GLP-1 receptor agonists such as semaglutide and liraglutide significantly reduce appetite and slow digestion, making dietary choices particularly important during treatment. Understanding what to eat on a GLP-1 medicine helps you meet nutritional requirements within smaller portions, manage common gastrointestinal side effects, and support your weight management or diabetes goals. This guide provides evidence-based recommendations on optimal food choices, foods to limit, and practical meal planning strategies tailored to the physiological effects of GLP-1 therapy, aligned with NHS and NICE guidance for safe, effective treatment outcomes.
Summary: Whilst taking GLP-1 medicines, prioritise lean proteins, non-starchy vegetables, complex carbohydrates in moderate portions, and healthy fats, whilst limiting high-fat, ultra-processed, and sugary foods that may worsen side effects or undermine treatment goals.
- GLP-1 receptor agonists suppress appetite, slow gastric emptying, and enhance insulin secretion whilst reducing glucagon release.
- Lean protein sources (20–30g per meal) help preserve muscle mass and promote satiety within reduced stomach capacity.
- Non-starchy vegetables and complex carbohydrates provide essential nutrients, fibre, and sustained energy without overwhelming digestion.
- Common gastrointestinal side effects include nausea, early satiety, constipation, and reflux, manageable through smaller frequent meals and strategic food choices.
- Seek urgent medical advice for severe persistent abdominal pain, vomiting preventing fluid intake for 24 hours, or signs of pancreatitis or gallbladder disease.
Table of Contents
How GLP-1 Medicines Affect Your Appetite and Digestion
Glucagon-like peptide-1 (GLP-1) receptor agonists, including semaglutide (Wegovy, Ozempic) and liraglutide (Saxenda, Victoza), work by mimicking a naturally occurring hormone that regulates blood glucose and appetite. These medicines bind to GLP-1 receptors in the pancreas, brain, and gastrointestinal tract, triggering several physiological responses that support weight management and blood glucose control.
A key mechanism involves acting on appetite centres in the hypothalamus, directly suppressing hunger signals and reducing food cravings. GLP-1 medicines also slow gastric emptying (particularly in early treatment), meaning food remains in your stomach longer, creating a prolonged sensation of fullness after meals and helping you feel satisfied with smaller portions.
These medicines also enhance insulin secretion in response to food intake whilst suppressing glucagon release, which helps stabilise blood glucose levels throughout the day. For individuals with type 2 diabetes, this dual action improves glucose control alongside weight reduction. When used alone, GLP-1 medicines rarely cause hypoglycaemia (low blood sugar), but the risk increases if you also take insulin or sulfonylureas.
The slowed digestion can initially cause gastrointestinal side effects, particularly during dose escalation. Many patients experience nausea, early satiety, bloating, or changes in bowel habits as their digestive system adapts to the medicine.
Importantly, seek urgent medical advice (NHS 111 or A&E) if you experience severe, persistent abdominal pain (especially if radiating to your back), yellowing of skin/eyes, dark urine, pale stools, or inability to keep fluids down for 24 hours. These could indicate serious conditions like pancreatitis or gallbladder disease.
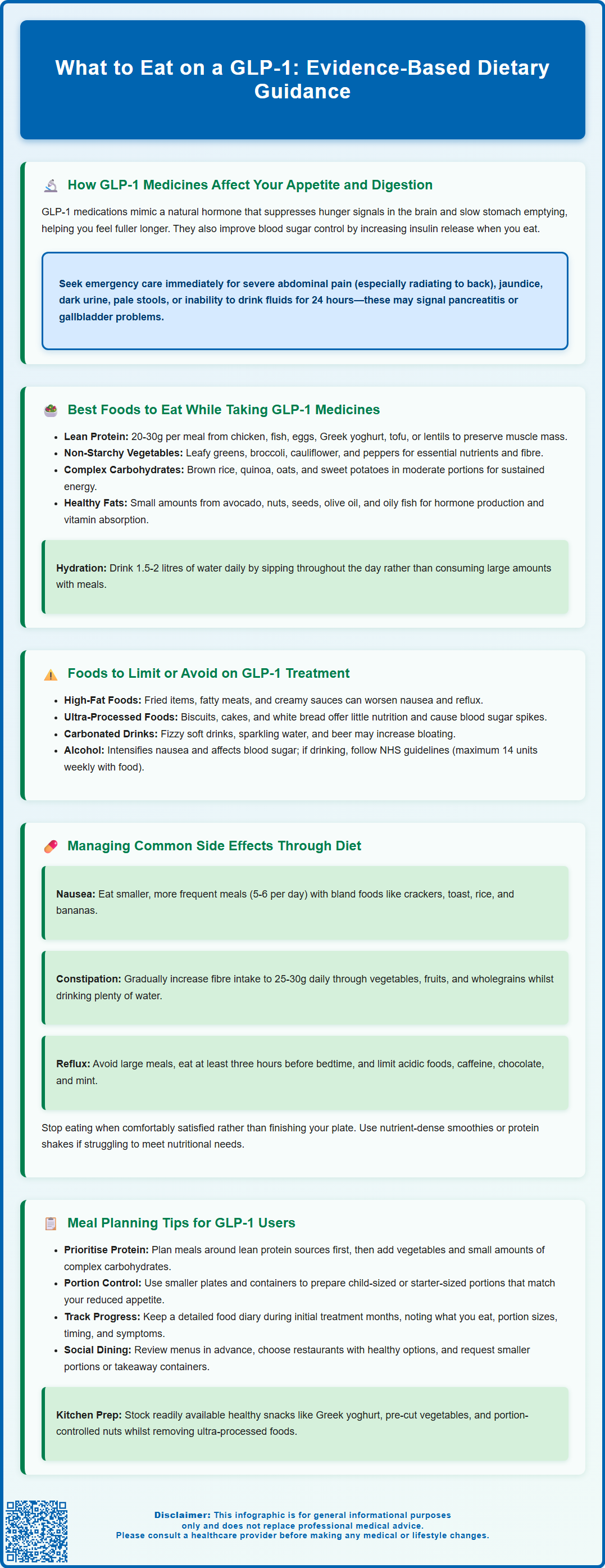
Best Foods to Eat While Taking GLP-1 Medicines
Optimising your diet whilst taking GLP-1 medicines requires focusing on nutrient-dense foods that provide essential vitamins, minerals, and macronutrients within smaller portion sizes. Since these medicines significantly reduce appetite, every bite becomes more important for meeting your nutritional requirements.
Lean protein sources should form the foundation of your meals. Prioritise skinless chicken, turkey, white fish (such as cod or haddock), eggs, Greek yoghurt, and plant-based options like tofu or lentils. Protein helps preserve muscle mass during weight loss, promotes satiety, and supports tissue repair. Aim for 20-30g of protein per meal, though this should be adjusted based on your individual requirements, body size, and kidney function.
Non-starchy vegetables are excellent choices, providing fibre, vitamins, and minerals with minimal calories. Include leafy greens (spinach, kale, rocket), cruciferous vegetables (broccoli, cauliflower, Brussels sprouts), courgettes, peppers, tomatoes, and mushrooms. These foods add volume and nutrients without overwhelming your reduced stomach capacity.
Complex carbohydrates in moderate portions help maintain energy levels and provide sustained glucose release. Choose wholegrain options such as brown rice, quinoa, oats, wholemeal bread, and sweet potatoes. These foods contain more fibre than refined alternatives, supporting digestive health and blood glucose stability.
Healthy fats in controlled amounts are essential for hormone production, vitamin absorption, and satiety. Include small portions of avocado, nuts, seeds, olive oil, and oily fish like salmon or mackerel, which also provide omega-3 fatty acids.
Hydration remains crucial—aim for 1.5-2 litres of water daily (unless advised otherwise by your healthcare professional if you have heart or kidney problems), sipping throughout the day rather than drinking large amounts with meals, which can increase feelings of fullness and discomfort.
For balanced meal planning, the NHS Eatwell Guide provides helpful visual guidance on portion sizes and food group proportions.
Foods to Limit or Avoid on GLP-1 Treatment
Certain foods may exacerbate side effects or undermine your treatment goals whilst taking GLP-1 medicines. Understanding which foods to limit helps you navigate your dietary choices more effectively and maintain comfort throughout your treatment journey.
High-fat foods may be problematic for some people, as they can further delay gastric emptying when combined with GLP-1 medicines. Consider limiting fried foods, fatty cuts of meat, pastries, and creamy sauces if you notice they trigger or worsen nausea, cause prolonged feelings of uncomfortable fullness, or lead to reflux or indigestion. Tolerance varies between individuals, so you may find you can include moderate amounts of healthy fats without discomfort.
Ultra-processed foods high in refined sugars and simple carbohydrates are best minimised. Biscuits, cakes, sweets, sugary cereals, and white bread provide minimal nutritional value whilst occupying valuable stomach capacity. These foods can also cause rapid blood glucose fluctuations, counteracting the glycaemic benefits of GLP-1 therapy.
Carbonated beverages may increase bloating and gastric discomfort for some people, particularly when stomach emptying is already delayed. If you notice symptoms, consider reducing fizzy soft drinks, sparkling water, and beer. However, if you tolerate them well, there's no need to avoid them completely.
Spicy and highly seasoned foods may irritate the digestive system, especially during the initial treatment phases when gastrointestinal sensitivity is heightened. Whilst tolerance varies individually, consider moderating very spicy curries, hot sauces, and heavily seasoned dishes if you experience increased nausea or reflux.
Alcohol warrants particular caution. It can intensify nausea, interact with blood glucose regulation, and provides empty calories that may impede weight loss goals. If you choose to drink, do so in moderation and always with food, following NHS guidelines of no more than 14 units weekly, spread over three or more days with several alcohol-free days. Avoid alcohol completely if you're experiencing significant side effects or poor food intake.
Managing Common Side Effects Through Diet
Gastrointestinal side effects are the most frequently reported adverse reactions to GLP-1 medicines, but strategic dietary modifications can significantly reduce their impact and improve treatment tolerance.
For nausea management, eat smaller, more frequent meals rather than three large ones. Many patients find success with five to six small meals throughout the day. Choose bland, easily digestible foods during periods of increased nausea—plain crackers, toast, rice, bananas, and clear broths are often well-tolerated. Ginger tea or ginger biscuits may provide natural relief. Avoid lying down immediately after eating, and try to identify specific trigger foods that worsen your symptoms. Cold or room-temperature foods are sometimes better tolerated than hot meals when nausea is prominent.
Constipation affects many GLP-1 users due to slowed intestinal transit. Increase your fibre intake gradually through vegetables, fruits, wholegrains, and legumes, aiming for 25-30g daily. Ensure adequate hydration—water helps fibre work effectively in your digestive system. Prunes, kiwi fruit, and linseeds can be particularly helpful. Regular physical activity also promotes healthy bowel function.
Diarrhoea may occur in some people. If this happens, maintain hydration with regular sips of water or oral rehydration solutions. Temporarily reducing fibre and fat intake may help, focusing on plain foods like rice, toast, and bananas until symptoms improve.
Reflux and heartburn can be minimised by avoiding large meals, especially before bedtime. Eat your last meal at least three hours before lying down, and consider elevating the head of your bed. Limit acidic foods (citrus, tomatoes), caffeine, chocolate, and mint if these trigger symptoms.
Early satiety requires patience and adjustment. Stop eating when you feel comfortably satisfied, even if food remains on your plate. Eating beyond fullness often triggers nausea and discomfort. If you struggle to meet nutritional needs, consider nutrient-dense smoothies or protein shakes between meals.
If you also take insulin or sulfonylureas, monitor your blood glucose more frequently, as GLP-1 medicines can increase the risk of hypoglycaemia. Treat low blood sugar (below 4 mmol/L) with 15-20g of fast-acting carbohydrate (like glucose tablets or fruit juice), followed by a longer-acting carbohydrate snack.
Seek urgent medical help (NHS 111 or A&E) if you experience severe, persistent abdominal pain (especially radiating to your back), vomiting that prevents fluid intake for over 24 hours, yellowing of skin/eyes, or minimal urine output. Contact your GP if side effects persist despite dietary modifications or significantly impact your quality of life.
Meal Planning Tips for GLP-1 Users
Successful long-term management on GLP-1 medicines requires thoughtful meal planning that accommodates your reduced appetite whilst ensuring adequate nutrition. These practical strategies can help you establish sustainable eating patterns.
Prioritise protein at every meal. With limited stomach capacity, ensuring adequate protein intake prevents muscle loss during weight reduction. Plan meals around a protein source first, then add vegetables and a modest portion of complex carbohydrates. Batch-cooking lean proteins at the beginning of the week—grilled chicken breasts, hard-boiled eggs, or baked fish—makes meal assembly quicker and ensures you always have nutritious options available.
Prepare smaller portions and use smaller plates to avoid food waste and the pressure to finish large servings. Many patients find that child-sized portions or starter-sized meals are more appropriate for their reduced appetite. Consider investing in smaller storage containers for meal prep, which naturally limit portion sizes.
Keep a food diary during your initial treatment months. Record what you eat, portion sizes, timing, and any symptoms experienced. This information helps identify patterns, trigger foods, and optimal eating schedules. Share this diary with your healthcare provider during follow-up appointments.
Plan for social situations by reviewing restaurant menus in advance, choosing establishments with healthy options, and not feeling obligated to finish meals. Many patients successfully request smaller portions or ask for a takeaway container for leftovers.
Stock your kitchen strategically. Keep readily available healthy snacks like Greek yoghurt, pre-cut vegetables with hummus, nuts in portion-controlled bags, and protein-rich options. Remove or limit ultra-processed foods that may tempt you during vulnerable moments.
Consider nutritional supplementation only if you struggle to meet requirements through food alone. A food-first approach is always preferable, but if your intake remains consistently low, discuss with your GP or a registered dietitian who can assess your individual needs. Avoid high-dose supplements unless specifically recommended by a healthcare professional.
If you experience persistent difficulty maintaining adequate nutrition or unintentional weight loss, ask your GP about a referral to an NHS dietitian for personalised advice. You can also report any suspected side effects from your medicine through the MHRA Yellow Card scheme.
Frequently Asked Questions
How much protein should I eat whilst taking GLP-1 medicines?
Aim for 20–30g of protein per meal from lean sources like chicken, fish, eggs, Greek yoghurt, or plant-based options. Adequate protein helps preserve muscle mass during weight loss and promotes satiety within your reduced stomach capacity.
Can I drink alcohol whilst on GLP-1 treatment?
Alcohol should be consumed with caution, as it can intensify nausea and interfere with blood glucose regulation. If you choose to drink, follow NHS guidelines of no more than 14 units weekly with food, and avoid alcohol completely if experiencing significant side effects.
What should I do if I feel too full to eat enough food on GLP-1 medicines?
Eat smaller, more frequent meals (five to six daily) and prioritise nutrient-dense foods, especially protein. Consider nutrient-rich smoothies or protein shakes between meals, and consult your GP about a dietitian referral if you struggle to maintain adequate nutrition.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript