Allergic reactions to Ozempic, whilst rare, can range from mild injection site responses to serious systemic hypersensitivity requiring emergency treatment. Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes management, administered as a weekly subcutaneous injection. Understanding how to recognise and respond to potential allergic reactions is essential for patient safety. This article examines the types of allergic reactions associated with Ozempic, identifies warning signs requiring urgent medical attention, and outlines appropriate management steps in line with UK guidance from the MHRA, NICE, and NHS clinical protocols.
Summary: Allergic reactions to Ozempic range from mild local injection site reactions to rare but serious systemic hypersensitivity including anaphylaxis, requiring immediate discontinuation and emergency treatment in severe cases.
- Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes, administered as a weekly subcutaneous injection.
- Mild reactions include injection site redness and itching; serious reactions include widespread hives, angioedema, breathing difficulties, and anaphylaxis.
- Anaphylaxis is a medical emergency requiring immediate 999 call, adrenaline administration, and permanent discontinuation of Ozempic.
- Hypersensitivity to semaglutide or excipients is a contraindication; patients with drug allergy history should inform prescribers before starting treatment.
- Alternative diabetes treatments include other GLP-1 agonists (if no cross-reactivity), SGLT2 inhibitors, DPP-4 inhibitors, or insulin therapy per NICE NG28 guidance.
- All suspected allergic reactions should be reported to the MHRA via the Yellow Card scheme and documented in medical records.
Table of Contents
What Is Ozempic and How Does It Work?
Ozempic is the brand name for semaglutide, a prescription medicine licensed in the UK for the treatment of type 2 diabetes mellitus in adults. It is not licensed for weight management or for use in type 1 diabetes or diabetic ketoacidosis. Ozempic belongs to a class of medications known as glucagon-like peptide-1 (GLP-1) receptor agonists, which work by mimicking the action of a naturally occurring hormone that regulates blood glucose levels. The Medicines and Healthcare products Regulatory Agency (MHRA) approved Ozempic for use in the UK, and it is administered as a once-weekly subcutaneous injection.
The mechanism of action of semaglutide involves binding to GLP-1 receptors found throughout the body, particularly in the pancreas, gastrointestinal tract, and brain. When blood glucose levels rise after eating, Ozempic stimulates the pancreas to release insulin in a glucose-dependent manner, meaning it only works when blood sugar is elevated. Simultaneously, it suppresses the release of glucagon, a hormone that raises blood glucose levels. This dual action helps to maintain more stable blood sugar control throughout the day.
Beyond its effects on glucose regulation, Ozempic slows gastric emptying, which means food moves more slowly from the stomach into the small intestine. This effect is most pronounced after initiation and may diminish with continued use. The delayed gastric emptying contributes to increased feelings of fullness and can lead to reduced appetite. The medication has also been associated with modest weight loss in many patients, which can be beneficial for individuals with type 2 diabetes who are overweight. NICE guidance (NG28) recognises GLP-1 receptor agonists as an important treatment option for type 2 diabetes, particularly when other medications have not achieved adequate glycaemic control or when weight management is a clinical priority.
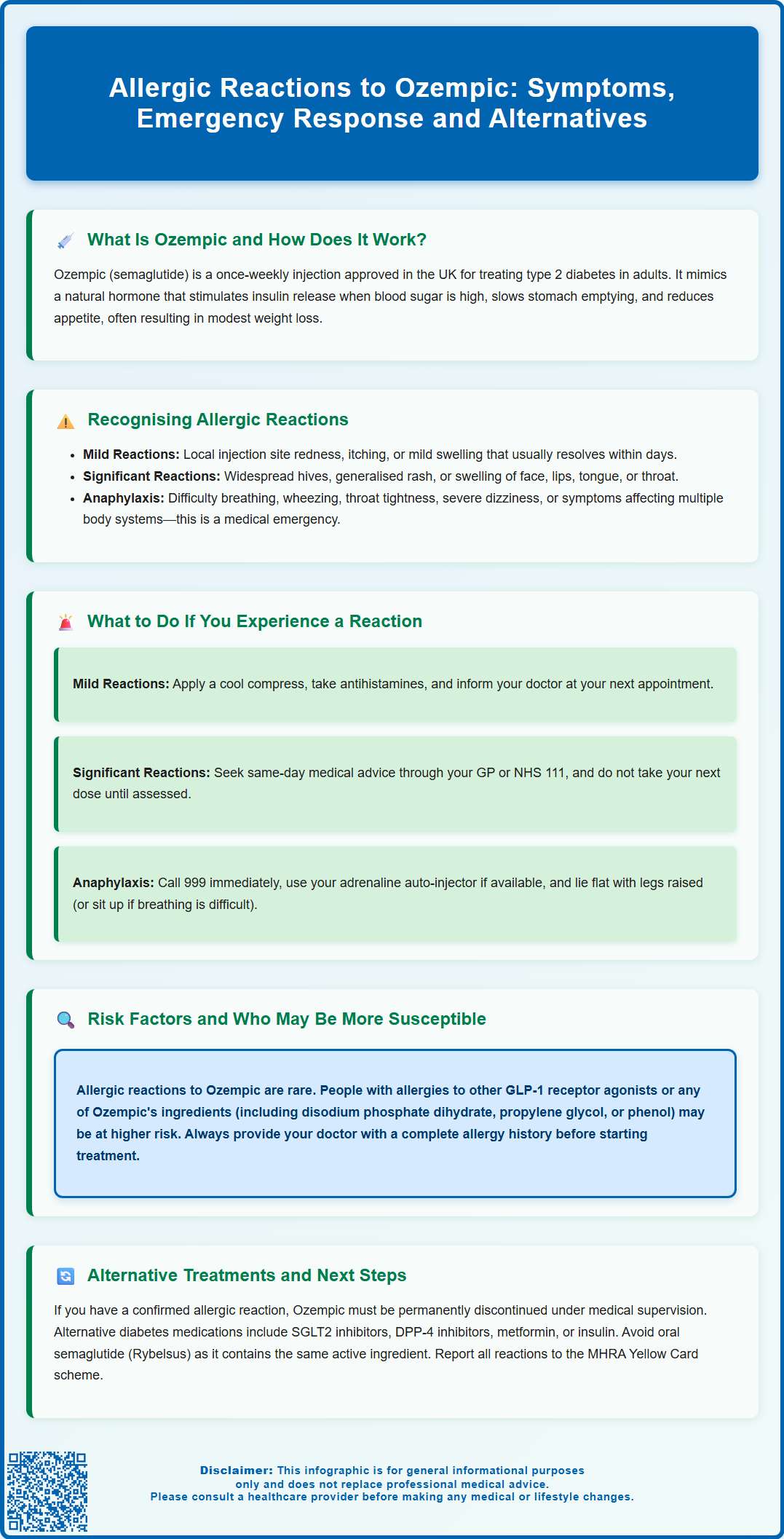
Recognising Allergic Reactions to Ozempic
Allergic reactions to Ozempic can range from mild local reactions at the injection site to rare but serious systemic hypersensitivity responses. It is important to distinguish between common side effects and genuine allergic reactions, as this determines the appropriate course of action. Local injection site reactions, such as redness, itching, or mild swelling at the site where the needle entered the skin, are relatively common and usually resolve within a few days. These reactions do not necessarily indicate a true allergy and often improve with continued use.
More concerning allergic reactions include widespread skin manifestations such as urticaria (hives), which appear as raised, itchy welts that can occur anywhere on the body. Some patients may develop a generalised rash, facial swelling, or swelling of the lips, tongue, or throat (angioedema). These symptoms suggest a more significant hypersensitivity response and require prompt medical attention. Respiratory symptoms, including difficulty breathing, wheezing, or a sensation of throat tightness, are particularly serious and may indicate the onset of anaphylaxis, a life-threatening allergic emergency.
Anaphylaxis and angioedema related to Ozempic are rare but represent a medical emergency requiring immediate treatment. According to the Summary of Product Characteristics (SmPC), serious hypersensitivity reactions including anaphylaxis and angioedema have been reported with semaglutide in post-marketing surveillance. Warning signs include a rapid onset of symptoms affecting multiple body systems: skin reactions combined with breathing difficulties, a sudden drop in blood pressure causing dizziness or loss of consciousness, rapid heartbeat, and gastrointestinal symptoms such as severe abdominal cramping or vomiting. If you experience any combination of these symptoms after administering Ozempic, you should call 999 immediately and the medication should be permanently discontinued.
What to Do If You Experience an Allergic Reaction
If you suspect you are experiencing an allergic reaction to Ozempic, your response should be proportionate to the severity of your symptoms. For mild local reactions confined to the injection site—such as slight redness, itching, or minor swelling—you can typically manage these at home by applying a cool compress to the affected area and taking an over-the-counter antihistamine if the itching is bothersome. However, you should still inform your GP or diabetes specialist nurse at your next appointment, as they may wish to monitor the reaction or adjust your injection technique.
For more significant reactions, such as widespread hives, facial swelling, or any swelling affecting the mouth or throat, you should seek same-day medical advice. Contact your GP surgery immediately, call NHS 111 for guidance, or attend an Urgent Treatment Centre. Do not administer your next dose of Ozempic until you have been assessed by a healthcare professional. If the reaction occurred shortly after injection, note the time and any other factors that might be relevant, such as whether you used a different injection site or if you were taking any new medications.
In the event of severe symptoms suggesting anaphylaxis—including difficulty breathing, swelling of the tongue or throat causing breathing problems, sudden severe dizziness, or collapse—call 999 immediately and state that you believe you are having an allergic reaction. If you carry an adrenaline auto-injector (such as an EpiPen, Jext, or Emerade) for known allergies, use it without delay according to the instructions you have been given. Adrenaline is the first-line life-saving treatment for anaphylaxis. Lie flat with your legs raised unless you are having difficulty breathing, in which case sit up in a position that makes breathing easier. Do not attempt to drive yourself to hospital. Emergency treatment for anaphylaxis includes intramuscular adrenaline, oxygen therapy, intravenous fluids, and antihistamines (as an adjunctive treatment only), followed by a period of observation in hospital (typically at least 6 hours, and potentially longer if severe or if there are risk factors for a biphasic reaction). Both you and your healthcare professional should report the reaction to the MHRA via the Yellow Card scheme.
Risk Factors and Who May Be More Susceptible
Allergic reactions to Ozempic can theoretically occur in anyone, though they are rare. The Summary of Product Characteristics (SmPC) states that hypersensitivity to semaglutide or any of the excipients is a contraindication to using Ozempic. Individuals with a history of allergies to other medications, particularly other GLP-1 receptor agonists such as liraglutide (Victoza) or dulaglutide (Trulicity), may be at increased risk and should discuss this history with their prescribing clinician before starting Ozempic.
Patients with multiple drug allergies should inform their healthcare provider, as this may influence the decision to prescribe or the monitoring plan. It is worth noting that the active ingredient semaglutide is a synthetic peptide, and the formulation also contains excipients including disodium phosphate dihydrate, propylene glycol, and phenol, as listed in the current SmPC. Any of these ingredients could potentially trigger a reaction in susceptible individuals.
Before prescribing Ozempic, your doctor should take a comprehensive allergy history and discuss any previous adverse reactions to injectable medications. If you have previously experienced injection site reactions to other subcutaneous medications, this should be mentioned. The MHRA recommends that healthcare professionals remain vigilant for hypersensitivity reactions when initiating any new medication, and patients should be counselled on recognising the signs of allergic reactions before their first dose. There is no routine allergy testing available for Ozempic prior to use, so clinical history remains the primary tool for risk assessment. If you have experienced a confirmed allergic reaction to injectable semaglutide, oral semaglutide (Rybelsus) should also be avoided as it contains the same active ingredient.
Alternative Treatments and Next Steps
If you have experienced a confirmed allergic reaction to Ozempic, your healthcare team will need to review your diabetes management plan and consider alternative treatment options. The decision to discontinue Ozempic should always be made in consultation with your GP or diabetes specialist, as abruptly stopping the medication without a replacement strategy could lead to deterioration in blood glucose control. Your doctor will assess the severity of the reaction and determine whether it represents a true allergy requiring permanent avoidance of semaglutide. According to the SmPC, Ozempic should be permanently discontinued if a serious hypersensitivity reaction is suspected.
Alternative medications for type 2 diabetes are numerous and include other classes of glucose-lowering agents with different mechanisms of action. If the allergic reaction was specifically to semaglutide, other GLP-1 receptor agonists may also need to be avoided, though cross-reactivity is not guaranteed and would depend on the nature of the allergic response. Oral semaglutide (Rybelsus) should not be used after a confirmed semaglutide allergy. Other options include SGLT2 inhibitors such as dapagliflozin or empagliflozin, DPP-4 inhibitors like sitagliptin, or traditional agents such as metformin (if not already prescribed), sulfonylureas, or insulin therapy. NICE guidance (NG28) provides a structured approach to type 2 diabetes management, with treatment intensification based on individual patient factors including HbA1c levels, cardiovascular risk, and tolerability.
Your diabetes care team will work with you to identify the most appropriate alternative based on your clinical circumstances, other medical conditions, and treatment goals. This may involve a period of more frequent blood glucose monitoring whilst transitioning to a new medication. If you experienced anaphylaxis or a severe allergic reaction, you should be referred to an allergy specialist for further assessment in line with NICE guidance (NG196 and NG213) and may be prescribed an adrenaline auto-injector to carry for future protection. You should also receive a written emergency action plan and training on how to use your adrenaline auto-injector. It is essential to ensure that your allergic reaction to Ozempic is clearly documented in your medical records and that you inform all healthcare providers of this allergy in future consultations. Both you and your healthcare professional should report the reaction to the MHRA via the Yellow Card scheme, which monitors medication safety across the UK and helps identify previously unrecognised adverse effects.
Scientific References
- Ozempic 0.5 mg solution for injection in pre-filled pen - Summary of Product Characteristics (SmPC).
- Type 2 diabetes in adults: management. NICE guideline [NG28].
- Ozempic (semaglutide) - European Public Assessment Report.
- GLP-1 receptor agonists: reminder of the potential side effects and to be aware of the potential for misuse.
- Treatment for type 2 diabetes.
Frequently Asked Questions
What are the signs of a serious allergic reaction to Ozempic?
Serious allergic reactions include widespread hives, facial or throat swelling (angioedema), difficulty breathing, wheezing, rapid heartbeat, severe dizziness, or collapse. These symptoms require immediate emergency care by calling 999, as they may indicate anaphylaxis.
Should I stop taking Ozempic if I have a mild injection site reaction?
Mild injection site reactions such as redness or itching are common and usually resolve within days. You should inform your GP or diabetes nurse, but do not stop Ozempic without medical advice, as these reactions often improve with continued use and do not necessarily indicate a true allergy.
What diabetes medications can I use if I'm allergic to Ozempic?
Alternative treatments include SGLT2 inhibitors (dapagliflozin, empagliflozin), DPP-4 inhibitors (sitagliptin), metformin, sulfonylureas, or insulin therapy. Your diabetes care team will select the most appropriate option based on your clinical circumstances, following NICE guidance for type 2 diabetes management.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript