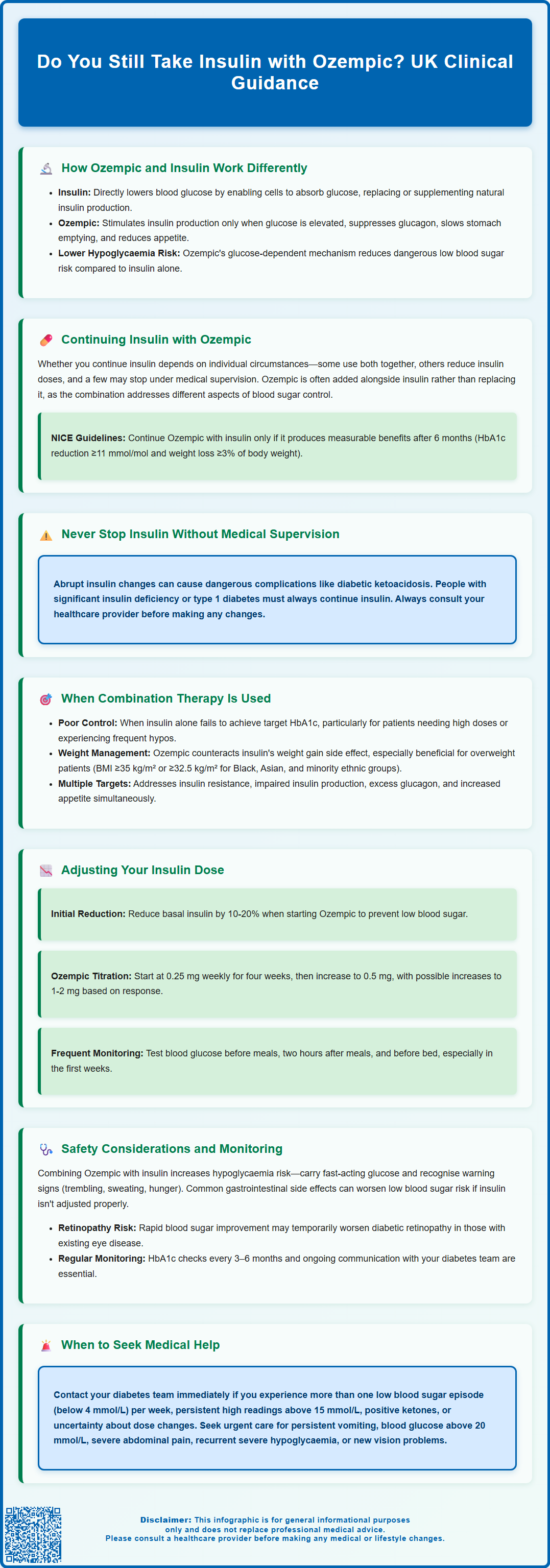
Many people with type 2 diabetes wonder whether they can stop taking insulin after starting Ozempic (semaglutide). The answer depends entirely on individual circumstances, diabetes control, and clinical needs. Whilst some patients may reduce or discontinue insulin under careful medical supervision, others continue both medications as complementary therapies. Ozempic and insulin work through different mechanisms—insulin directly replaces the hormone your body lacks, whilst Ozempic enhances your body's own glucose regulation. Any changes to insulin therapy must be supervised by your GP or diabetes specialist, as abrupt adjustments can lead to dangerous complications including diabetic ketoacidosis.
Summary: Whether you continue insulin with Ozempic depends on individual diabetes control—some people maintain both medications, others reduce insulin doses, and a minority may discontinue insulin under strict medical supervision.
- Ozempic is a GLP-1 receptor agonist that stimulates insulin production only when blood glucose is elevated, whilst insulin directly replaces the hormone.
- NICE guidance supports combining Ozempic with insulin for type 2 diabetes when glucose targets aren't met with insulin alone, particularly when weight management is a concern.
- Any insulin dose reduction must be gradual with close monitoring, as abrupt changes can precipitate diabetic ketoacidosis, especially in those with significant insulin deficiency.
- Hypoglycaemia risk increases when Ozempic is combined with insulin, requiring frequent blood glucose monitoring and proactive dose adjustments.
- Regular HbA1c monitoring, retinal screening, and prompt reporting of side effects through the Yellow Card Scheme are essential safety measures for combination therapy.
Table of Contents
Understanding Ozempic and Insulin: How They Work Differently
Ozempic (semaglutide) and insulin are both used to manage type 2 diabetes, but they work through fundamentally different mechanisms. Understanding these differences is essential for anyone considering or currently using these medications.
Insulin is a hormone that directly lowers blood glucose levels by enabling cells throughout the body to absorb glucose from the bloodstream. People with type 2 diabetes either don't produce enough insulin or their bodies don't respond effectively to it (insulin resistance). Injectable insulin therapy replaces or supplements the body's natural insulin production, providing immediate glucose-lowering effects.
Ozempic belongs to a class of medications called GLP-1 receptor agonists (glucagon-like peptide-1). Rather than replacing insulin, Ozempic works by mimicking a natural hormone that stimulates the pancreas to produce more insulin—but only when blood glucose levels are elevated. It also suppresses glucagon secretion (also in a glucose-dependent manner), which helps prevent the liver from releasing excess glucose. This glucose-dependent mechanism reduces the risk of hypoglycaemia when used alone, though this risk increases when combined with insulin or sulfonylureas. Additionally, Ozempic slows gastric emptying, which moderates the rise in blood glucose after meals, and reduces appetite, often leading to weight loss.
The key distinction is that insulin is a direct replacement therapy, whilst Ozempic enhances the body's own glucose regulation mechanisms. Insulin can be used in both type 1 and type 2 diabetes, whereas Ozempic is licensed only for type 2 diabetes in adults, as specified in the MHRA/EMC Summary of Product Characteristics. Because they work differently, these medications can complement each other in certain clinical situations, though this requires careful medical supervision and individualised treatment planning.
Do You Still Take Insulin with Ozempic?
Whether you continue taking insulin after starting Ozempic depends entirely on your individual circumstances, diabetes control, and clinical needs. There is no universal answer—some people may continue both medications, others may reduce their insulin dose, and a minority might discontinue insulin altogether under medical guidance.
For many people with type 2 diabetes who require insulin, Ozempic is added as a complementary therapy rather than a replacement. The combination can be particularly effective because the medications address different aspects of glucose control. Ozempic's ability to stimulate insulin production, slow digestion, and promote weight loss can enhance overall glycaemic control whilst potentially allowing for lower insulin doses.
NICE guidance (NG28) supports the use of GLP-1 receptor agonists like Ozempic in combination with insulin for adults with type 2 diabetes when blood glucose targets aren't being met with insulin alone, particularly if weight management is also a concern. Importantly, NICE recommends continuing GLP-1 receptor agonists only if there's a beneficial metabolic response (a reduction in HbA1c of at least 11 mmol/mol [1%] and weight loss of at least 3% of initial body weight) at 6 months.
Some individuals with well-controlled type 2 diabetes who were using small amounts of basal (long-acting) insulin may find that Ozempic provides sufficient glucose control on its own, allowing insulin to be discontinued. However, any reduction in insulin must be gradual with close monitoring. The MHRA has warned that abrupt insulin reduction or cessation when starting GLP-1 receptor agonists can precipitate diabetic ketoacidosis. People with significant insulin deficiency or those with type 1 diabetes should never stop insulin, as it remains essential for survival.
The critical point is that any changes to your insulin regimen must be supervised by your GP or diabetes specialist. Never adjust or stop insulin independently, as this can lead to dangerous hyperglycaemia (high blood sugar) or even diabetic ketoacidosis in severe cases. Also be aware that rapid improvement in blood glucose control with semaglutide may temporarily worsen diabetic retinopathy, particularly in those with pre-existing retinopathy who are on insulin. Report any new visual symptoms promptly.
When Insulin and Ozempic Are Used Together
Combination therapy with Ozempic and insulin is increasingly common in clinical practice and can offer significant benefits for specific patient groups. Understanding when this approach is appropriate helps clarify treatment goals and expectations.
Clinical scenarios where combination therapy is considered include:
-
Inadequate glycaemic control: When HbA1c (a measure of average blood glucose over 2–3 months) remains above target despite optimised insulin therapy
-
Weight management concerns: Insulin therapy often causes weight gain, whilst Ozempic typically promotes weight loss—a valuable combination for overweight or obese patients
-
High insulin requirements: People requiring large insulin doses may benefit from Ozempic's insulin-sparing effects
-
Frequent hypoglycaemia: Ozempic's glucose-dependent mechanism may allow insulin dose reduction, decreasing hypoglycaemia risk
According to NICE clinical guidelines (NG28), GLP-1 receptor agonists like Ozempic should be considered for adults with type 2 diabetes who have a BMI of 35 kg/m² or higher (or lower thresholds of approximately 32.5 kg/m² for people of Black, Asian and other minority ethnic groups) and specific psychological or medical problems associated with obesity. They may also be considered when BMI is below 35 kg/m² if insulin would have significant occupational implications or if weight loss would benefit other significant obesity-related comorbidities. The guidance also supports their use in combination with insulin when triple therapy with metformin and other oral agents hasn't achieved adequate control.
The combination approach addresses multiple pathophysiological defects in type 2 diabetes: insulin resistance, impaired insulin secretion, excessive glucagon release, and increased appetite. By targeting these different mechanisms simultaneously, many patients achieve better overall glucose control with improved quality of life.
Your diabetes team will assess factors including your current HbA1c, weight, hypoglycaemia frequency, insulin doses, other medications, and personal treatment goals when determining whether combination therapy is appropriate for you. Remember that NICE recommends continuing GLP-1 receptor agonists only if there's a reduction in HbA1c of at least 11 mmol/mol and weight loss of at least 3% after 6 months of treatment.
Adjusting Your Insulin Dose When Starting Ozempic
When initiating Ozempic whilst on insulin therapy, dose adjustments are typically necessary to prevent hypoglycaemia. This process requires close collaboration with your healthcare team and careful self-monitoring.
Initial insulin dose reduction is often recommended when starting Ozempic, particularly for basal (long-acting) insulin. Many clinicians suggest reducing basal insulin by 10–20% at Ozempic initiation, though the exact reduction must be individualised based on your current glucose control, insulin sensitivity, and hypoglycaemia history. Any insulin reduction should be stepwise and carefully monitored to avoid diabetic ketoacidosis (DKA), as warned by the MHRA. If you're using bolus (mealtime) insulin, adjustments may also be needed, especially as Ozempic slows gastric emptying and reduces appetite, potentially decreasing post-meal glucose excursions and altering the timing or amount of mealtime insulin required.
The titration schedule for Ozempic typically begins at 0.25 mg once weekly for four weeks (a non-therapeutic starter dose to improve gastrointestinal tolerability), increasing to 0.5 mg weekly thereafter. Further increases to 1 mg or 2 mg weekly may be considered based on glycaemic response and tolerability. Throughout this titration period, insulin requirements often decrease progressively, necessitating ongoing adjustments.
Practical monitoring recommendations include:
-
Frequent blood glucose testing: Check levels before meals, two hours after meals, and before bed, particularly during the first few weeks
-
Ketone testing: Check ketones if blood glucose is persistently above 13-15 mmol/L or if you feel unwell; seek urgent medical help if ketones are present
-
Recognising hypoglycaemia symptoms: Trembling, sweating, confusion, rapid heartbeat, or feeling faint
-
Keeping fast-acting carbohydrates available: Glucose tablets, sugary drinks, or sweets to treat low blood sugar promptly
-
Maintaining a glucose diary: Record readings, insulin doses, meals, and any symptoms to identify patterns
Contact your diabetes team promptly if you experience recurrent hypoglycaemia (more than one episode of blood glucose below 4 mmol/L in a week), persistent hyperglycaemia (readings consistently above 15 mmol/L), positive ketones, or if you're uncertain about dose adjustments. Many diabetes services offer telephone or email support for dose titration queries between appointments.
Safety Considerations and Monitoring Blood Sugar Levels
Combining Ozempic with insulin requires heightened awareness of potential risks and diligent monitoring to ensure safe, effective treatment. Understanding these safety considerations empowers you to manage your diabetes confidently whilst minimising complications.
Hypoglycaemia risk, whilst lower with Ozempic alone due to its glucose-dependent mechanism, increases when combined with insulin. Warning signs include trembling, sweating, hunger, difficulty concentrating, and palpitations. Severe hypoglycaemia (requiring assistance from another person) is a medical emergency. Always carry fast-acting glucose and ensure family members or colleagues know how to help if needed. If you experience impaired awareness of hypoglycaemia (not recognising warning symptoms), inform your diabetes team immediately, as this requires specialist assessment.
Gastrointestinal side effects are common with Ozempic, particularly nausea, vomiting, and diarrhoea, especially during dose escalation. These symptoms usually improve over time but can affect appetite and food intake, potentially increasing hypoglycaemia risk if insulin doses aren't adjusted accordingly. Prolonged vomiting or diarrhoea can lead to dehydration and acute kidney injury, so maintaining adequate fluid intake is essential. Staying well-hydrated and eating smaller, more frequent meals may help manage these effects.
Diabetic retinopathy complications may temporarily worsen with rapid improvement in blood glucose control when starting semaglutide, particularly in people with pre-existing retinopathy who are on insulin. Report any new visual symptoms promptly and ensure your retinal screening is up to date.
Gallbladder disease, including gallstones, has been reported with GLP-1 receptor agonists. Contact your healthcare provider if you experience symptoms such as severe abdominal pain, particularly in the upper right area.
Regular HbA1c monitoring (typically every 3–6 months) helps assess overall glucose control and guides treatment adjustments. Your healthcare team will also monitor weight, blood pressure, kidney function, and cardiovascular risk factors, as comprehensive diabetes management extends beyond glucose control alone.
When to seek urgent medical attention:
-
Persistent vomiting preventing food or fluid intake
-
Blood glucose consistently above 20 mmol/L despite insulin
-
Positive ketone test results
-
Symptoms of diabetic ketoacidosis (excessive thirst, frequent urination, fruity breath odour, confusion)
-
Severe abdominal pain (potential sign of pancreatitis or gallbladder disease—if pancreatitis is suspected, stop taking Ozempic)
-
Recurrent severe hypoglycaemia
-
New or worsening visual problems
Report any suspected side effects via the Yellow Card Scheme at yellowcard.mhra.gov.uk or through your healthcare professional. Regular communication with your diabetes team, adherence to monitoring schedules, and prompt reporting of concerns are fundamental to safe, effective combination therapy with Ozempic and insulin.
Frequently Asked Questions
Can I stop taking insulin completely when I start Ozempic?
Some people with well-controlled type 2 diabetes using small amounts of basal insulin may discontinue insulin under medical supervision, but this decision must be made by your diabetes specialist. Never stop insulin independently, as abrupt cessation can cause dangerous hyperglycaemia or diabetic ketoacidosis.
How much should I reduce my insulin dose when starting Ozempic?
Many clinicians recommend reducing basal insulin by 10–20% when initiating Ozempic, though the exact reduction must be individualised. Your diabetes team will guide dose adjustments based on your blood glucose monitoring, current control, and hypoglycaemia history.
What are the risks of combining Ozempic with insulin?
The main risk is increased hypoglycaemia, requiring frequent blood glucose monitoring and insulin dose adjustments. Other considerations include gastrointestinal side effects, potential temporary worsening of diabetic retinopathy with rapid glucose improvement, and the need for adequate hydration to prevent kidney complications.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript










