Ozempic (semaglutide) is a once-weekly injectable medication prescribed for type 2 diabetes management in the UK. Learning how to inject Ozempic correctly is essential for achieving optimal blood sugar control and minimising side effects. This comprehensive guide explains proper injection technique, from preparing your pen and selecting injection sites to avoiding common mistakes. Whether you're new to Ozempic or seeking to refine your technique, understanding the correct administration method ensures safe, effective treatment. Always receive initial training from your diabetes specialist nurse or GP practice before starting Ozempic therapy.
Summary: Ozempic is injected subcutaneously once weekly using a pre-filled pen, with proper technique including site rotation, counting to six after pressing the dose button, and using a new needle for each injection.
- Ozempic is a GLP-1 receptor agonist administered as a once-weekly subcutaneous injection for type 2 diabetes treatment.
- Approved injection sites include the abdomen, thigh, and upper arm, with strict rotation required to prevent lipohypertrophy.
- After inserting the needle at 90 degrees, press and hold the dose button until the counter shows zero, then count to six before withdrawing.
- New needles must be used for each injection and disposed of in a sharps container; never reuse or share needles.
- Common side effects include gastrointestinal symptoms, which typically improve over time with proper dose escalation.
- Ozempic requires MHRA approval for type 2 diabetes and must meet NICE criteria for continued NHS prescribing based on HbA1c reduction.
Table of Contents
What Is Ozempic and How Does It Work?
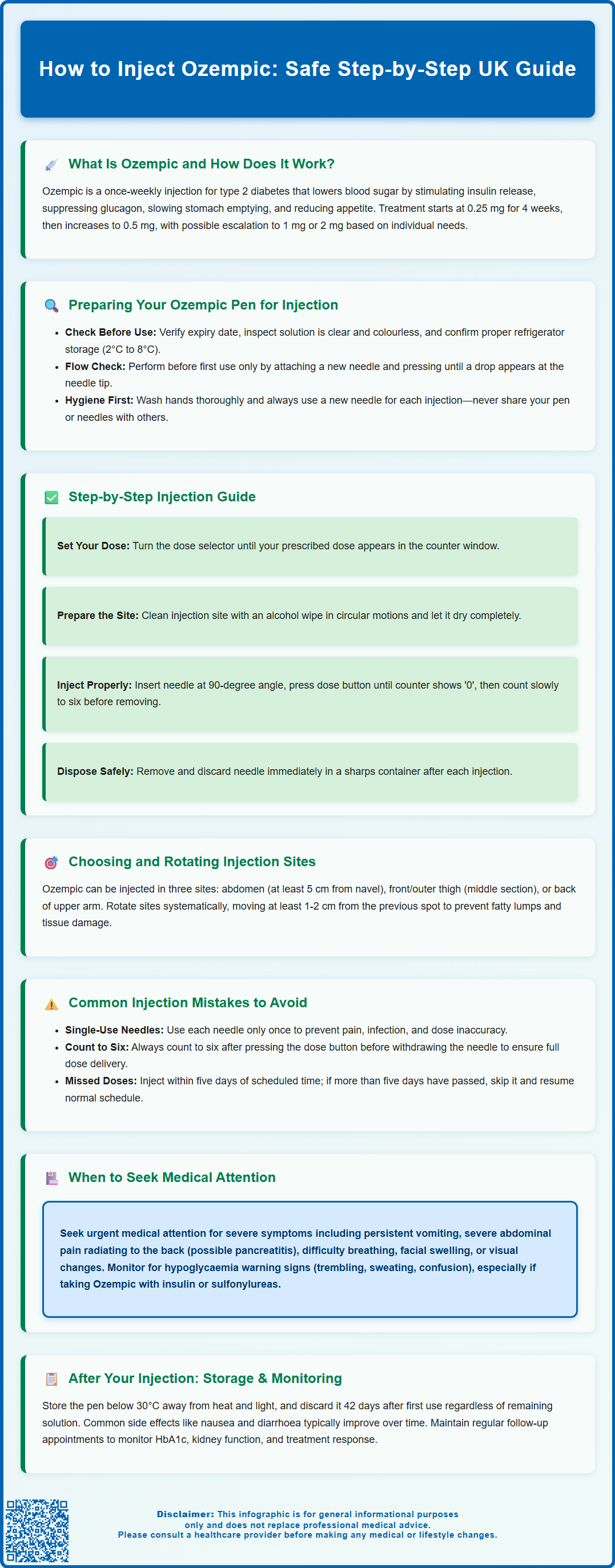
Ozempic (semaglutide) is a prescription medicine licensed in the UK for the treatment of type 2 diabetes mellitus in adults. It belongs to a class of medications called glucagon-like peptide-1 (GLP-1) receptor agonists, which work by mimicking the action of a naturally occurring hormone that helps regulate blood sugar levels.
The mechanism of action involves several complementary effects. Ozempic stimulates insulin secretion from the pancreas when blood glucose levels are elevated, whilst simultaneously suppressing the release of glucagon, a hormone that raises blood sugar. Additionally, it slows gastric emptying, which helps reduce post-meal glucose spikes, and acts on appetite centres in the brain to promote satiety and reduce food intake.
Ozempic is administered as a once-weekly subcutaneous injection. Treatment typically begins with a 0.25 mg dose for 4 weeks (for tolerability, not glycaemic control), then increases to 0.5 mg, with possible further escalation to 1 mg or 2 mg if needed. This makes it more convenient than daily injectable diabetes medications. The MHRA-approved indications include use as monotherapy when diet and exercise alone do not provide adequate glycaemic control and metformin is inappropriate, or in combination with other glucose-lowering medicines including insulin. Ozempic is not indicated for type 1 diabetes or diabetic ketoacidosis.
Clinical efficacy has been demonstrated in multiple trials, with significant reductions in HbA1c levels. In adults with type 2 diabetes and established cardiovascular disease, Ozempic has shown cardiovascular risk reduction benefits. According to NICE guidance (NG28), GLP-1 receptor agonists like Ozempic may be considered for adults with type 2 diabetes when treatment intensification is required and specific criteria are met, with continuation based on HbA1c reduction and weight loss response at review.
It is essential to understand that Ozempic requires proper injection technique to ensure optimal therapeutic effect and minimise adverse reactions. Patients should receive comprehensive training from their diabetes specialist nurse or GP practice before commencing treatment.
Preparing Your Ozempic Pen for Injection
Proper preparation of your Ozempic pen is crucial for safe and effective administration. Before each injection, several important steps must be followed to ensure the medication is suitable for use.
Initial checks should include:
-
Verify the expiry date printed on the pen label
-
Inspect the solution through the pen window – it should be clear and colourless
-
Check that you have the correct dose strength (0.25 mg, 0.5 mg, 1 mg, or 2 mg)
-
Ensure the pen has been stored correctly in a refrigerator (2°C to 8°C) before first use
Before first use only, you must perform a flow check to ensure the pen is working properly. Attach a new needle, select the flow check symbol (not a dose), hold the pen with the needle pointing upward, and press the dose button until the dose counter returns to zero. A drop of solution should appear at the needle tip. If no drop appears, try changing the needle and repeat the process. If no drop appears after repeating this process six times, do not use the pen and contact your pharmacy or the manufacturer.
For each injection, attach a new needle by removing the protective seal, screwing the needle straight onto the pen, and removing both the outer and inner needle caps. Never reuse needles, as this increases infection risk and may affect dose accuracy. Never share your pen or needles with anyone else, even if the needle is changed, as this poses a serious infection risk.
Hand hygiene is essential – wash your hands thoroughly with soap and water before handling the pen. Gather all necessary supplies: your Ozempic pen, a new needle, an alcohol wipe, and a sharps container for safe needle disposal.
Allow the pen to reach room temperature before injecting, as cold medication may cause discomfort at the injection site. However, do not warm the pen artificially using hot water or microwaves. After each use, remove the needle and store the pen with its cap on, without a needle attached.
Step-by-Step Guide to Injecting Ozempic Safely
Administering Ozempic correctly ensures optimal medication delivery and reduces the risk of complications. Follow this systematic approach for each weekly injection.
Step 1: Select your dose Turn the dose selector until the dose counter displays your prescribed dose. The pen will click as you turn it. If you select the wrong dose, you can turn the selector forwards or backwards to correct it.
Step 2: Prepare the injection site Choose an appropriate injection site (abdomen, thigh, or upper arm) and clean the area with an alcohol wipe using a circular motion. Allow the skin to dry completely – injecting through wet skin can cause stinging and may introduce bacteria.
Step 3: Insert the needle If using a 4 mm needle, you typically do not need to pinch the skin. For longer needles or if you are lean, gently pinch a fold of skin between your thumb and forefinger. Insert the needle into the skin at a 90-degree angle. The needle should be inserted to ensure subcutaneous delivery rather than intradermal or intramuscular injection. Do not inject into a vein or muscle. Note that the upper arm site may require assistance for correct placement.
Step 4: Inject the medication Press and hold the dose button until the dose counter shows '0'. Keep the button pressed and count slowly to six before withdrawing the needle. This ensures the full dose is delivered and prevents medication leakage.
Step 5: Withdraw and dispose If you pinched the skin, release the fold and withdraw the needle at the same angle it was inserted. A small amount of bleeding is normal – apply gentle pressure with a clean tissue if needed, but do not rub the site. Carefully place the outer needle cap back on, unscrew the needle, and dispose of it immediately in a sharps container.
Important safety note: If you see a drop of medication at the needle tip after withdrawal, this is normal and does not mean you have missed your dose. Never attempt to re-inject.
Choosing and Rotating Injection Sites
Proper site selection and rotation are essential components of safe Ozempic administration, helping to prevent complications such as lipohypertrophy (fatty lumps under the skin) and ensuring consistent medication absorption.
Approved injection sites for Ozempic include:
-
Abdomen: A commonly used site offering a large surface area. Inject at least 5 cm away from the navel and avoid the area directly around it.
-
Thigh: Use the front and outer aspects of the thigh, in the middle section between the hip and knee. Avoid the inner thigh where major blood vessels are located.
-
Upper arm: The back of the upper arm (triceps area) can be used, though this site may be more difficult to reach without assistance and offers a smaller injection area.
Site rotation strategy is crucial to prevent tissue damage. Never inject into the exact same spot twice in succession. A systematic approach involves rotating within an area and moving at least 1-2 cm from your previous injection site. For example, if using the abdomen, you might inject into different sections each week, ensuring you don't reuse the same spot.
Avoid injecting into areas that are:
-
Bruised, tender, red, or hard
-
Scarred or damaged
-
Areas where the skin is not normal (e.g., has lumps)
Maintaining a simple injection diary or using a smartphone app can help track your rotation pattern. Some patients find it helpful to inject on the same day each week (e.g., every Sunday evening) to establish a routine, though the specific day can be changed if needed, provided at least 72 hours have passed since the last injection.
Common Injection Mistakes and How to Avoid Them
Understanding frequent errors in Ozempic administration helps ensure treatment effectiveness and minimises adverse effects. Many injection-related problems are easily preventable with proper technique and awareness.
Reusing needles is one of the most common mistakes. Each needle should be used only once and then disposed of safely. Reusing needles causes them to become blunt and bent, leading to painful injections, increased risk of infection, and potential dose inaccuracy due to medication leakage or blockage.
Insufficient injection time occurs when patients fail to count to six after pressing the dose button. Withdrawing the needle too quickly can result in medication leaking from the injection site, meaning you receive less than your prescribed dose. This may compromise glycaemic control.
Incorrect injection depth can happen if the needle is inserted at the wrong angle or if the technique doesn't match your body type and needle length. This may affect medication absorption and efficacy. Adjust your technique based on needle length and body habitus – 4 mm needles typically don't require a skin pinch, while longer needles or lean patients may benefit from lifting a skin fold.
Poor site rotation leads to lipohypertrophy – lumpy areas of fat tissue that can affect medication absorption and cause unpredictable blood glucose levels. These areas may feel firm or rubbery and can take months to resolve. Strict adherence to site rotation prevents this complication.
Forgetting doses is problematic with weekly medications. If you miss a dose and it has been less than five days since the missed dose was due, inject as soon as you remember. If more than five days have passed, skip the missed dose and resume your normal schedule. Never double up doses to compensate.
Storage errors compromise medication integrity. Once in use, Ozempic pens can be stored at room temperature (below 30°C) or in the refrigerator for up to 6 weeks (42 days). Never freeze Ozempic, and discard any pen that has been frozen. Protect pens from direct sunlight and excessive heat. Always store the pen with its cap on and without a needle attached.
Not performing the initial flow check on new pens may result in using a faulty device, leading to dose inaccuracy. Never share your pen with others, even if you change the needle, as this poses serious infection risks.
What to Do After Your Ozempic Injection
Post-injection care and monitoring are important aspects of safe Ozempic use, helping to identify potential problems early and ensuring optimal treatment outcomes.
Immediate post-injection steps include proper needle disposal in a rigid, puncture-proof sharps container. Never dispose of needles in household waste or recycling bins. When your sharps container is three-quarters full, seal it and return it to your pharmacy or local authority collection point according to NHS or local council guidance. Replace the pen cap and store the pen appropriately – in the refrigerator if preferred, or at room temperature (below 30°C) away from direct heat and light. Remember to discard the pen 6 weeks (42 days) after first use, even if solution remains.
Monitoring for adverse effects is essential, particularly during the first few weeks of treatment or after dose increases. Common side effects include:
-
Gastrointestinal symptoms: Nausea, vomiting, diarrhoea, and constipation are the most frequently reported adverse effects, typically improving over time. Eating smaller, more frequent meals and avoiding fatty foods may help.
-
Injection site reactions: Mild redness, itching, or swelling at the injection site usually resolves within a few days. Rotating sites properly minimises this risk.
-
Hypoglycaemia: Whilst uncommon with Ozempic alone, the risk increases when used with insulin or sulfonylureas. Recognise warning signs including trembling, sweating, confusion, and palpitations.
When to seek medical advice:
-
Contact your GP or diabetes nurse if you experience persistent vomiting, severe abdominal pain (particularly if radiating to the back), or signs of pancreatitis
-
Seek urgent medical attention for symptoms of severe allergic reaction (difficulty breathing, facial swelling, severe rash)
-
Report any visual changes, as diabetic retinopathy may worsen initially during glycaemic improvement
-
Contact your healthcare team if you develop signs of dehydration from gastrointestinal side effects
-
Seek medical advice for symptoms of gallbladder disease (right upper quadrant pain, fever, jaundice)
Blood glucose monitoring frequency should be discussed with your diabetes team. Regular monitoring helps assess treatment effectiveness and guides dose adjustments. Keep a record of your readings to share at appointments.
Maintain regular follow-up appointments to monitor HbA1c, renal function, and treatment response. Your healthcare team will assess whether Ozempic continues to meet NICE criteria for ongoing prescribing, including HbA1c reduction and weight loss response.
Scientific References
Frequently Asked Questions
Where should I inject Ozempic on my body?
Ozempic can be injected into three approved sites: the abdomen (at least 5 cm from the navel), the front and outer thigh, or the back of the upper arm. Rotate injection sites weekly, moving at least 1-2 cm from your previous injection spot to prevent tissue damage and ensure consistent medication absorption.
What happens if I don't count to six after injecting Ozempic?
Failing to count to six after pressing the dose button can result in medication leaking from the injection site, meaning you receive less than your prescribed dose. This may compromise blood sugar control and treatment effectiveness.
Can I reuse Ozempic needles to save money?
No, never reuse Ozempic needles. Reusing needles increases infection risk, causes painful injections due to blunting, and may affect dose accuracy through medication leakage or blockage. Always use a new needle for each injection and dispose of it safely in a sharps container.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript