Glucagon-like peptide-1 (GLP-1) receptor agonists are increasingly prescribed for type 2 diabetes and weight management in the UK. Understanding how long it takes for GLP-1 to kick in helps set realistic expectations for treatment outcomes. The timeframe varies depending on the specific medication, the therapeutic effect being measured, and individual patient factors. Blood glucose improvements may be noticed within days, whilst appetite suppression and weight changes typically emerge over several weeks. This article explores the onset of action for GLP-1 medications, factors influencing response times, and what to expect during your initial treatment period.
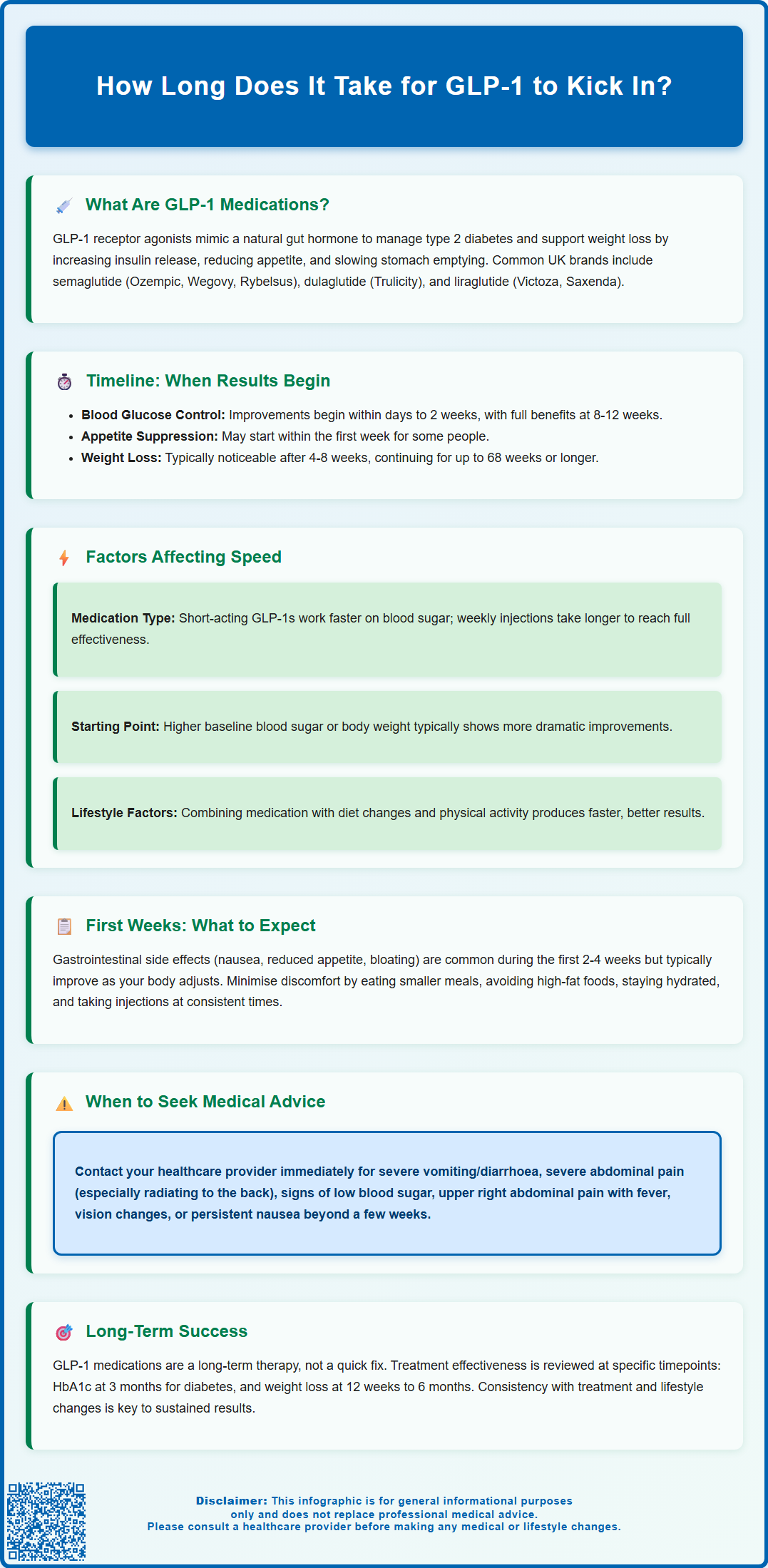
Summary: GLP-1 medications typically begin improving blood glucose control within days to two weeks, with full glycaemic benefits developing over 8 to 12 weeks as doses are gradually increased.
- GLP-1 receptor agonists work by enhancing insulin secretion, suppressing glucagon release, slowing gastric emptying, and reducing appetite through action on brain appetite centres.
- Appetite suppression may be noticed within the first week, whilst meaningful weight loss generally becomes apparent after 4 to 8 weeks of consistent treatment.
- Medications are initiated at low doses and gradually increased over several weeks to minimise gastrointestinal side effects such as nausea and vomiting.
- Individual response varies based on medication formulation, baseline metabolic status, adherence to lifestyle modifications, and gastrointestinal tolerance.
- Common early side effects include nausea, reduced appetite, and altered bowel habits, which typically diminish as the body adapts to treatment.
- Severe abdominal pain, persistent vomiting, or signs of hypoglycaemia require prompt medical attention during the initial treatment period.
Table of Contents
What Are GLP-1 Medications and How Do They Work?
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications primarily used to manage type 2 diabetes and, more recently, for weight management in certain patient groups. These medicines mimic the action of naturally occurring GLP-1, a hormone produced in the intestine that plays a crucial role in regulating blood glucose levels and appetite.
GLP-1 medications work through several complementary mechanisms:
-
Enhancing insulin secretion: They stimulate the pancreas to release insulin when blood glucose levels are elevated, helping to lower blood sugar in a glucose-dependent manner
-
Suppressing glucagon release: They reduce the secretion of glucagon, a hormone that raises blood glucose, thereby preventing excessive glucose production by the liver
-
Slowing gastric emptying: They delay the rate at which food leaves the stomach, leading to more gradual glucose absorption and increased feelings of fullness
-
Reducing appetite: They act on areas of the brain involved in appetite regulation, helping to decrease food intake
Commonly prescribed GLP-1 receptor agonists in the UK include semaglutide (Ozempic for diabetes, Wegovy for weight management, Rybelsus as an oral formulation), dulaglutide (Trulicity), liraglutide (Victoza for diabetes, Saxenda for weight management), and exenatide (Byetta, Bydureon). Most are administered via subcutaneous injection.
For type 2 diabetes, NICE guidance (NG28) recommends GLP-1 RAs based on individual factors including comorbidities, prior treatments, and HbA1c targets. For weight management, NICE technology appraisals (TA875 for Wegovy, TA664 for Saxenda) specify these treatments should be used within specialist weight management services (tier 3 or 4), with specific eligibility criteria, time-limited use, and defined stopping rules.
GLP-1 RAs are not indicated for type 1 diabetes and should not be used during pregnancy or breastfeeding unless the benefits clearly outweigh potential risks.
How Long Does It Take for GLP-1 to Start Working?
The timeframe for GLP-1 medications to 'kick in' varies depending on what therapeutic effect you're measuring and which specific medication you're taking. For blood glucose control, many patients notice improvements within the first few days to two weeks of treatment, as the medication begins to enhance insulin secretion and suppress glucagon release. However, the full glycaemic benefits typically develop over 8 to 12 weeks as the body adjusts to the medication and dose titration progresses.
For appetite suppression and weight loss, the timeline can differ slightly. Some individuals report reduced hunger and earlier satiety within the first week of treatment, whilst others may not notice significant changes until several weeks into therapy. Meaningful weight loss generally becomes apparent after 4 to 8 weeks, with continued weight reduction over several months. Clinical trials have shown that weight loss may continue for up to 68 weeks or longer with consistent treatment.
It's important to understand that GLP-1 medications are initiated at a low dose and gradually increased over several weeks to minimise gastrointestinal side effects such as nausea and vomiting. This dose escalation schedule means that you may not experience the full therapeutic effects until you reach the maintenance dose. For example:
-
Semaglutide for diabetes (Ozempic) typically starts at 0.25 mg weekly for 4 weeks, then 0.5 mg weekly, potentially increasing to 1 mg weekly
-
Semaglutide for weight management (Wegovy) follows a different schedule, starting at 0.25 mg and increasing through 0.5 mg, 1.0 mg, 1.7 mg to a maintenance dose of 2.4 mg weekly
For diabetes treatment, your healthcare team will typically review your HbA1c after about 3 months. For weight management medications, NICE guidance specifies different stopping rules—for example, Wegovy treatment should be reviewed after 6 months, and Saxenda should be discontinued if less than 5% weight loss is achieved after 12 weeks at the maintenance dose.
Factors That Affect How Quickly GLP-1 Takes Effect
Several individual and medication-specific factors influence how rapidly you'll experience the benefits of GLP-1 therapy:
Medication formulation and dosing frequency play a significant role. Short-acting GLP-1 agonists like exenatide (taken twice daily) may produce more immediate effects on post-meal glucose levels, whilst longer-acting weekly formulations such as semaglutide or dulaglutide provide more sustained action but may take longer to reach steady-state concentrations in the body. Oral semaglutide has different absorption characteristics compared to injectable forms, which can affect the onset of action.
Your baseline metabolic status significantly impacts treatment response. Individuals with higher baseline HbA1c levels or greater insulin resistance may experience more dramatic improvements in blood glucose control, though it may take longer to achieve target levels. Similarly, those with higher starting body weight may see more substantial weight loss, but the rate of loss varies considerably between individuals.
Adherence to lifestyle modifications is crucial. GLP-1 medications work synergistically with dietary changes and physical activity. Patients who implement calorie reduction and increase their activity levels typically experience faster and more pronounced benefits than those relying on medication alone. NICE guidelines emphasise that GLP-1 therapy should be part of a comprehensive weight management or diabetes care programme.
Gastrointestinal tolerance can affect dose escalation speed. Some patients experience significant nausea, vomiting, or diarrhoea during the initial weeks, which may necessitate slower dose increases or temporary dose reductions. This can delay reaching the therapeutic dose and, consequently, the full clinical benefits.
Concomitant medications may also influence response. GLP-1 RAs can delay gastric emptying, potentially affecting the absorption of some oral medications. Additionally, renal function is important to consider, particularly with exenatide, which is not recommended for patients with severe renal impairment (eGFR <30 mL/min/1.73 m²).
What to Expect During Your First Weeks on GLP-1 Treatment
Understanding what to anticipate during the initial phase of GLP-1 therapy can help you manage expectations and identify any concerning symptoms that require medical attention.
Common early experiences include gastrointestinal side effects, which are the most frequently reported adverse reactions. During the first 2 to 4 weeks, you may experience:
-
Nausea: Often most pronounced after meals, typically improving over time
-
Reduced appetite: You may feel full more quickly and have less interest in food
-
Mild abdominal discomfort: Bloating or a feeling of fullness
-
Altered bowel habits: Either constipation or loose stools
-
Fatigue: Some patients report tiredness as their body adjusts
These effects are generally mild to moderate and tend to diminish as your body adapts to the medication. Taking your injection at the same time each day/week, eating smaller meals, avoiding high-fat foods, and staying well-hydrated can help minimise discomfort. Remember to rotate injection sites to prevent lipohypertrophy (fatty lumps under the skin).
Monitoring and follow-up are essential during the initial treatment period. Your healthcare team will typically schedule reviews to assess your response, check for adverse effects, and adjust your dose accordingly. You should monitor your blood glucose levels as advised (particularly if you're taking other diabetes medications) and never adjust insulin or sulfonylurea doses without healthcare professional guidance, as this could increase hypoglycaemia risk.
When to seek medical advice: Contact your GP or diabetes specialist promptly if you experience:
-
Severe, persistent vomiting or diarrhoea leading to dehydration
-
Severe abdominal pain, particularly if radiating to the back (potential pancreatitis)
-
Signs of hypoglycaemia (if taking insulin or sulphonylureas concurrently)
-
Symptoms of gallbladder problems (pain in the upper right abdomen, fever, yellowing of skin)
-
Any changes in vision (rapid improvement in blood glucose can sometimes worsen diabetic retinopathy)
-
Unexplained persistent nausea beyond the first few weeks
If you are planning pregnancy, discuss this with your healthcare provider as GLP-1 RAs are not recommended during pregnancy or breastfeeding. For semaglutide specifically, it's advised to stop treatment at least 2 months before a planned pregnancy.
If you experience any suspected side effects, you can report them via the MHRA Yellow Card scheme at yellowcard.mhra.gov.uk or through the Yellow Card app.
Remember that GLP-1 therapy is a long-term commitment, and patience during the initial adjustment period is important. Most patients find that side effects become manageable and the therapeutic benefits become increasingly apparent as treatment continues.
Frequently Asked Questions
Can I expect to see weight loss in the first week of GLP-1 treatment?
Some individuals notice reduced appetite within the first week, but meaningful weight loss typically becomes apparent after 4 to 8 weeks of treatment. GLP-1 medications start at low doses that are gradually increased, so full therapeutic effects develop over time as you reach the maintenance dose.
Why do GLP-1 medications need to be started at a low dose?
GLP-1 medications are initiated at low doses and gradually increased to minimise gastrointestinal side effects such as nausea and vomiting. This dose escalation schedule allows your body to adapt to the medication whilst reducing the likelihood of troublesome adverse reactions.
When should I contact my doctor whilst taking GLP-1 medication?
Contact your GP or diabetes specialist promptly if you experience severe persistent vomiting or diarrhoea, severe abdominal pain (particularly radiating to the back), signs of hypoglycaemia, symptoms of gallbladder problems, vision changes, or unexplained persistent nausea beyond the first few weeks.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












