Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes management, though Wegovy is the preparation specifically approved for weight management. When prescribed appropriately, semaglutide can facilitate weight loss by reducing appetite and slowing gastric emptying. However, medication alone is insufficient—NICE guidance emphasises that semaglutide must be combined with structured dietary modification and lifestyle interventions. A well-planned meal approach maximises therapeutic benefits whilst minimising gastrointestinal side effects. This article explores evidence-based nutritional strategies for individuals using semaglutide under medical supervision, focusing on balanced nutrition, symptom management, and sustainable eating habits aligned with UK clinical guidance.
Summary: An Ozempic meal plan for weight loss should prioritise nutrient-dense foods including lean proteins, complex carbohydrates, abundant vegetables, and healthy fats in smaller, frequent portions to maximise therapeutic benefits whilst minimising gastrointestinal side effects.
- Semaglutide is a GLP-1 receptor agonist that reduces appetite and slows gastric emptying; Wegovy (not Ozempic) is licensed for weight management in the UK.
- Each meal should contain lean protein (20–30g), complex carbohydrates, non-starchy vegetables (half the plate), and moderate healthy fats.
- Common gastrointestinal side effects include nausea, constipation, and diarrhoea, which can be managed through smaller meals, adequate hydration, and strategic food choices.
- NICE guidance recommends semaglutide only as part of specialist weight management services with concurrent behavioural interventions and dietary counselling.
- Regular monitoring of weight, body measurements, and symptoms is essential, with professional support from registered dietitians for optimal outcomes and safety.
Table of Contents
How Ozempic Works for Weight Loss
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed by the MHRA specifically for managing type 2 diabetes mellitus. While it can cause weight loss, it is important to note that Wegovy (semaglutide 2.4 mg) is the preparation specifically licensed for chronic weight management in the UK.
The mechanism of action centres on mimicking the naturally occurring GLP-1 hormone, which is released from the gut in response to food intake. Semaglutide binds to GLP-1 receptors in multiple tissues, including the pancreas, gastrointestinal tract, and brain. In the pancreas, it enhances glucose-dependent insulin secretion and suppresses inappropriate glucagon release, thereby improving glycaemic control. Crucially for weight loss, semaglutide acts on appetite-regulating centres in the hypothalamus, reducing hunger and increasing satiety signals. It also slows gastric emptying, prolonging the sensation of fullness after meals.
Clinical trials with Wegovy 2.4 mg have demonstrated substantial weight reduction—typically 15% of baseline body weight over 68 weeks in people without diabetes (somewhat less in those with type 2 diabetes) when combined with lifestyle interventions. The medication does not directly burn fat or increase metabolism; rather, it facilitates weight loss by making it easier to adhere to a reduced-calorie diet through appetite suppression.
It is essential to understand that semaglutide is not a standalone solution. NICE guidance (TA875) recommends Wegovy only as part of a specialist weight management service for people with specific BMI thresholds and weight-related health conditions, typically for a maximum of 2 years on the NHS. The NHS currently advises against using Ozempic off-label for weight loss due to supply shortages affecting people with diabetes. Optimal outcomes require concurrent dietary modification and increased physical activity under appropriate medical supervision.
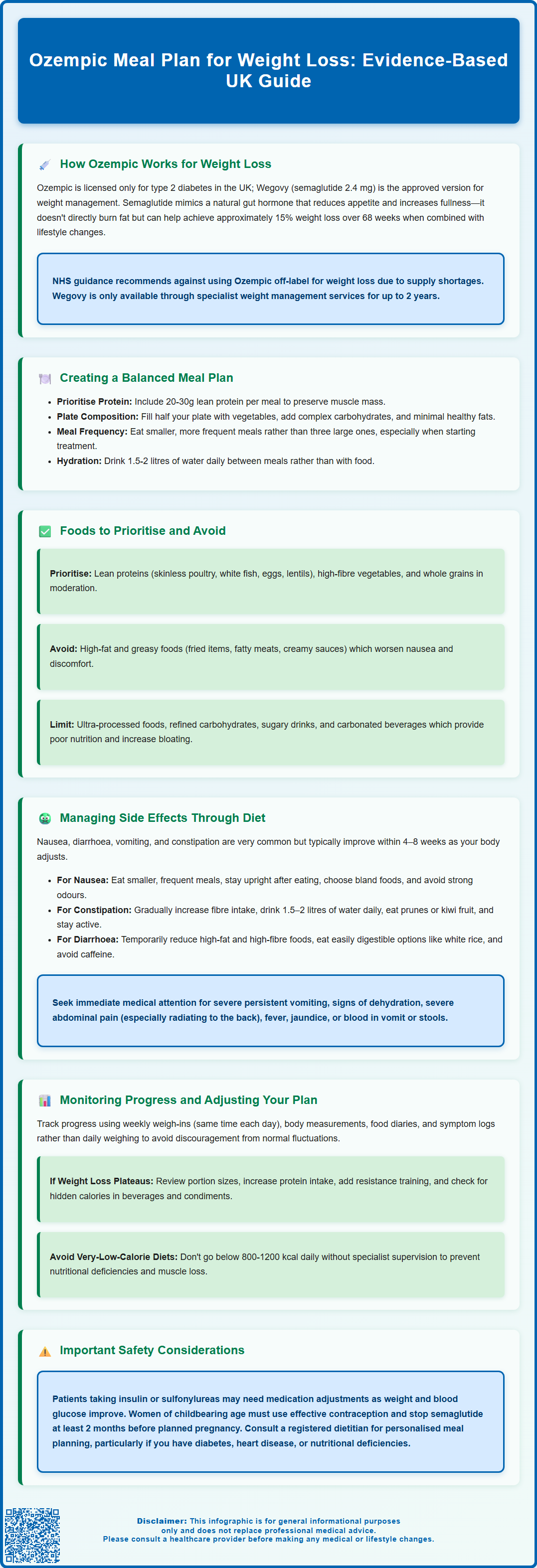
Creating a Balanced Meal Plan While Taking Ozempic
Developing a structured, nutritionally complete meal plan is fundamental to maximising the benefits of semaglutide whilst minimising potential side effects. The medication's appetite-suppressing effects can significantly reduce food intake, making it vital to ensure that every meal provides adequate nutrition despite smaller portion sizes.
A balanced approach should prioritise nutrient density over calorie density. Many people find that smaller, more frequent meals are better tolerated than three larger ones, particularly during dose escalation. Each meal should ideally contain:
-
Lean protein sources (20–30g per meal, adjusted if you have kidney disease): chicken breast, turkey, white fish, eggs, tofu, or low-fat Greek yoghurt
-
Complex carbohydrates (portion-controlled): wholegrain bread, brown rice, quinoa, sweet potato, or oats
-
Abundant vegetables: aim for at least half your plate to comprise non-starchy vegetables
-
Healthy fats in moderation: avocado, nuts, seeds, or olive oil (small quantities due to slower gastric emptying)
Given the reduced gastric capacity and delayed emptying associated with semaglutide, eating slowly and chewing thoroughly helps prevent uncomfortable fullness or nausea. Stopping when comfortably satisfied—rather than completely full—is advisable. During dose escalation, temporarily reducing fat and spicy foods while gradually introducing fibre may help minimise gastrointestinal symptoms.
Hydration deserves particular attention. Aim for 1.5–2 litres of water daily, which many find easier to consume between rather than with meals. The NHS Eatwell Guide provides an excellent framework for balanced nutrition, though portion sizes will naturally decrease. If you consume alcohol, follow UK low-risk drinking guidelines (no more than 14 units weekly, spread over several days with alcohol-free days).
Consider consulting a registered dietitian for personalised guidance, particularly if you have comorbidities such as diabetes, cardiovascular disease, or nutritional deficiencies. NICE guidance emphasises that pharmacological weight management should always be accompanied by evidence-based behavioural interventions and dietary counselling.
Foods to Prioritise and Avoid on Ozempic
Strategic food selection can enhance weight loss outcomes and improve gastrointestinal tolerance whilst taking semaglutide. Understanding which foods to emphasise and which to limit is essential for both efficacy and comfort.
Foods to prioritise:
-
Lean proteins: Essential for preserving muscle mass during weight loss. Options include skinless poultry, white fish (cod, haddock), shellfish, eggs, and plant-based proteins like lentils and chickpeas
-
High-fibre vegetables: Broccoli, spinach, kale, courgettes, peppers, and cauliflower provide volume, micronutrients, and fibre with minimal calories
-
Whole grains in moderation: Porridge oats, wholemeal bread, and brown rice offer sustained energy and prevent blood glucose fluctuations
-
Low-fat dairy or fortified alternatives: Skimmed milk, low-fat yoghurt, reduced-fat cheese, or calcium/iodine-fortified plant-based alternatives provide important nutrients
-
Whole fruits in appropriate portions: Focus on whole fruits rather than juices, limiting fruit juice to 150ml per day as per NHS guidance
Foods to limit or avoid:
-
High-fat, greasy foods: Fried items, fatty cuts of meat, and creamy sauces can exacerbate nausea and delayed gastric emptying, leading to significant discomfort
-
Ultra-processed foods: Crisps, biscuits, and ready meals often contain excessive salt, sugar, and unhealthy fats whilst providing poor nutritional value
-
Refined carbohydrates: White bread, pastries, and sugary cereals cause rapid glucose spikes and provide little satiety
-
Sugar-sweetened beverages: Provide empty calories and can affect blood glucose control
-
Carbonated beverages: Can increase bloating and gastric discomfort, particularly given slower stomach emptying
-
Excessive alcohol: Provides empty calories, may affect blood glucose control, and can intensify gastrointestinal side effects
Portion control remains paramount. Even nutritious foods can cause discomfort if consumed in large quantities. Many patients find that eating from smaller plates helps recalibrate portion expectations. There is no official link between specific foods and reduced semaglutide efficacy, but poor dietary choices will naturally limit weight loss potential regardless of medication use.
Managing Side Effects Through Diet
Gastrointestinal adverse effects are very common with semaglutide, affecting the majority of users to varying degrees. According to the Wegovy SmPC, nausea, diarrhoea, vomiting, and constipation are all very common side effects. These typically diminish over the first 4–8 weeks as the body adjusts, and dietary strategies can significantly improve tolerability.
For nausea management:
-
Eat smaller, more frequent meals rather than three large ones
-
Avoid lying down immediately after eating; remain upright for at least 30 minutes
-
Choose bland, easily digestible foods during symptomatic periods: plain crackers, toast, bananas, or rice
-
Ginger tea or ginger biscuits may provide natural anti-nausea benefits, though evidence is limited
-
Avoid strong food odours and overly spicy or heavily seasoned dishes
-
Stay well-hydrated with small, frequent sips of water throughout the day
For constipation (a common issue given slower gut motility):
-
Gradually increase dietary fibre through vegetables, fruits, and whole grains
-
Ensure adequate fluid intake—at least 1.5–2 litres daily
-
Include prunes, kiwi fruit, or linseeds, which have natural laxative properties
-
Maintain regular physical activity to stimulate bowel function
-
If persistent, speak to your GP about appropriate laxatives; avoid long-term use without medical advice
For diarrhoea:
-
Temporarily reduce high-fat and high-fibre foods
-
Focus on easily digestible options: white rice, boiled potatoes, cooked carrots
-
Maintain hydration and consider oral rehydration solutions if severe
-
Avoid caffeine and artificial sweeteners (particularly sorbitol), which can worsen symptoms
When to seek medical attention: Contact your healthcare provider promptly if you experience severe, persistent vomiting preventing fluid intake, signs of dehydration (reduced urination, dizziness, confusion), severe or persistent abdominal pain (especially if radiating to the back), fever or jaundice (yellowing of skin/eyes), or blood in vomit or stools. These may indicate serious complications such as pancreatitis, gallbladder disease, or acute kidney injury requiring urgent assessment.
If side effects are intolerable, discuss with your prescriber about slowing the dose escalation or temporarily reducing the dose. The MHRA advises reporting any suspected adverse drug reactions through the Yellow Card scheme at yellowcard.mhra.gov.uk.
Monitoring Progress and Adjusting Your Eating Plan
Systematic monitoring and periodic adjustment of your dietary approach are essential for sustained success with semaglutide. Weight loss is rarely linear, and nutritional needs evolve as body composition changes.
Tracking methods to consider:
-
Weekly weigh-ins: Measure at the same time of day (ideally morning, after voiding, before eating) to ensure consistency. Avoid daily weighing, which can be discouraging due to normal fluctuations
-
Body measurements: Waist circumference, hip measurements, and clothing fit often reflect progress when scale weight plateaus
-
Food diary: Recording meals, portion sizes, and associated symptoms helps identify patterns and problematic foods
-
Symptom log: Note gastrointestinal effects, energy levels, and hunger patterns to guide dietary adjustments
Adjusting your plan:
As weight decreases, caloric requirements naturally reduce. However, very-low-energy diets (below 800-1200 kcal daily) are not recommended without specialist supervision, as these risk nutritional deficiencies and muscle loss. If weight loss stalls after initial success, consider:
-
Reviewing portion sizes, which may have gradually increased
-
Increasing protein intake to preserve lean muscle mass
-
Incorporating more physical activity, progressing from walking to resistance training
-
Assessing for "hidden calories" in beverages, condiments, or cooking methods
If you have diabetes and are taking insulin or sulfonylureas, you may need medication adjustments as your weight and blood glucose levels improve. Discuss this with your healthcare team to avoid hypoglycaemia.
It's important to note that Wegovy is typically prescribed for up to 2 years on the NHS as part of a specialist weight management service (per NICE TA875). Developing sustainable eating habits during treatment is crucial for maintaining weight loss after medication discontinuation.
Women of childbearing age should use effective contraception while taking semaglutide and should stop the medication at least 2 months before a planned pregnancy. Semaglutide is not recommended during pregnancy or breastfeeding.
Professional support is invaluable. Regular follow-up with healthcare professionals is recommended to monitor for adverse effects, assess cardiovascular risk factors, and determine appropriate treatment duration. Referral to a registered dietitian is advisable if you have complex nutritional needs, multiple comorbidities, or are struggling with adherence.
Frequently Asked Questions
What foods should I avoid whilst taking Ozempic?
Limit high-fat and greasy foods, ultra-processed items, refined carbohydrates, sugar-sweetened beverages, and excessive alcohol, as these can exacerbate gastrointestinal side effects and provide poor nutritional value. Focus instead on nutrient-dense whole foods in appropriate portions.
How can I manage nausea when taking semaglutide?
Eat smaller, more frequent meals, avoid lying down immediately after eating, choose bland foods during symptomatic periods, stay well-hydrated with small sips throughout the day, and avoid strong food odours or heavily spiced dishes. Nausea typically improves within 4–8 weeks.
Is Ozempic licensed for weight loss in the UK?
No, Ozempic is licensed specifically for type 2 diabetes management. Wegovy (semaglutide 2.4 mg) is the preparation licensed for chronic weight management in the UK and is prescribed through specialist weight management services according to NICE guidance.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












