Starting a GLP-1 receptor agonist for type 2 diabetes or weight management marks an important step in your treatment journey. During your first week on medications such as semaglutide (Ozempic, Wegovy), liraglutide (Victoza, Saxenda), or dulaglutide (Trulicity), you will likely notice changes in appetite, digestion, and possibly blood glucose levels. Understanding what to expect—from common gastrointestinal side effects like nausea and bloating to early appetite suppression—can help you navigate this adjustment period with confidence. This guide outlines the typical first-week experience, practical management strategies, and when to seek medical advice, ensuring you are well-prepared as your body adapts to GLP-1 therapy.
Summary: During your first week on GLP-1 medications, you can expect reduced appetite, gastrointestinal side effects such as nausea and bloating, and possible modest weight changes as your body adjusts to the treatment.
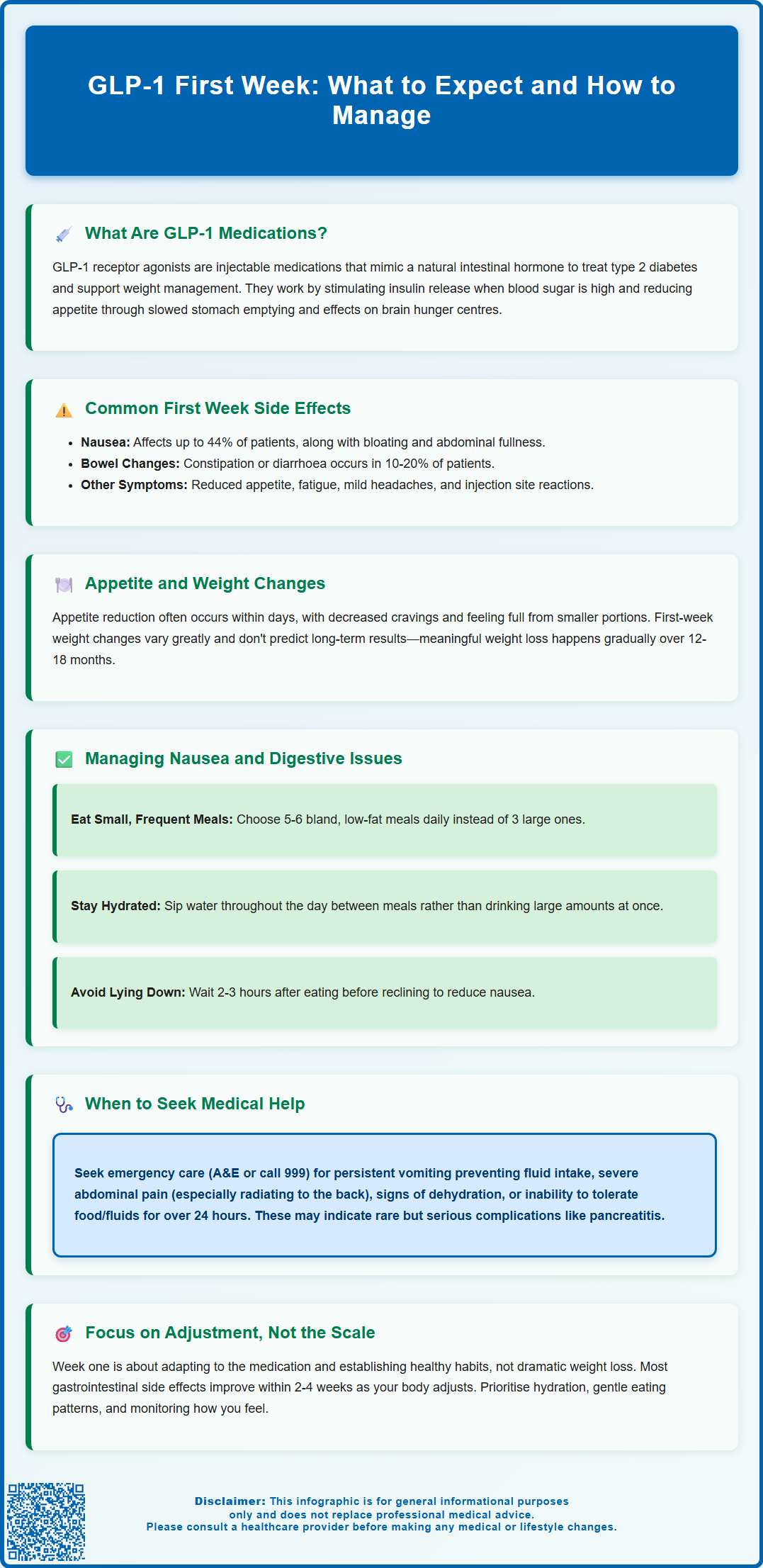
- GLP-1 receptor agonists mimic a natural gut hormone that regulates blood sugar, slows gastric emptying, and reduces appetite through central and peripheral mechanisms.
- Nausea is the most common first-week side effect, affecting up to 44% of patients on higher doses, alongside bloating, constipation, or diarrhoea, which typically diminish over 2–4 weeks.
- Appetite suppression often occurs within days, leading to early satiety and reduced food intake, though initial weight changes vary widely and are not indicative of long-term results.
- Eating smaller, frequent meals, avoiding high-fat foods, staying upright after eating, and maintaining hydration help minimise gastrointestinal symptoms during the adjustment period.
- Seek urgent medical attention for persistent vomiting, severe abdominal pain radiating to the back, signs of dehydration, or symptoms suggesting pancreatitis or gallbladder complications.
- Patients taking insulin or sulfonylureas alongside GLP-1 therapy should monitor blood glucose carefully due to increased hypoglycaemia risk and may require dose adjustments.
Table of Contents
What Are GLP-1 Medications and How Do They Work?
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications originally developed for type 2 diabetes management, with some now specifically licensed for weight management in the UK. These injectable medicines include semaglutide (Ozempic for diabetes; Wegovy for weight management), liraglutide (Victoza for diabetes; Saxenda for weight management), and dulaglutide (Trulicity for diabetes only). The National Institute for Health and Care Excellence (NICE) has approved certain GLP-1 medications for specific indications, with weight management treatments typically initiated in specialist services following NICE criteria.
GLP-1 medications work by mimicking a naturally occurring hormone produced in the intestines after eating. This hormone plays several crucial roles in metabolic regulation. Firstly, it stimulates insulin secretion from the pancreas in a glucose-dependent manner, meaning insulin is only released when blood sugar levels are elevated. While this mechanism reduces the risk of hypoglycaemia compared to some other diabetes medications, patients taking GLP-1s alongside insulin or sulfonylureas should be aware of an increased risk of low blood sugar and may need dose adjustments of these other medications.
GLP-1 receptor agonists also suppress glucagon release, a hormone that raises blood glucose levels, thereby helping to maintain more stable blood sugar throughout the day.
Beyond glycaemic effects, GLP-1 receptor agonists slow gastric emptying, which means food remains in the stomach longer, promoting feelings of fullness and satiety. They also act on appetite centres in the brain, particularly the hypothalamus, reducing hunger signals and food cravings. This dual action on both peripheral and central appetite regulation explains their effectiveness for weight management.
When starting GLP-1 therapy, patients typically begin with a low dose that is gradually increased over several weeks, as outlined in the Summary of Product Characteristics (SmPC) for each medication. This gradual dose escalation helps minimise side effects whilst allowing the body to adjust to the medication's effects.
Importantly, GLP-1 medications are not indicated for type 1 diabetes. If you are pregnant, planning pregnancy, or breastfeeding, you should discuss the risks and benefits with your healthcare provider, as these medications are generally not recommended during pregnancy.
Common Side Effects During Your First Week on GLP-1
During the first week of GLP-1 therapy, most patients experience some degree of gastrointestinal side effects, which are the most frequently reported adverse reactions with this medication class. These effects occur because GLP-1 receptor agonists fundamentally alter digestive processes, particularly gastric emptying rates. Clinical trials consistently demonstrate that gastrointestinal symptoms are most pronounced during the initial weeks of treatment and typically diminish as the body adapts to the medication.
Nausea is the most common side effect, with frequency varying by specific medication and dose. For example, nausea affects up to 44% of patients on the highest dose of semaglutide (Wegovy), though rates are typically lower at starting doses. This sensation may range from mild queasiness to more pronounced nausea, particularly after meals. Alongside nausea, many patients report feelings of abdominal fullness or bloating, even after consuming smaller portions than usual. Some individuals experience mild abdominal discomfort or cramping, which generally resolves within the first few weeks of treatment.
Other gastrointestinal effects during week one may include:
-
Constipation or diarrhoea – bowel habit changes affect roughly 10–20% of patients
-
Reduced appetite – often marked and may feel unusual initially
-
Indigestion or acid reflux – particularly when lying down after eating
-
Fatigue or mild headache – possibly related to dietary changes or adjustment period
Injection site reactions such as redness, itching, or mild swelling may occur but are generally minor and resolve quickly. It is important to rotate injection sites (abdomen, thigh, or upper arm) to minimise these reactions.
For patients with diabetes who are also taking insulin or sulfonylureas, there is an increased risk of hypoglycaemia. Monitor your blood glucose levels carefully and discuss potential dose adjustments of these medications with your healthcare provider.
Most side effects during the first week are mild to moderate in severity and do not require discontinuation of therapy. However, you should contact your GP for persistent symptoms, NHS 111 for urgent concerns, or attend A&E if you experience severe, persistent vomiting, signs of dehydration (dark urine, dizziness, reduced urination), severe abdominal pain (especially if radiating to the back), or symptoms of gallbladder problems (severe upper right abdominal pain, fever, yellowing of skin/eyes). These could indicate serious complications such as pancreatitis or acute kidney injury, though such occurrences are uncommon during the initial low-dose phase.
You can report any suspected side effects to the MHRA Yellow Card Scheme at yellowcard.mhra.gov.uk.
What to Expect: Appetite Changes and Weight Loss in Week One
One of the most immediate and noticeable effects of starting GLP-1 therapy is a reduction in appetite, which many patients experience within the first few days of their initial injection. This appetite suppression can feel quite profound and sometimes unexpected in its intensity. Patients frequently report that foods they previously found appealing no longer hold the same interest, and the constant thoughts about food or snacking urges that may have been present before treatment often diminish significantly.
During the first week, you may notice that you feel satisfied with considerably smaller portions than you typically consumed. Meals that would have left you wanting more now leave you feeling comfortably full, sometimes even uncomfortably so if you attempt to eat your usual portion sizes. This sensation of early satiety occurs because GLP-1 slows gastric emptying, meaning food remains in your stomach longer, triggering fullness signals more readily. Some patients describe feeling full for several hours after eating, with reduced interest in snacking between meals.
Regarding weight loss in the first week, expectations should be realistic and individualised. Early weight changes vary widely between individuals, with some experiencing modest weight reduction while others may see little or no change initially. Any early weight changes may be attributed to:
-
Reduced caloric intake due to appetite suppression
-
Decreased fluid retention in some individuals
-
Changes in glycogen stores and associated water weight
-
Reduced food volume in the digestive system
It is important to understand that week one weight changes are not indicative of long-term results. GLP-1 medications are designed for gradual, sustained weight loss over months, not rapid reduction. According to NICE guidance and clinical trials, clinically meaningful weight loss occurs over several months of treatment, with continued weight reduction possible over 12–18 months when combined with lifestyle modifications. The specific continuation criteria for treatment vary by product and are outlined in the respective NICE technology appraisals.
Patients should focus on adjusting to the medication during the first week rather than fixating on the scales. Establishing healthy eating patterns, staying adequately hydrated, and monitoring how your body responds to the medication are more important initial goals than achieving specific weight loss targets.
Managing Nausea and Digestive Symptoms on GLP-1
Successfully managing gastrointestinal side effects during your first week on GLP-1 therapy can significantly improve your treatment experience and adherence. Practical dietary modifications represent the first-line approach to minimising nausea and digestive discomfort. These strategies work with the medication's mechanism of action rather than against it.
Dietary strategies to reduce nausea include:
-
Eat smaller, more frequent meals – consuming 5–6 small meals rather than 3 large ones prevents overwhelming your slowed digestive system
-
Avoid high-fat foods – fatty meals delay gastric emptying further and can exacerbate nausea and bloating
-
Choose bland, easily digestible foods – plain crackers, toast, rice, bananas, and clear soups are generally well-tolerated
-
Eat slowly and chew thoroughly – taking time with meals allows your body to register fullness signals before overeating
-
Stop eating when comfortably satisfied – continuing to eat despite fullness signals often triggers nausea
-
Avoid lying down immediately after eating – remain upright for at least 2–3 hours after meals to facilitate digestion
Hydration management is equally important. Sip water throughout the day rather than consuming large volumes at once. Some patients find that drinking fluids between meals rather than with meals reduces feelings of excessive fullness. Ginger tea or peppermint tea may provide natural relief from nausea for some individuals, though there is no official link established through clinical trials specific to GLP-1-induced nausea.
For constipation, which affects some patients, increasing dietary fibre gradually (fruits, vegetables, whole grains) and maintaining adequate fluid intake usually provides relief. If constipation persists beyond a few days, speak with your pharmacist about appropriate over-the-counter remedies.
If you have diabetes and are also taking insulin or sulfonylureas, monitor your blood glucose levels regularly, as your requirements for these medications may decrease. Always carry fast-acting carbohydrates (like glucose tablets or fruit juice) in case of hypoglycaemia, and discuss dose adjustments with your healthcare provider.
When to seek medical advice:
-
Contact your GP for persistent but non-urgent symptoms
-
Use NHS 111 for urgent concerns
-
Attend A&E or call 999 for:
- Persistent vomiting preventing adequate fluid intake
- Signs of dehydration (dark urine, dizziness, dry mouth, decreased urination)
- Severe abdominal pain, particularly if radiating to the back (possible pancreatitis)
- Upper right abdominal pain with fever or jaundice (possible gallbladder issues)
- Severe allergic reaction
- Inability to tolerate any food or fluids for more than 24 hours
Your prescribing clinician may consider delaying dose escalation or temporarily reducing the dose if side effects are particularly troublesome, as outlined in the SmPC. Most patients find that gastrointestinal symptoms improve significantly after the first 2–4 weeks as their body adapts to the medication. Patience during this adjustment period, combined with appropriate dietary modifications, usually results in successful tolerance of GLP-1 therapy and achievement of therapeutic goals.
Frequently Asked Questions
Will I lose weight in my first week on GLP-1 medication?
Weight changes during the first week vary widely between individuals, with some experiencing modest reduction whilst others see little or no change initially. Clinically meaningful weight loss occurs gradually over several months of treatment combined with lifestyle modifications, so first-week results are not indicative of long-term outcomes.
How long does nausea last when starting GLP-1 therapy?
Nausea is most pronounced during the initial weeks of GLP-1 treatment and typically diminishes significantly after 2–4 weeks as your body adapts to the medication. Eating smaller, frequent meals and avoiding high-fat foods can help manage symptoms during this adjustment period.
When should I seek medical help for GLP-1 side effects?
Attend A&E or call 999 if you experience persistent vomiting preventing fluid intake, severe abdominal pain (especially radiating to the back), signs of dehydration, upper right abdominal pain with fever or jaundice, or inability to tolerate food or fluids for more than 24 hours. Contact your GP for persistent but non-urgent symptoms or NHS 111 for urgent concerns.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












