators that your injection was successful include seeing the dose counter return to '0' and maintaining pressure on the dose button for at least 6 seconds as recommended in the Patient Information Leaflet. After withdrawing the needle, you may notice a small droplet of clear liquid at the injection site or on the needle tip—this is normal and typically represents an insignificant amount that does not affect your dose.
Physical sensations during injection are usually minimal. Most patients report feeling only slight pressure or a brief pinch. The absence of pain does not indicate failure; Ozempic injections are designed to be relatively comfortable. You should not see significant liquid leaking from the injection site after withdrawal, though a tiny amount is acceptable. If you notice a large wet patch on your skin or clothing, this may suggest the injection was not completed properly.
Over the following hours and days, successful administration is reflected in the medication's therapeutic effects, though these develop gradually. Patients should not expect immediate symptoms confirming absorption. If you have persistent concerns about whether your injection was successful, contact your GP or diabetes specialist nurse rather than administering an additional dose. If a weekly dose is missed, you can take it within 5 days of the missed dose. If more than 5 days have passed, skip that dose and take your next dose on the regularly scheduled day.
Common Injection Mistakes and How to Avoid Them
Premature needle withdrawal represents one of the most frequent errors with Ozempic administration. The manufacturer specifies that users must keep the dose button pressed and count slowly to 6 after the dose counter reaches '0'. Releasing pressure or withdrawing the needle too quickly can result in incomplete dose delivery, as the medication requires this time to fully dispense from the pen into the subcutaneous tissue. To avoid this mistake, count aloud or use a timer, and only release the button after the full 6-second hold.
Incorrect injection depth can compromise medication delivery. Ozempic must be injected subcutaneously—into the fatty layer beneath the skin—not intramuscularly or intradermally. Injecting too shallow may cause the medication to leak back out, whilst injecting too deep into muscle can alter absorption rates and cause discomfort. Using the correct technique involves pinching the skin gently (if needed, particularly in leaner individuals) and inserting the needle at a 90-degree angle, following FIT UK injection technique recommendations. Compatible NovoFine or NovoTwist needles (typically 4mm, up to 8mm) are recommended for subcutaneous delivery.
Failing to check the flow before first use is another common error. New pens require a flow check to ensure the needle is properly attached and medicine flows through. This involves selecting the flow check symbol, pointing the needle upward, and pressing the button until a droplet appears at the needle tip. This flow check is only needed before the very first use of a new pen, not routinely after periods of non-use.
Reusing needles is strongly discouraged, as this can cause needle blockages, increase infection risk, and lead to inaccurate dosing. Always attach a new, sterile needle for each injection. Additionally, injecting through clothing should be avoided, as fabric can deflect the needle or introduce contaminants. Always inject into clean, exposed skin at recommended sites: the abdomen (avoiding the area around the navel), thigh, or upper arm.
What to Do If You're Unsure About Your Dose
If you suspect your injection was incomplete, the most important principle is: do not administer a second dose immediately. Ozempic has a long half-life of approximately one week, meaning it remains active in your system for an extended period. Administering an additional dose could result in overdosing, increasing the risk of adverse effects including nausea, vomiting and diarrhoea. The risk of hypoglycaemia (low blood sugar) is primarily a concern if you are also taking insulin or sulfonylurea medications.
Document your concerns by noting the time of injection, what made you uncertain (e.g., liquid leakage, early needle withdrawal), and any immediate observations. Check your blood glucose levels more frequently over the next 24-48 hours if you have a home monitoring device, as this can provide indirect evidence of medication effect. However, remember that Ozempic's glucose-lowering effects are gradual and may not show immediate dramatic changes.
Contact your healthcare provider for guidance—either your GP, diabetes specialist nurse, or hospital diabetes team. They can advise on the best course of action. According to the Patient Information Leaflet, if you miss a weekly dose, you can take it within 5 days of the missed dose. If more than 5 days have passed, skip that dose and take your next dose on the regularly scheduled day. The same principle applies if you're unsure whether your dose was delivered properly.
For future injections, consider keeping a simple injection log where you record the date, time, injection site, and a brief note confirming successful administration (e.g., "dose counter at 0, held for 6 seconds"). This practice can provide reassurance and help identify patterns if problems recur. If you repeatedly experience uncertainty about dose delivery, request a review of your injection technique with a diabetes specialist nurse, who can observe your method and provide personalised guidance. Report any suspected side effects or device problems to the MHRA via the Yellow Card scheme.
Proper Ozempic Injection Technique Step-by-Step
Preparation phase begins with hand hygiene—wash your hands thoroughly with soap and water. Remove your Ozempic pen from the refrigerator approximately 15-30 minutes before injection to allow it to reach room temperature, which improves comfort. Check the medication by holding the pen up to the light; the solution should be clear and colourless. Do not use if it appears cloudy, discoloured, or contains particles. Gather your supplies: the Ozempic pen, a new compatible needle (such as NovoFine or NovoTwist, supplied separately), and an alcohol wipe if recommended by your healthcare team, though routine skin cleansing is not always necessary for patients with good hygiene.
Attaching the needle and checking the flow (for new pens only) requires removing the pen cap and checking that the dose counter shows the correct remaining doses. Remove the protective seal from a new needle and screw or push it straight onto the pen until secure. Remove both the outer and inner needle caps (keep the outer cap for disposal). For a new pen only, check the flow by turning the dose selector to the flow check symbol, point the needle upward, tap gently to move air bubbles to the top, then press and hold the dose button until a droplet appears at the needle tip. This flow check is only needed before the very first use of a new pen.
Selecting and preparing the injection site involves choosing from three approved areas: the abdomen (at least 5cm away from the navel), the front of the thighs, or the upper arm (though this may require assistance). Rotate sites with each injection to prevent lipohypertrophy (fatty lumps) or lipoatrophy (tissue loss). The skin should be clean and dry. If using alcohol wipes, allow the area to dry completely before injecting.
Administering the injection begins with turning the dose selector to your prescribed dose (0.25mg, 0.5mg, 1mg, or 2mg). If needed, gently pinch the skin to lift the fatty tissue. Insert the needle at a 90-degree angle with a quick, dart-like motion. Press the dose button fully until it stops. Crucially, keep the button pressed and count slowly to 6 whilst the needle remains in the skin. After 6 seconds, release the button and withdraw the needle straight out. Do not rub the injection site. Carefully replace the outer needle cap, unscrew the needle, and dispose of it immediately in a sharps container. Replace the pen cap and store the pen as directed—refrigerated if unopened, or at room temperature (below 30°C) for up to 6 weeks once in use. Do not freeze. Keep the pen cap on to protect from light. Never share your pen with others and follow local arrangements for sharps disposal through your GP or pharmacy.
Frequently Asked Questions
How do I know if my Ozempic injection went in properly?
The most reliable sign is that the dose counter returns to '0' and you held the dose button pressed for the full 6 seconds after the counter reached zero. You may see a tiny droplet of liquid at the injection site or on the needle tip after withdrawal, which is normal and doesn't mean your dose failed.
What should I do if I think my Ozempic didn't go in fully?
Do not inject a second dose immediately, as Ozempic stays active in your system for about a week and doubling up could cause overdose side effects like severe nausea. Contact your GP or diabetes nurse for advice, and monitor your blood glucose more frequently over the next 24–48 hours if you have a home testing device.
Can I take Ozempic with other diabetes medications like metformin?
Yes, Ozempic is commonly prescribed alongside other diabetes medicines such as metformin, though your doctor will tailor your combination therapy. If you're also taking insulin or sulfonylureas, be aware that the risk of low blood sugar (hypoglycaemia) increases, so closer glucose monitoring may be needed.
Why do I need to hold the button for 6 seconds after injecting Ozempic?
The 6-second hold ensures the full dose is delivered into the fatty tissue beneath your skin, as the medication takes time to dispense completely from the pen. Releasing the button or withdrawing the needle too early is one of the most common mistakes that can result in an incomplete dose.
What's the difference between injecting Ozempic into fat versus muscle?
Ozempic must be injected subcutaneously into the fatty layer beneath the skin, not into muscle, to ensure proper absorption and effectiveness. Injecting too deep into muscle can alter how quickly the drug is absorbed and may cause discomfort, whilst injecting too shallow can lead to leakage back out of the skin.
How do I get an Ozempic prescription in the UK?
You'll need a prescription from your GP or diabetes specialist, as Ozempic is a prescription-only medicine licensed for type 2 diabetes management in the UK. Your doctor will assess whether it's suitable for you based on your diabetes control, other medications, and overall health, and will provide training on proper injection technique.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript