Arm soreness after Ozempic injection is a recognised local reaction affecting some patients using this GLP-1 receptor agonist for type 2 diabetes management. Whilst typically mild and self-limiting, understanding why this discomfort occurs and how to minimise it can improve treatment adherence and patient comfort. This article examines the mechanisms behind injection site soreness, evidence-based techniques to reduce pain, warning signs requiring medical attention, optimal injection sites and methods, and comprehensive side effect management strategies. Guidance is based on UK regulatory information and clinical best practice to support safe, effective Ozempic therapy.
Summary: Arm soreness after Ozempic injection is a mild, self-limiting local reaction caused by needle insertion and inflammatory response in subcutaneous tissue.
- Ozempic is a GLP-1 receptor agonist administered subcutaneously for type 2 diabetes management
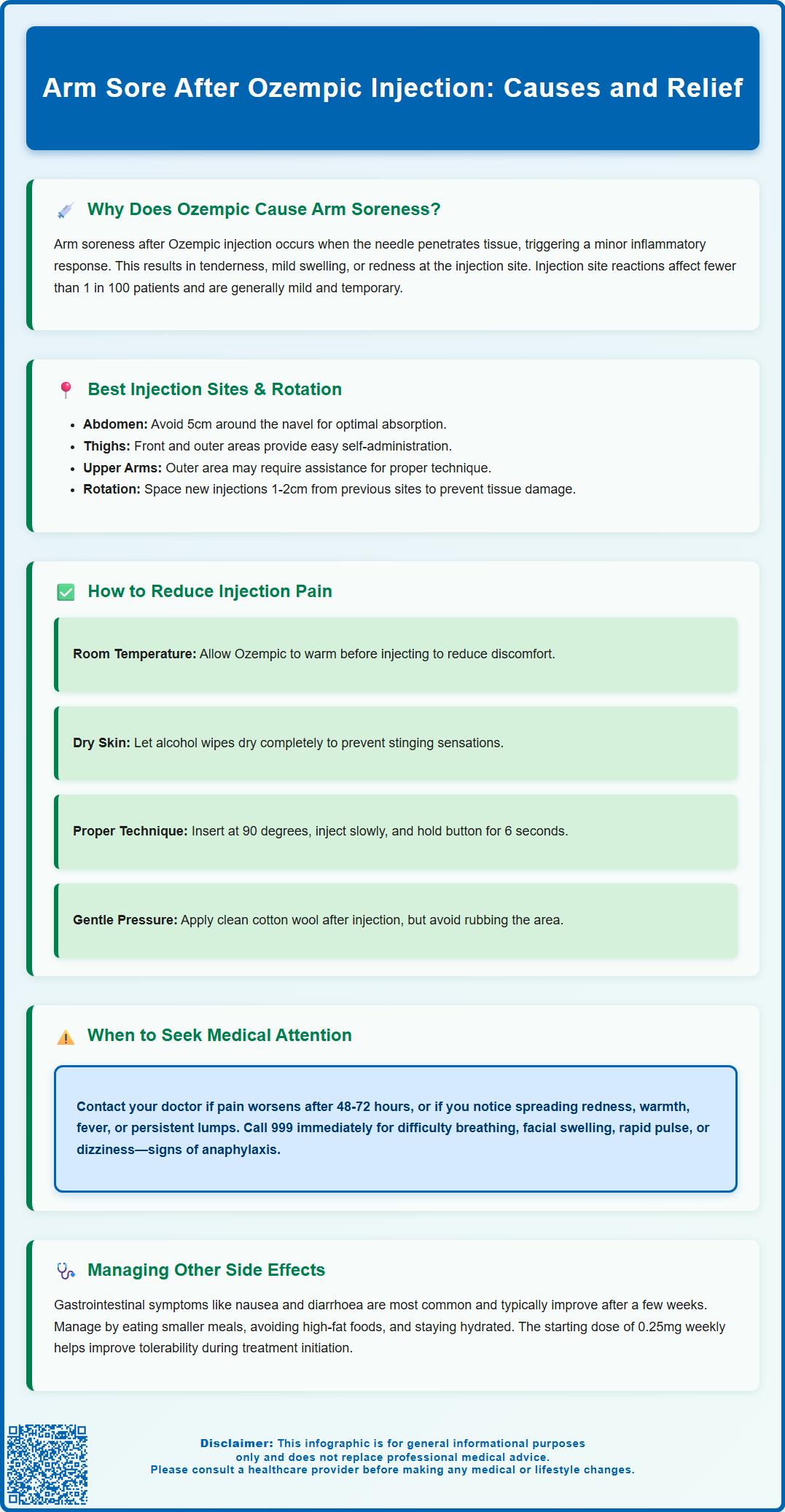
- Injection site reactions are classified as uncommon, affecting between 1 in 100 and 1 in 1,000 patients
- Pain can be reduced by using room-temperature medication, proper injection technique, systematic site rotation, and allowing alcohol to dry before injection
- Medical attention is required for severe worsening pain, significant swelling with warmth or redness, fever, or signs of allergic reaction
- Approved injection sites include the abdomen, front and outer thighs, and outer upper arms with systematic rotation between sites
- Regular monitoring and communication with healthcare professionals ensure safe therapy and appropriate management of adverse effects
Table of Contents
- Why Does Ozempic Cause Arm Soreness After Injection?
- How to Reduce Injection Site Pain When Using Ozempic
- When Arm Pain After Ozempic Requires Medical Attention
- Best Injection Sites and Techniques for Ozempic
- Managing Side Effects and Discomfort with Ozempic Treatment
- Scientific References
- Frequently Asked Questions
Why Does Ozempic Cause Arm Soreness After Injection?
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist administered via subcutaneous injection for the management of type 2 diabetes mellitus. Arm soreness following Ozempic injection is a recognised local reaction that occurs in some patients, though it is generally mild and self-limiting. Understanding the underlying mechanisms can help patients manage expectations and distinguish normal reactions from those requiring medical review.
The soreness experienced after injecting Ozempic into the arm typically results from the mechanical trauma of needle insertion and the subsequent inflammatory response triggered by the introduction of the medication into subcutaneous tissue. When the needle penetrates the skin and underlying tissue, it causes minor tissue disruption and activates a local inflammatory response. This localised inflammation may manifest as tenderness, mild swelling, or redness at the injection site.
According to the Ozempic Summary of Product Characteristics (SmPC), injection site reactions are classified as 'uncommon', meaning they affect between 1 in 100 and 1 in 1,000 patients (trial rates were typically below 1%). The subcutaneous space in the arm, abdomen, or thigh can all be used for Ozempic administration, with individual patient comfort varying between sites. Injection technique, including needle depth and injection speed, can influence the degree of soreness experienced. It is important to note that whilst arm soreness is an expected local reaction, there is no official link between this discomfort and the systemic therapeutic effects of semaglutide, which acts to regulate glucose metabolism and appetite.
How to Reduce Injection Site Pain When Using Ozempic
Minimising injection site discomfort is an important aspect of treatment adherence and patient satisfaction with Ozempic therapy. Several evidence-based strategies can significantly reduce arm soreness and improve the overall injection experience. Implementing these techniques consistently can help patients maintain their treatment regimen with greater comfort and confidence.
Firstly, injections may be more comfortable when Ozempic is at room temperature. According to the Ozempic Patient Information Leaflet (PIL), after first use, the pen may be stored at room temperature (below 30°C) or in a refrigerator for up to 6 weeks. The medication should not be artificially warmed or exposed to direct heat. Regarding skin preparation, if the injection site is visibly dirty, cleaning with soap and water or an alcohol wipe is recommended. If using an alcohol wipe, allow the area to dry completely before injection to prevent stinging sensations.
Injection technique plays a vital role in minimising discomfort. The Ozempic Instructions for Use advise patients to pinch a fold of skin if they are slim or using a longer needle, while those with more subcutaneous tissue may not need to pinch. The needle should be inserted at an appropriate angle (typically 90 degrees) in a smooth, confident motion. The medication should be injected slowly and steadily. After injection, patients should keep the pen button fully pressed and count slowly to 6 before withdrawing the needle to ensure complete dose delivery and reduce medication leakage.
Rotating injection sites systematically is essential to prevent localised tissue damage and cumulative soreness. Whilst the arm is a suitable injection site, alternating between different areas of the abdomen, thigh, and upper arm allows previously used sites adequate recovery time. Each new injection should be given at least 1-2 cm away from the previous one. Patients should avoid injecting into areas with visible bruising, scarring, or skin abnormalities. Applying gentle pressure with a clean cotton wool ball immediately after injection can help reduce bleeding and bruising, though vigorous rubbing should be avoided as this may increase irritation and affect medication absorption.
When Arm Pain After Ozempic Requires Medical Attention
Whilst mild arm soreness following Ozempic injection is expected and typically resolves within a few days, certain symptoms warrant prompt medical evaluation. Recognising the distinction between normal post-injection reactions and potentially serious complications is essential for patient safety. Patients should be educated about warning signs that require contact with their GP or diabetes specialist nurse.
Severe or worsening pain that intensifies rather than improves over 48 to 72 hours may indicate an injection site complication requiring assessment. Similarly, significant swelling extending beyond the immediate injection area, particularly if accompanied by warmth, increasing redness, or red streaking radiating from the site, could suggest cellulitis or another soft tissue infection. Although rare with proper injection technique and hygiene, bacterial infections can occur and require antibiotic therapy. Patients should seek same-day medical advice if they develop fever, chills, or systemic symptoms alongside injection site changes.
Allergic reactions, though uncommon, represent another important consideration. Localised urticaria (hives), intense itching, or the development of a raised, indurated area at the injection site may indicate hypersensitivity to semaglutide or an excipient in the formulation. Whilst mild local reactions may be managed conservatively, patients experiencing difficulty breathing, facial swelling, rapid pulse, or dizziness should call 999 immediately, as these symptoms may indicate anaphylaxis.
Persistent nodules or lumps at injection sites that do not resolve within two weeks should be evaluated by a healthcare professional. Additionally, patients experiencing recurrent severe injection site reactions across multiple sites or those finding the discomfort significantly impacts treatment adherence should discuss alternative GLP-1 receptor agonist formulations or delivery methods with their prescribing clinician. For urgent advice when GP services are unavailable, patients should contact NHS 111. The MHRA Yellow Card scheme (yellowcard.mhra.gov.uk) allows patients and healthcare professionals to report suspected adverse drug reactions, contributing to ongoing medication safety monitoring.
Best Injection Sites and Techniques for Ozempic
Selecting appropriate injection sites and employing correct technique are fundamental to optimising Ozempic therapy whilst minimising discomfort and complications. The medication is designed for subcutaneous administration, meaning it should be injected into the fatty tissue layer between skin and muscle. Understanding anatomical considerations and proper injection methodology enhances treatment efficacy and patient comfort.
According to the Ozempic SmPC, the medication can be administered into three primary body areas: the abdomen (excluding a 5cm radius around the navel), the front and outer aspects of the thighs, and the outer upper arms. All three sites are considered equally appropriate for administration. When using the arm, patients should target the outer upper arm area where there is adequate subcutaneous tissue. As noted in the Instructions for Use, self-injection into the arm can be challenging, and this site may require assistance from another person to ensure proper technique.
The thigh offers an accessible alternative, particularly the middle and outer portions of the upper leg. This site allows for easy self-administration and typically has sufficient subcutaneous tissue in most patients. Regardless of the chosen site, systematic rotation is essential. Patients should rotate between different injection sites with each dose, using a different point at least 1-2 cm from the previous injection within each region. Keeping a simple injection diary or using a rotation chart can help track sites and prevent overuse of particular areas.
Proper injection technique begins with hand hygiene and site preparation. After selecting a site, patients should inspect the area for any abnormalities and cleanse if necessary. The skin should be pinched gently between thumb and forefinger if needed based on body habitus and needle length. The needle should be inserted at the appropriate angle (typically 90 degrees). After depressing the dose button fully, maintaining pressure for six seconds ensures complete dose delivery. The needle should then be withdrawn smoothly, and only the needle (not the entire pen) should be disposed of safely in a sharps container. The Ozempic pen is designed for multiple doses and should be stored according to the PIL instructions until empty or expired. Patients uncertain about their technique should request a review with their diabetes specialist nurse or practice nurse, who can observe their method and provide personalised guidance.
Managing Side Effects and Discomfort with Ozempic Treatment
Comprehensive management of Ozempic-related side effects extends beyond addressing injection site reactions and encompasses the broader spectrum of potential adverse effects associated with GLP-1 receptor agonist therapy. A holistic approach to side effect management supports treatment adherence and optimises clinical outcomes for patients with type 2 diabetes.
Gastrointestinal symptoms represent the most frequently reported adverse effects of Ozempic, affecting a substantial proportion of patients, particularly during treatment initiation and dose escalation. Nausea, vomiting, diarrhoea, and constipation occur due to semaglutide's effects on gastric emptying and gut motility. These symptoms are typically most pronounced during the first few weeks of therapy and often diminish as the body adapts. Patients can minimise gastrointestinal discomfort by eating smaller, more frequent meals, avoiding high-fat and spicy foods, and ensuring adequate hydration. The graduated dosing schedule in the Ozempic SmPC—starting at 0.25mg weekly for four weeks before increasing to 0.5mg—is specifically designed to improve tolerability. Patients experiencing persistent or severe gastrointestinal symptoms should consult their prescriber, as dose adjustment or temporary treatment interruption may be necessary. Severe vomiting or diarrhoea can lead to dehydration and acute kidney injury, requiring prompt medical attention.
Beyond injection site reactions and gastrointestinal effects, patients should be aware of less common but clinically significant adverse effects. Hypoglycaemia risk increases when Ozempic is used in combination with insulin or sulfonylureas, necessitating potential dose adjustments of these concurrent medications. Patients should be educated about hypoglycaemia recognition and management. The SmPC notes that rapid improvement in glucose control has been associated with temporary worsening of diabetic retinopathy, particularly in patients with pre-existing retinopathy. Additionally, there is an increased risk of gallbladder disease, including cholelithiasis and cholecystitis. There have been post-marketing reports of acute pancreatitis in patients taking GLP-1 receptor agonists; persistent severe abdominal pain radiating to the back requires urgent medical assessment and treatment discontinuation pending investigation.
Regular monitoring and open communication with healthcare professionals are essential components of safe Ozempic therapy. Patients should attend scheduled diabetes reviews, during which HbA1c, renal function, and body weight are typically assessed. Any concerns about side effects, injection technique difficulties, or treatment efficacy should be discussed promptly. The multidisciplinary diabetes team, including GPs, specialist nurses, and pharmacists, can provide tailored advice and support. Patients should never discontinue Ozempic abruptly without medical guidance, as this may result in deterioration of glycaemic control. For those finding subcutaneous injections particularly challenging, discussion of alternative diabetes management strategies, including other GLP-1 receptor agonist formulations or different therapeutic classes, may be appropriate. Patient education resources from Diabetes UK and the NHS provide valuable supplementary information to support informed decision-making and successful long-term diabetes management.
Scientific References
Frequently Asked Questions
How long does arm soreness last after Ozempic injection?
Mild arm soreness after Ozempic injection typically resolves within a few days. If pain worsens or persists beyond 48 to 72 hours, contact your GP or diabetes specialist nurse for assessment.
Can I inject Ozempic in the same arm each week?
You should rotate injection sites systematically, alternating between the abdomen, thigh, and upper arm. Each new injection should be at least 1-2 cm away from the previous site to prevent tissue damage and cumulative soreness.
Should I stop using Ozempic if my arm is sore after injection?
Mild arm soreness is a normal reaction and does not require stopping treatment. However, if you experience severe pain, significant swelling, warmth, redness, or fever, seek medical advice promptly before your next dose.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript