What if you inject Ozempic into a vein? This is a critical safety question for patients using semaglutide therapy. Ozempic is a GLP-1 receptor agonist licensed exclusively for subcutaneous injection in type 2 diabetes management. Whilst accidental intravenous administration is extremely unlikely with proper technique, understanding the potential consequences and correct injection methods is essential for patient safety. This article examines what could happen if Ozempic enters a vein, how to prevent injection errors, and when to seek medical advice following suspected administration mistakes.
Summary: Ozempic must never be injected into a vein; intravenous administration could cause rapid systemic absorption, potentially intensifying gastrointestinal side effects and altering the drug's pharmacokinetic profile.
- Ozempic is a GLP-1 receptor agonist licensed exclusively for subcutaneous injection into fatty tissue beneath the skin.
- Accidental intravenous injection is extremely unlikely when proper technique is followed using the short needles provided with the pen device.
- Rapid intravenous delivery could theoretically increase acute adverse effects such as severe nausea, vomiting, and gastrointestinal distress.
- Patients should seek immediate medical attention if they experience severe symptoms including chest pain, persistent vomiting, confusion, or signs of allergic reaction after injection.
- Proper training from healthcare professionals, correct injection technique, and regular site rotation are essential to prevent administration errors.
Table of Contents
How Ozempic Should Be Administered Correctly
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. It's important to note that for weight management, a different semaglutide product called Wegovy is used, which has different strengths and a different device. Ozempic is designed exclusively for subcutaneous injection, meaning it must be administered into the fatty tissue layer beneath the skin. This route of administration ensures the drug is absorbed gradually into the bloodstream, providing steady therapeutic levels over the dosing interval.
The approved injection sites for Ozempic include the abdomen (avoiding a 5cm radius around the navel), the front of the thighs, or the upper arms (though upper arm injections may require assistance from another person). Patients should rotate injection sites within the same body region each week to prevent local skin problems and ensure consistent absorption. The pre-filled pen device is designed to deliver a precise dose when used correctly.
Before using a new pen for the first time, patients should perform a flow check (sometimes called an 'air shot') to ensure the pen is functioning properly. Before each injection, patients should inspect the solution to ensure it is clear and colourless. A new needle must be attached for each injection, and needles should never be reused. After selecting the prescribed dose, the needle should be inserted fully into the skin (typically at a 90-degree angle with 4-6mm needles), the dose button pressed until it stops, and held in place for at least six seconds while the dose counter shows '0' to ensure complete delivery. The needle is then withdrawn and disposed of safely in a sharps container.
Proper training from a healthcare professional is essential before initiating Ozempic therapy. Patients should receive clear written and verbal instructions, ideally with a demonstration using a training device. Pens should never be shared with others, even if the needle is changed. This education significantly reduces the risk of administration errors and ensures optimal therapeutic outcomes whilst minimising potential complications.
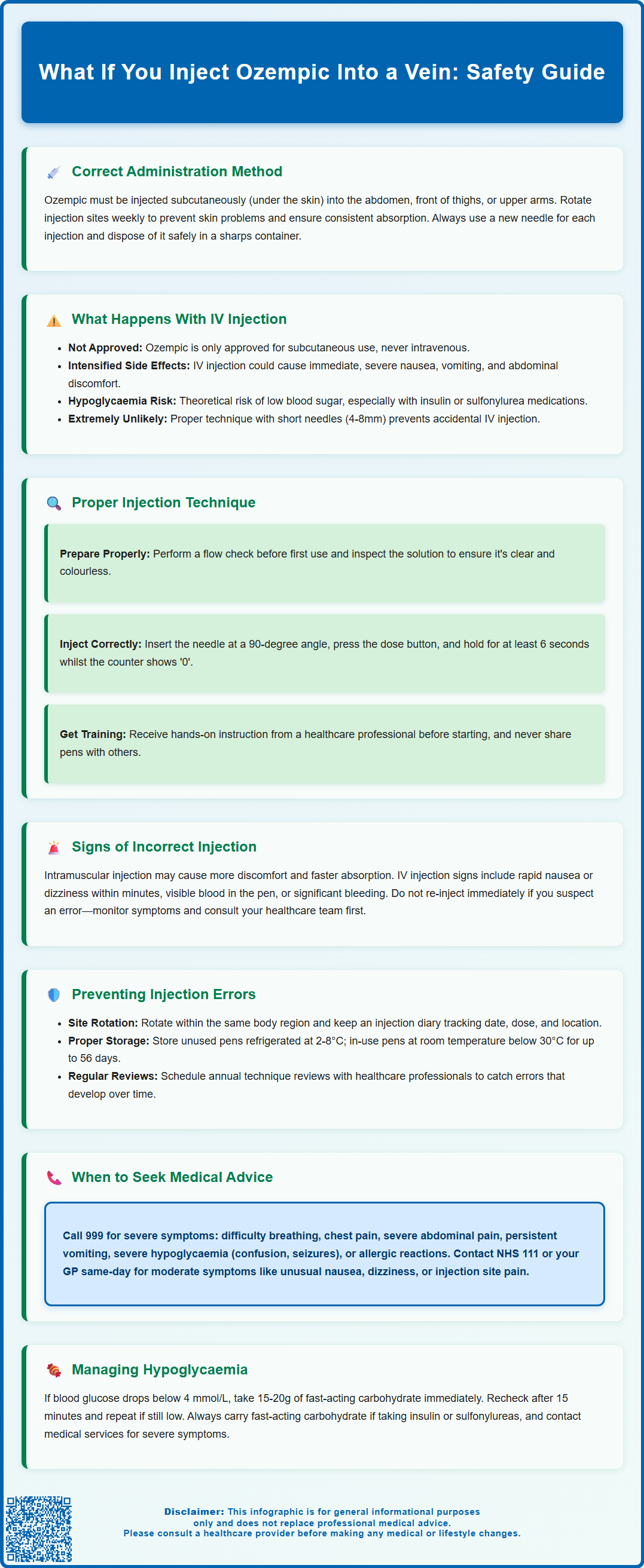
What Happens If Ozempic Is Injected Into a Vein
Intravenous administration of Ozempic is not an approved route and must not be used. The medication is formulated and licensed exclusively for subcutaneous use, as clearly stated in the Summary of Product Characteristics. If Ozempic were inadvertently injected directly into a vein, the entire dose would enter the systemic circulation immediately rather than being absorbed gradually from subcutaneous tissue. This rapid delivery could potentially alter the pharmacokinetic profile of semaglutide, leading to an unexpected concentration peak.
The most significant concern with accidental intravenous injection would be an increased risk of acute adverse effects. Semaglutide's mechanism of action involves slowing gastric emptying, enhancing glucose-dependent insulin secretion, and suppressing glucagon release. A sudden high concentration in the bloodstream might intensify gastrointestinal effects such as nausea, vomiting, and abdominal discomfort. There is also a theoretical possibility of more pronounced cardiovascular effects, though this remains speculative as semaglutide is generally well-tolerated from a cardiac perspective.
Hypoglycaemia represents another potential concern, particularly in patients taking concomitant insulin or sulfonylureas. Whilst semaglutide alone rarely causes hypoglycaemia due to its glucose-dependent mechanism, a rapid bolus effect combined with other glucose-lowering medications could theoretically increase this risk. Additionally, the immediate systemic exposure might provoke more severe gastrointestinal distress than typically experienced with subcutaneous administration.
It is important to emphasise that accidental intravenous injection of Ozempic is extremely unlikely when proper subcutaneous technique is followed. The short needles provided with the pen device (typically 4-8mm) are specifically designed to reach subcutaneous tissue but not deeper structures. Brief bleeding at the injection site can occur normally and is not necessarily evidence of intravenous injection; applying gentle pressure to the site is usually sufficient.
Signs of Incorrect Injection and What to Do
Recognising the signs of an incorrectly administered Ozempic injection is important for patient safety and treatment efficacy. If the injection has been given into muscle (intramuscular) rather than subcutaneous tissue, patients may experience more discomfort at the injection site, potentially faster absorption, and possibly more pronounced side effects. Intramuscular injection might occur if the needle is too long for the patient's body habitus or if the injection technique is incorrect.
In the highly unlikely event of intravenous injection, patients might notice symptoms that differ from their usual experience with the medication. These could potentially include rapid onset of nausea or dizziness within minutes rather than hours. There may be visible blood in the pen device or significant bleeding at the injection site, though minor bleeding is common with subcutaneous injections and does not necessarily indicate a problem.
If a patient suspects an injection error, they should not administer another dose immediately. The first step is to remain calm and monitor for symptoms. If the error involves uncertainty about whether the full dose was delivered subcutaneously (for example, if medication leaked from the injection site), patients should not attempt to re-inject the missing dose without consulting their healthcare team. According to the Ozempic Patient Information Leaflet, if a dose is missed, it can be administered within 5 days of the scheduled dose; if more than 5 days have passed, the missed dose should be skipped and the next dose taken on the regularly scheduled day.
For minor concerns such as slight bleeding or bruising at the injection site without systemic symptoms, patients can apply gentle pressure with clean gauze and monitor the area. However, if there are any unusual or concerning symptoms—particularly severe nausea, vomiting, significant pain, dizziness, rapid heartbeat, or signs of hypoglycaemia such as tremor, sweating, or confusion—medical advice should be sought promptly. If hypoglycaemia occurs (blood glucose below 4 mmol/L), patients should take 15-20g of fast-acting carbohydrate (such as glucose tablets or fruit juice), recheck after 15 minutes, and repeat if necessary. For more serious symptoms, patients should contact their GP, diabetes specialist nurse, NHS 111, or in cases of severe symptoms, attend an emergency department.
Preventing Injection Errors With Ozempic
Prevention of injection errors begins with comprehensive patient education at the point of prescribing. Healthcare professionals should provide hands-on training with the Ozempic pen device, allowing patients to practice with a demonstration pen before administering their first dose. This training should cover all steps: attaching a new needle for each injection, performing the flow check with a new pen, selecting the dose, proper injection technique, and safe needle disposal. Written instructions and manufacturer-provided materials should supplement verbal teaching.
Correct injection technique is fundamental to preventing errors. Patients should wash their hands thoroughly before handling the pen and ensure the injection site is clean and dry. With the standard 4mm needles, most patients can inject at a 90-degree angle without pinching the skin. Very lean patients may benefit from pinching the skin to create a subcutaneous 'tent' or using a 45-degree angle to avoid intramuscular injection. The needle should be inserted swiftly and confidently, the dose button pressed completely, and the needle held in place for at least 6 seconds while the dose counter shows '0'.
Regular site rotation within the same body region helps maintain healthy subcutaneous tissue and consistent absorption. Patients should avoid injecting into areas with scarring, bruising, or skin problems. Keeping a simple injection diary noting the date, time, dose, and site can help establish a rotation pattern and provide useful information if problems arise. The abdomen generally offers the most consistent absorption and is often the preferred site.
Proper storage and handling of Ozempic pens is also important in preventing errors. Unused pens should be refrigerated (2-8°C), while in-use pens can be kept at room temperature (below 30°C) for up to 56 days. Pens should never be frozen or exposed to extreme heat. If a pen malfunctions or if patients experience adverse effects, they should report this through the MHRA Yellow Card Scheme.
Ongoing support from healthcare professionals is essential for maintaining correct technique over time. Annual reviews should include observation of the patient's injection technique, as errors can develop gradually. Community pharmacists and practice nurses play a vital role in providing this ongoing education and troubleshooting. Patients should be encouraged to ask questions and report any difficulties or concerns about their injection technique. For those with visual impairment, dexterity problems, or cognitive difficulties, involving a family member or carer in the training process, or arranging for a healthcare professional to administer injections, may be appropriate.
When to Seek Medical Advice After an Injection Mistake
Understanding when to seek medical advice following a suspected injection error is crucial for patient safety. Immediate medical attention is warranted if a patient experiences severe symptoms after injection, including significant difficulty breathing, chest pain, severe abdominal pain, persistent vomiting that prevents fluid intake, signs of severe hypoglycaemia (confusion, loss of consciousness, seizures), or symptoms of an allergic reaction such as widespread rash, facial swelling, or throat tightness. In these circumstances, patients should call 999 or attend the nearest emergency department.
For less severe but concerning symptoms, patients should contact NHS 111, their diabetes specialist nurse, or their GP practice for same-day advice. These situations include moderate to severe nausea and vomiting that develops unusually quickly after injection, unexplained dizziness or feeling faint, unusual pain at the injection site, or symptoms of hypoglycaemia in patients taking other diabetes medications. If hypoglycaemia occurs (blood glucose below 4 mmol/L), patients should take 15-20g of fast-acting carbohydrate (such as glucose tablets, sugary drinks, or fruit juice), wait 15 minutes, and recheck. If still below 4 mmol/L, they should repeat the treatment. Patients on insulin or sulfonylureas should always carry fast-acting carbohydrate with them.
Patients should also seek advice if they are uncertain whether the full dose was delivered correctly. This might occur if there was significant leakage at the injection site, if the pen malfunctioned, or if the injection was interrupted. Rather than attempting to re-inject, patients should follow the missed dose guidance in the Patient Information Leaflet: if within 5 days of the scheduled dose, take it as soon as possible; if more than 5 days have passed, skip the missed dose and take the next dose on the regular day. Patients should contact their diabetes specialist nurse or GP if they need further guidance.
Routine follow-up with the prescribing healthcare professional is appropriate for non-urgent concerns such as persistent bruising at injection sites, questions about technique, or general uncertainty about the injection process. Patients should not discontinue Ozempic without medical advice, even if they have experienced an injection error, as abrupt cessation can affect diabetes control. Any suspected device faults should be reported via the MHRA Yellow Card Scheme. Documentation of any injection errors in the patient's medical records helps inform ongoing management and may identify the need for additional training or support.
Scientific References
- Ozempic 0.5 mg solution for injection in pre-filled pen - Summary of Product Characteristics.
- Ozempic - European Public Assessment Report.
- Population Pharmacokinetics of Semaglutide for Type 2 Diabetes.
- Biggest shake-up in type 2 diabetes care in a decade announced.
- GLP-1 medicines for weight loss and diabetes: what you need to know.
Frequently Asked Questions
What would actually happen if I accidentally injected Ozempic into a vein?
If Ozempic were injected directly into a vein, the entire dose would enter your bloodstream immediately rather than being absorbed gradually, potentially causing a rapid concentration peak. This could lead to more intense side effects such as severe nausea, vomiting, and abdominal discomfort, and might increase the risk of hypoglycaemia if you're taking other diabetes medications. However, accidental intravenous injection is extremely unlikely with proper subcutaneous technique, as the short needles provided (4-8mm) are specifically designed to reach only the fatty tissue beneath the skin.
Can I use the same Ozempic pen needle more than once to save money?
No, you must use a new needle for each Ozempic injection and never reuse needles. Reusing needles increases the risk of infection, can damage the needle tip making injections more painful, and may affect the accuracy of your dose delivery. Used needles should be disposed of safely in a sharps container after each injection.
How can I tell if my Ozempic injection went into muscle instead of fat?
An intramuscular injection may cause more discomfort at the injection site, potentially faster absorption, and possibly more pronounced side effects than usual. This can occur if the needle is too long for your body type or if you're injecting at the wrong angle. To prevent this, most patients can inject at a 90-degree angle with standard 4mm needles, whilst very lean patients may benefit from pinching the skin or using a 45-degree angle.
What's the difference between Ozempic and Wegovy if they're both semaglutide?
Ozempic is licensed in the UK specifically for treating type 2 diabetes mellitus, whilst Wegovy is the semaglutide product approved for weight management. Although both contain the same active ingredient, they come in different strengths and use different pen devices. Your healthcare professional will prescribe the appropriate product based on your specific medical condition and treatment goals.
If I see blood after injecting Ozempic, does that mean I hit a vein?
Brief bleeding at the injection site is common with subcutaneous injections and does not necessarily indicate you've hit a vein. Simply apply gentle pressure with clean gauze to stop the bleeding. However, if you notice blood in the pen device itself, significant bleeding, or experience rapid onset of unusual symptoms like severe nausea within minutes, you should seek medical advice.
What should I do if I'm not sure whether my full Ozempic dose went in properly?
Do not attempt to re-inject another dose immediately if you're uncertain whether the full dose was delivered. If medication leaked from the injection site or the injection was interrupted, contact your diabetes specialist nurse or GP for guidance rather than guessing. According to the Patient Information Leaflet, if you've missed a dose entirely, you can take it within 5 days of the scheduled time; if more than 5 days have passed, skip it and resume your regular schedule.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript