Many people wonder what improves overall metabolism and activates sluggish skin, seeking ways to enhance both energy levels and skin appearance. Metabolism encompasses the biochemical processes that convert nutrients into energy and support cellular function throughout the body, including the skin. The skin, as the body's largest organ, is highly metabolically active and requires substantial energy for regeneration, barrier function, and structural integrity. Whilst "sluggish skin" is not a recognised medical diagnosis, it describes skin that appears dull, lacks radiance, or shows delayed healing. This article explores evidence-based approaches to support metabolic health and skin vitality, including medical treatments for underlying conditions, skincare interventions, and lifestyle modifications grounded in UK clinical guidance.
Summary: Evidence-based approaches that improve overall metabolism and address sluggish skin include treating underlying medical conditions (such as hypothyroidism or iron deficiency), using topical retinoids and chemical exfoliants, and implementing lifestyle modifications including regular physical activity, balanced nutrition, and adequate sleep.
- Thyroid disorders, iron deficiency anaemia, and insulin resistance are common medical causes requiring specific pharmacological treatment under medical supervision.
- Topical retinoids, alpha-hydroxy acids, niacinamide, and vitamin C have evidence supporting their use for improving skin texture and appearance, though realistic expectations are essential.
- Regular physical activity (150 minutes moderate-intensity weekly) and balanced nutrition following the NHS Eatwell Guide support both metabolic function and skin health.
- There are no licensed medications specifically indicated to boost metabolism in healthy individuals; products marketed with such claims lack robust clinical evidence.
- Persistent fatigue with unexplained weight changes, or skin changes including non-healing lesions or new pigmented areas, warrant GP evaluation to exclude underlying pathology.
Table of Contents
- Understanding Metabolism and Its Impact on Skin Health
- Medical Causes of Sluggish Skin and Slow Metabolism
- Evidence-Based Treatments to Support Metabolic Function
- Skincare Approaches for Dull and Tired-Looking Skin
- Lifestyle Factors That Influence Metabolism and Skin Vitality
- When to Seek Medical Advice for Skin and Metabolic Concerns
- Frequently Asked Questions
Understanding Metabolism and Its Impact on Skin Health
Metabolism refers to the complex biochemical processes that convert nutrients into energy and support cellular function throughout the body. This encompasses both catabolism (the breakdown of molecules to produce energy) and anabolism (the synthesis of compounds needed for cellular maintenance and growth). The skin, as the body's largest organ, is highly metabolically active and requires substantial energy and nutrients to maintain its barrier function, regenerative capacity, and structural integrity.
The relationship between systemic metabolism and skin health is multifaceted. Cellular metabolism within the skin itself drives keratinocyte turnover, collagen synthesis, and the production of natural moisturising factors. When metabolic processes function optimally, skin cells regenerate efficiently, typically completing a full turnover cycle every 4-8 weeks, with this process generally taking longer as we age. This renewal process is essential for maintaining skin luminosity, texture, and resilience.
The term "sluggish skin" is not a recognised medical diagnosis but rather a descriptive phrase often used to characterise skin that appears dull, lacks radiance, shows delayed healing, or demonstrates reduced responsiveness to skincare interventions. This presentation may potentially reflect underlying factors affecting cellular metabolism, including reduced microcirculation, impaired mitochondrial function, or decreased cellular energy production, though these mechanisms remain hypothetical in routine clinical care. Understanding the physiological basis of these processes helps identify evidence-based approaches to support both systemic metabolic health and skin vitality.
It is important to note that whilst metabolic rate and skin appearance are connected, the relationship is complex and influenced by numerous factors including genetics, hormonal status, nutritional intake, and environmental exposures. Claims that specific products or interventions can dramatically "activate" or "boost" metabolism should be viewed critically and evaluated against available clinical evidence.
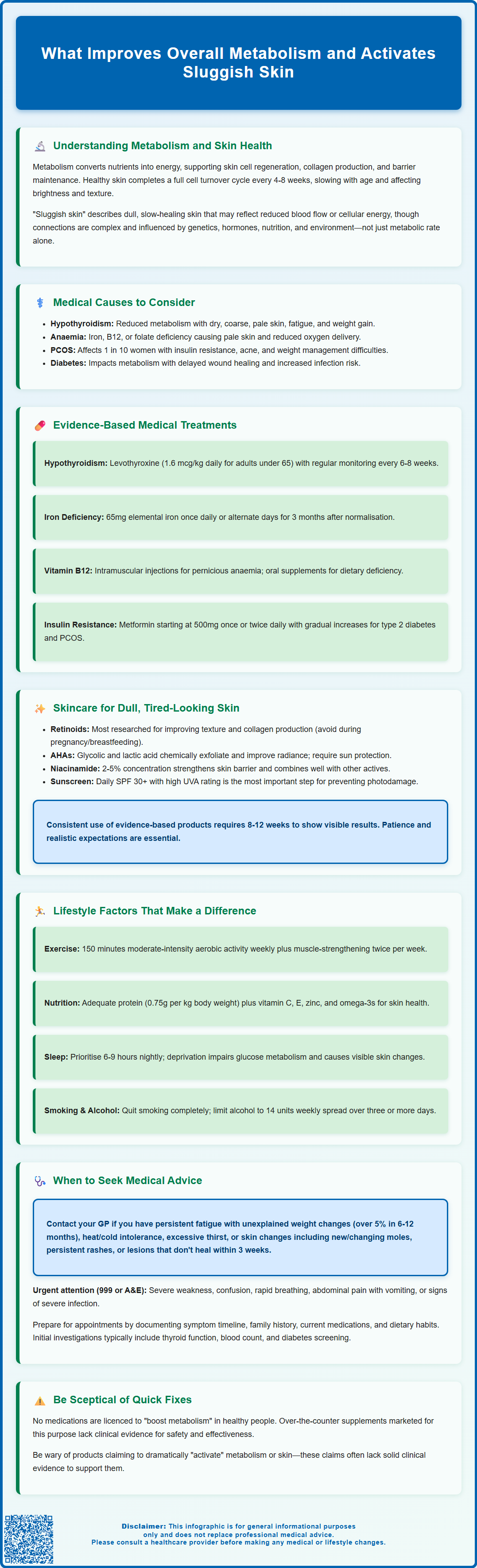
Medical Causes of Sluggish Skin and Slow Metabolism
Several medical conditions can affect both metabolic function and skin appearance, warranting clinical evaluation when symptoms are persistent or accompanied by other systemic features. Thyroid disorders, particularly hypothyroidism, represent one of the most common endocrine causes of reduced metabolic function. Patients with underactive thyroid function may experience dry, coarse, pale skin alongside fatigue, weight gain, cold intolerance, and cognitive changes. Thyroid hormones (T3 and T4) directly influence basal metabolic rate and are essential for normal skin cell turnover and sebum production.
Iron deficiency anaemia can manifest with pale, tired-looking skin due to reduced oxygen delivery to tissues. Haemoglobin carries oxygen to cells throughout the body, including dermal and epidermal layers, and inadequate iron stores impair this process. Patients may also report fatigue, breathlessness, and reduced exercise tolerance. Similarly, vitamin B12 or folate deficiency can affect skin appearance and energy metabolism, sometimes presenting with hyperpigmentation or glossitis alongside the cutaneous changes.
Polycystic ovary syndrome (PCOS) affects up to 1 in 10 women of reproductive age and involves metabolic dysfunction including insulin resistance. This condition may present with acne, hirsutism, and skin tags, alongside irregular menstruation and difficulty maintaining healthy weight. Diabetes mellitus, both type 1 and type 2, significantly impacts metabolic function and can cause various skin manifestations including delayed wound healing, increased infection susceptibility, and specific dermatological conditions such as acanthosis nigricans.
Other relevant conditions include chronic kidney disease, liver dysfunction, malabsorption disorders (such as coeliac disease or inflammatory bowel disease), and chronic inflammatory conditions. Certain medications, including beta-blockers, corticosteroids, and some antidepressants, may influence weight, glucose metabolism, fluid balance or skin appearance. When skin changes occur alongside unexplained fatigue, weight changes, or other systemic symptoms, medical evaluation is essential to identify any underlying pathology requiring specific treatment. Importantly, patients should not stop or change prescribed medications without consulting their healthcare provider.
Evidence-Based Treatments to Support Metabolic Function
Treatment approaches to support metabolic function must be tailored to any identified underlying medical condition. When hypothyroidism is diagnosed through blood tests measuring thyroid-stimulating hormone (TSH) and free thyroxine (FT4), levothyroxine replacement therapy is the standard treatment. This synthetic thyroid hormone is prescribed at individualised doses based on NICE guidance: approximately 1.6 micrograms per kilogram body weight daily for adults under 65 without cardiovascular disease, with lower starting doses (25-50 micrograms daily) for older adults or those with cardiac disease. Regular monitoring (typically every 6-8 weeks initially) is essential to achieve optimal thyroid function. Restoration of normal thyroid function generally improves both metabolic rate and associated skin changes over several months.
For iron deficiency anaemia, oral iron supplementation is first-line treatment, alongside investigation and management of the underlying cause of iron loss or malabsorption. Current UK guidance recommends once-daily or alternate-day elemental iron (e.g., ferrous sulphate providing 65mg elemental iron) to improve absorption and reduce side effects. Treatment should continue for approximately 3 months after haemoglobin levels normalise. For vitamin B12 deficiency, treatment depends on the cause: pernicious anaemia typically requires intramuscular hydroxocobalamin (1mg on alternate days for 2 weeks, then maintenance every 2-3 months), while dietary deficiency may respond to oral supplementation. Importantly, B12 deficiency should be corrected before treating folate deficiency, which typically requires folic acid 5mg daily for about 4 months.
Management of insulin resistance and metabolic syndrome follows a structured approach combining lifestyle modification with pharmacological intervention when indicated. Metformin, a biguanide medication that improves insulin sensitivity and reduces hepatic glucose production, is commonly prescribed for type 2 diabetes and may be used in PCOS management (though this is an off-label use in the UK). The typical starting dose is 500mg once or twice daily with meals, gradually increased to minimise gastrointestinal side effects. Modified-release formulations may help improve tolerance. Metformin is contraindicated in patients with eGFR below 30 mL/min/1.73m² and requires dose review when eGFR is 30-45 mL/min/1.73m². NICE recommends metformin as first-line pharmacological treatment for type 2 diabetes alongside lifestyle interventions.
It is crucial to emphasise that there are no licensed medications specifically indicated to "boost metabolism" in healthy individuals. Products marketed with such claims, including many over-the-counter supplements, lack robust clinical evidence for efficacy and safety. Any pharmacological intervention should be prescribed and monitored by a qualified healthcare professional following appropriate investigation and diagnosis.
Skincare Approaches for Dull and Tired-Looking Skin
Evidence-based topical skincare can address the appearance of dull or tired-looking skin through several mechanisms, though it is important to maintain realistic expectations about what topical products can achieve. Retinoids (vitamin A derivatives) represent the most extensively researched topical agents for improving skin texture and appearance. Tretinoin, adapalene, and other prescription retinoids (primarily licensed for acne in the UK) increase cellular turnover, stimulate collagen production, and improve epidermal organisation. Over-the-counter retinol products offer milder effects. Patients should be advised to introduce retinoids gradually, starting with 2–3 applications weekly, as they can cause initial irritation, dryness, and photosensitivity. Important safety note: Topical retinoids should be avoided during pregnancy, when planning pregnancy, or while breastfeeding, as advised by the MHRA.
Alpha-hydroxy acids (AHAs) such as glycolic acid and lactic acid function as chemical exfoliants, promoting desquamation of the stratum corneum and potentially stimulating dermal collagen synthesis at higher concentrations, though evidence for this effect is limited and varies between formulations. Products containing 5–10% AHAs are available over-the-counter, whilst higher concentrations should only be used by trained professionals in chemical peels. Patch testing is advisable before use, particularly for those with sensitive or darker skin tones, as AHAs can cause irritation and post-inflammatory hyperpigmentation. Regular use can improve skin texture and radiance, though sun protection is essential as AHAs increase photosensitivity. Vitamin C (L-ascorbic acid) serves as an antioxidant and cofactor in collagen synthesis. Formulations containing 10–20% L-ascorbic acid at pH 3.5 or below demonstrate the best stability and penetration, though the evidence for dramatic clinical effects remains modest.
Niacinamide (vitamin B3) at concentrations of 2–5% has demonstrated benefits for skin barrier function, reducing transepidermal water loss and improving skin texture in clinical studies. It is generally well-tolerated and can be combined with other active ingredients. Adequate moisturisation remains fundamental, supporting barrier function and improving the appearance of dry, dull skin. Moisturisers containing humectants (such as glycerin or hyaluronic acid), emollients, and occlusives help maintain hydration.
Sun protection is perhaps the most important skincare intervention for maintaining skin health. Daily application of broad-spectrum SPF 30 or higher with a 4-5 star UVA rating prevents photodamage, which significantly contributes to dull, uneven skin texture. Patients should be counselled that consistent, long-term use of evidence-based skincare products is necessary to see benefits, typically requiring 8–12 weeks of regular application. There is no official link between topical skincare products and systemic metabolic rate.
Lifestyle Factors That Influence Metabolism and Skin Vitality
Lifestyle modifications represent the foundation of supporting healthy metabolic function and skin appearance, with substantial evidence demonstrating their impact on both systemic health and dermatological outcomes. Regular physical activity is one of the most effective interventions for supporting metabolic health. Exercise increases energy expenditure, improves insulin sensitivity, supports cardiovascular function, and may enhance skin blood flow. Current UK Chief Medical Officers' guidelines recommend at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity activity weekly, alongside muscle-strengthening activities on two or more days per week. Whilst exercise does not permanently increase basal metabolic rate to a clinically significant degree in most individuals, resistance training may modestly increase resting metabolic rate through gains in lean muscle mass.
Nutritional intake profoundly influences both metabolism and skin health. Following the NHS Eatwell Guide provides a balanced approach to nutrition. Adults typically require approximately 0.75g of protein per kilogram body weight daily (with higher intakes of 1.0-1.2g/kg often recommended for older adults), alongside essential fatty acids, vitamins, and minerals to support cellular function throughout the body. Specific nutrients particularly relevant to skin health include:
-
Vitamin C: Essential for collagen synthesis; found in citrus fruits, berries, peppers, and leafy greens
-
Vitamin E: Functions as an antioxidant; present in nuts, seeds, and vegetable oils
-
Zinc: Supports wound healing and immune function; sources include meat, shellfish, legumes, and whole grains
-
Omega-3 fatty acids: May support skin barrier function; found in oily fish, flaxseeds, and walnuts
-
Adequate hydration: Whilst evidence that increased water intake improves skin appearance in well-hydrated individuals is limited, maintaining adequate fluid intake supports overall physiological function
Sleep quality and duration significantly impact metabolic and dermatological health. Sleep deprivation is associated with impaired glucose metabolism, increased cortisol levels, and visible changes in skin appearance including increased fine lines, reduced elasticity, and uneven pigmentation. Most adults need 6–9 hours of quality sleep nightly, according to NHS guidance. Smoking cessation is crucial, as tobacco use accelerates skin ageing through multiple mechanisms including vasoconstriction, oxidative stress, and direct toxic effects on dermal structures. Alcohol consumption should remain within recommended limits (14 units weekly spread over three or more days), as excessive intake can impair liver function, affect nutritional status, and contribute to skin dehydration and inflammation.
When to Seek Medical Advice for Skin and Metabolic Concerns
Whilst mild variations in skin appearance and energy levels are normal, certain presentations warrant medical evaluation to exclude underlying pathology. Patients should contact their GP if they experience persistent fatigue alongside unexplained weight changes (gain or loss of more than 5% body weight over 6–12 months without intentional dietary modification), as this may indicate thyroid dysfunction, diabetes, or other metabolic disorders. Additional concerning features include heat or cold intolerance, excessive thirst or urination, palpitations, tremor, or changes in bowel habit.
Skin changes requiring medical assessment include new or changing pigmented lesions (to exclude melanoma or other skin cancers), persistent rashes that do not respond to over-the-counter treatments, skin lesions that bleed or do not heal within 3 weeks, sudden onset of severe acne in adulthood, or excessive hair growth or loss. Skin manifestations of systemic disease may include yellow discolouration (suggesting liver dysfunction), bronze pigmentation (potentially indicating haemochromatosis), or velvety, hyperpigmented patches in body folds (acanthosis nigricans, associated with insulin resistance).
Urgent medical attention is required for symptoms suggesting acute metabolic decompensation, including severe weakness, confusion, rapid breathing, abdominal pain with vomiting, or signs of severe infection. Call 999 or go to A&E for life-threatening symptoms. For urgent advice when unsure, contact NHS 111. Patients with known diabetes experiencing symptoms of hypo- or hyperglycaemia should follow their individualised management plan and seek emergency care if symptoms are severe or not responding to usual measures.
When attending appointments, patients should be prepared to discuss:
-
Timeline and pattern of symptoms
-
Associated features such as fatigue, weight changes, menstrual irregularities, or mood changes
-
Family history of thyroid disease, diabetes, or autoimmune conditions
-
Current medications and supplements
-
Dietary habits and any recent changes
Initial investigation typically includes blood tests assessing thyroid function (TSH, FT4), full blood count (to identify anaemia), glucose or HbA1c (for diabetes screening), and potentially vitamin B12, folate, ferritin levels, kidney and liver function tests, and coeliac serology when indicated. Further investigations are guided by clinical findings. Early identification and management of underlying medical conditions optimises outcomes for both metabolic health and associated dermatological manifestations.
If you experience side effects from any medicines or vaccines, please report them to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or via the Yellow Card app).
Frequently Asked Questions
Can topical skincare products boost my metabolism?
No, topical skincare products do not affect systemic metabolic rate. However, evidence-based ingredients such as retinoids, alpha-hydroxy acids, and niacinamide can improve skin cell turnover and appearance locally through direct effects on skin tissue.
What medical conditions cause both slow metabolism and dull skin?
Hypothyroidism, iron deficiency anaemia, vitamin B12 deficiency, and insulin resistance (including PCOS and type 2 diabetes) can affect both metabolic function and skin appearance. These conditions require medical diagnosis through blood tests and specific treatment under GP supervision.
When should I see my GP about metabolism and skin concerns?
Contact your GP if you experience persistent fatigue with unexplained weight changes (more than 5% over 6–12 months), skin lesions that do not heal within 3 weeks, new or changing pigmented lesions, or symptoms such as heat or cold intolerance alongside skin changes.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












