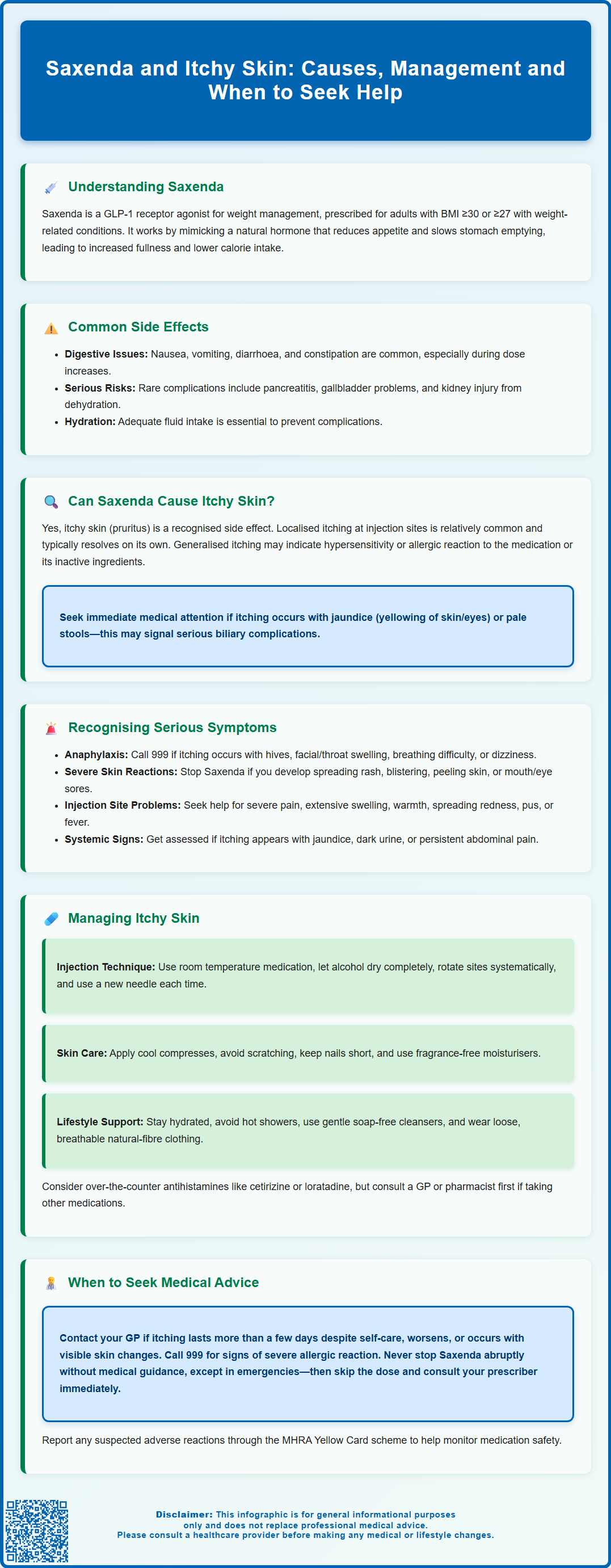
Saxenda (liraglutide 3 mg) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for weight management in adults and adolescents with obesity. Whilst gastrointestinal side effects such as nausea and diarrhoea are well recognised, some patients report experiencing itchy skin during treatment. Pruritus, both at injection sites and more generalised, is documented in the official product information. Understanding whether itching is a benign reaction, a sign of hypersensitivity, or unrelated to Saxenda is essential for safe medication use. This article explores the relationship between Saxenda and itchy skin, how to manage symptoms, and when to seek medical advice.
Summary: Saxenda can cause itchy skin, with both localised injection site pruritus and generalised itching documented as recognised adverse reactions in UK product information.
- Saxenda (liraglutide 3 mg) is a GLP-1 receptor agonist licensed for weight management in adults and adolescents with obesity in the UK.
- Pruritus, rash, and urticaria are documented side effects; itching may occur at injection sites or more widely across the body.
- Localised itching often relates to injection technique or site irritation, whilst generalised itching may indicate hypersensitivity reactions.
- Management includes proper injection technique, site rotation, emollients, cool compresses, and oral antihistamines for symptomatic relief.
- Urgent medical attention is required for signs of anaphylaxis (facial swelling, breathing difficulty, widespread hives) or severe skin reactions.
- Itching with jaundice, dark urine, or severe abdominal pain warrants prompt assessment for biliary or pancreatic complications.
Table of Contents
Understanding Saxenda and Its Common Side Effects
Saxenda (liraglutide 3 mg) is a prescription medicine licensed in the UK for weight management in adults with a BMI ≥30 kg/m² or ≥27-<30 kg/m² with weight-related health conditions. It's also licensed for adolescents aged 12 years and above with obesity. Saxenda is used as an adjunct to a reduced-calorie diet and increased physical activity.
It belongs to a class of medications called glucagon-like peptide-1 (GLP-1) receptor agonists, which work by mimicking a naturally occurring hormone that regulates appetite and food intake.
The mechanism of action involves binding to GLP-1 receptors in the brain, particularly in areas that control appetite, and slowing gastric emptying. This leads to increased feelings of fullness, reduced hunger, and consequently lower calorie intake. Saxenda is administered as a once-daily subcutaneous injection, typically in the abdomen, thigh, or upper arm. The dose starts at 0.6 mg daily and increases by 0.6 mg weekly to a maximum of 3 mg daily as tolerated. Treatment should be discontinued after 12 weeks at the 3 mg/day dose if at least 5% of initial body weight has not been lost.
Common side effects associated with Saxenda predominantly affect the gastrointestinal system. These include nausea, vomiting, diarrhoea, constipation, and abdominal discomfort. These symptoms are usually most pronounced during the initial titration period and often improve as the body adjusts to the medication. Other frequently reported effects include headache, dizziness, fatigue, and injection site reactions such as redness, swelling, bruising, or itching at the injection site.
According to the Medicines and Healthcare products Regulatory Agency (MHRA) and product literature, most adverse effects are mild to moderate in severity. However, patients should be aware of potential serious complications, including pancreatitis, gallbladder problems, and increased heart rate. Dehydration from gastrointestinal side effects may increase the risk of acute kidney injury, so maintaining adequate hydration is important. Understanding the full spectrum of possible side effects helps patients distinguish between expected reactions and those requiring medical attention, including skin-related symptoms that may occasionally occur.
Can Saxenda Cause Itchy Skin?
Itchy skin, medically termed pruritus, is a recognised adverse reaction to Saxenda according to the official product information. Both generalised pruritus and injection site itching are listed in the Saxenda Summary of Product Characteristics (SmPC). Rash and urticaria (hives) are also documented side effects.
When itching occurs in patients using Saxenda, it may manifest in several ways. Some individuals experience localised itching at injection sites, which can be attributed to the physical trauma of injection, the medication itself causing local irritation, or sensitivity to the solution components. This type of reaction is relatively common with subcutaneous injections and usually resolves without intervention. Rotating injection sites as recommended can help minimise this localised response.
Generalised itching affecting larger areas of the body may occur as part of a hypersensitivity reaction or allergic response to the medication. In rare cases, sensitivity to inactive ingredients in the formulation might contribute, though this is less common.
It is also worth considering that itching may sometimes be coincidental rather than causally related to Saxenda use. Pruritus has numerous potential causes, including dry skin (particularly common in older adults), dermatological conditions such as eczema or psoriasis, systemic diseases affecting the liver or kidneys, and other medications the patient may be taking concurrently.
Importantly, new-onset generalised itching with jaundice (yellowing of the skin/eyes) or pale stools warrants prompt medical assessment, as it could indicate biliary complications, which are a recognised risk with GLP-1 medications. A thorough assessment is necessary to determine whether Saxenda is genuinely implicated or whether alternative explanations should be explored.
Recognising Allergic Reactions and Serious Skin Symptoms
Whilst mild itching may be benign, it is crucial to recognise when skin symptoms indicate a more serious allergic or hypersensitivity reaction. Anaphylaxis, though rare with Saxenda, is a medical emergency characterised by rapid onset of symptoms affecting multiple body systems. Warning signs include widespread itching accompanied by urticaria (hives), facial or throat swelling (angioedema), difficulty breathing, wheezing, rapid pulse, dizziness, or a sudden drop in blood pressure.
Patients should be particularly vigilant for progressive or worsening symptoms. Extremely rarely, medications can cause serious skin reactions. If itching is accompanied by a spreading rash, blistering, peeling skin, or mucosal involvement (affecting the mouth, eyes, or genital area), this requires immediate medical intervention and discontinuation of the suspected medication. While such severe cutaneous reactions are not specifically linked to liraglutide in current UK labelling, any such symptoms should be treated as a medical emergency.
Injection site reactions warrant attention when they extend beyond mild, transient irritation. Severe pain, extensive swelling, warmth, spreading redness, or signs of infection (such as pus or fever) should prompt medical review. Persistent nodules or lumps at injection sites should also be assessed by a healthcare professional.
Other concerning features include itching associated with jaundice (yellowing of skin or eyes), dark urine, pale stools, or persistent abdominal pain, which could indicate liver or gallbladder complications. If severe, persistent upper abdominal pain (possibly with vomiting) suggests pancreatitis, patients should stop taking Saxenda and seek urgent medical assessment. Similarly, itching accompanied by unexplained weight loss, night sweats, or enlarged lymph nodes requires investigation to exclude underlying systemic conditions. The MHRA Yellow Card scheme encourages reporting of suspected adverse drug reactions, contributing to ongoing medication safety surveillance.
Managing Itchy Skin While Taking Saxenda
For patients experiencing mild, localised itching at injection sites, several practical strategies can provide relief. Ensuring proper injection technique is fundamental—using a new needle for each injection, allowing the skin to dry completely after cleaning with alcohol wipes, and injecting at room temperature (removing Saxenda from the refrigerator 15–30 minutes beforehand) can reduce irritation. Systematic rotation of injection sites across the abdomen, thighs, and upper arms prevents repeated trauma to the same area and allows tissue recovery.
Applying a cool compress to itchy areas can provide symptomatic relief without interfering with medication absorption. Patients should avoid scratching, which can damage skin integrity and increase infection risk. Keeping fingernails short and wearing cotton gloves at night may help prevent unconscious scratching during sleep. Over-the-counter emollients and moisturisers can be beneficial, particularly for those with underlying dry skin. Fragrance-free, hypoallergenic products are preferable to minimise additional irritation.
For more troublesome itching, oral antihistamines such as cetirizine or loratadine may be considered. These non-sedating antihistamines are available over the counter and can help manage histamine-mediated itching. Patients should check labels for potential drowsiness warnings and be aware that some antihistamines may cause drowsiness affecting driving ability. Those taking multiple medicines or with underlying health conditions should consult their GP or pharmacist before starting any new medication to ensure there are no contraindications or interactions with their existing treatment regimen.
Lifestyle modifications can also support skin health during Saxenda treatment. Maintaining adequate hydration, avoiding hot showers or baths (which can dry the skin), using gentle, soap-free cleansers, and wearing loose, breathable clothing made from natural fibres can all help reduce skin irritation. If itching persists despite these measures, or if there is uncertainty about its cause, patients should seek professional medical advice rather than discontinuing prescribed medication independently. If symptoms worsen outside of GP hours, NHS 111 can provide urgent advice.
When to Seek Medical Advice
Patients should contact their GP or prescribing clinician if itching persists for more than a few days despite self-care measures, or if it progressively worsens in intensity or distribution. Medical review is particularly important when itching is accompanied by visible skin changes such as rash, blistering, discolouration, or texture changes, as these may indicate conditions requiring specific treatment or medication adjustment.
Urgent medical attention is required if symptoms suggest an allergic reaction. Patients experiencing widespread hives, facial swelling, tongue or throat swelling, difficulty breathing, chest tightness, or feeling faint should seek immediate help by calling 999 or attending the nearest emergency department. These symptoms may indicate anaphylaxis, which requires prompt administration of adrenaline and supportive care. Patients with known severe allergies may already carry an adrenaline auto-injector (EpiPen), which should be used according to previous medical advice whilst awaiting emergency services.
Consultation is also warranted when itching is associated with systemic symptoms such as fever, malaise, joint pain, or signs suggesting organ involvement (jaundice, dark urine, persistent abdominal pain). These features may indicate complications requiring investigation through blood tests, imaging, or specialist referral. If severe, persistent upper abdominal pain occurs (possibly with vomiting), this could indicate pancreatitis – patients should not take another dose of Saxenda and should seek urgent medical assessment.
For urgent advice when GP services are unavailable, patients should contact NHS 111, which can provide guidance and arrange appropriate care if needed.
Patients should generally not abruptly stop Saxenda without medical guidance. However, if severe allergic reactions, serious skin reactions, or symptoms of pancreatitis occur, patients should not take another dose until they have received medical advice. Any decision to discontinue treatment should be made in consultation with their prescriber, who can assess the risk-benefit balance and consider alternative weight management strategies if necessary.
Suspected side effects can be reported through the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk), which helps monitor the safety of medicines and identify new side effects.
Frequently Asked Questions
Is itchy skin a common side effect of Saxenda?
Itchy skin (pruritus) is a recognised adverse reaction to Saxenda, documented in UK product information. It may occur at injection sites or more widely, though gastrointestinal side effects remain more common.
What should I do if I develop itchy skin whilst taking Saxenda?
For mild localised itching, rotate injection sites, apply cool compresses, use emollients, and consider oral antihistamines. Seek medical advice if itching persists, worsens, or is accompanied by rash or systemic symptoms.
When does itchy skin from Saxenda require urgent medical attention?
Seek immediate help (call 999) if itching occurs with facial or throat swelling, difficulty breathing, widespread hives, or feeling faint, as these may indicate anaphylaxis requiring emergency treatment.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript