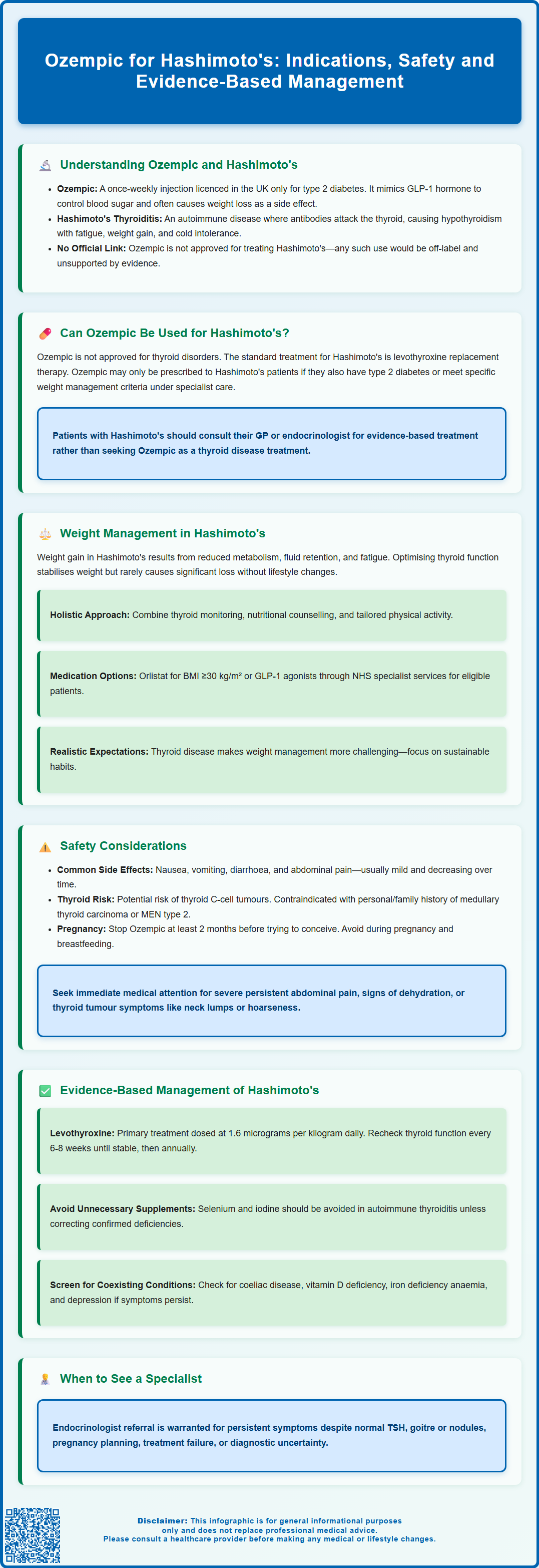
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for type 2 diabetes mellitus, not for thyroid conditions. Hashimoto's thyroiditis is an autoimmune disorder causing hypothyroidism, typically managed with levothyroxine replacement therapy. Whilst some patients with Hashimoto's experience persistent weight concerns despite optimal thyroid hormone replacement, Ozempic is not indicated for treating thyroid disease itself. This article examines the relationship between Ozempic and Hashimoto's, clarifies appropriate treatment pathways, and explores evidence-based approaches to managing weight and metabolic health in patients with autoimmune thyroid disease.
Summary: Ozempic is not licensed or indicated for treating Hashimoto's thyroiditis and should not be used for thyroid disease management.
- Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK exclusively for type 2 diabetes mellitus, not thyroid conditions.
- Hashimoto's thyroiditis is an autoimmune disorder causing hypothyroidism, treated with levothyroxine replacement therapy to normalise thyroid hormone levels.
- Ozempic may be prescribed to Hashimoto's patients only if they have coexisting type 2 diabetes meeting licensed indications.
- Rodent studies link semaglutide to thyroid C-cell tumours; patients with personal or family history of medullary thyroid carcinoma or MEN 2 require careful assessment.
- Weight management in Hashimoto's requires optimised levothyroxine therapy, lifestyle interventions, and specialist referral if additional pharmacotherapy is considered.
- NICE guidance recommends multicomponent obesity management; semaglutide 2.4 mg (Wegovy) is available through NHS specialist weight management services for eligible patients.
Table of Contents
Understanding Ozempic and Hashimoto's Thyroiditis
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. According to its Summary of Product Characteristics (SmPC), it works by mimicking the action of the naturally occurring hormone GLP-1, which stimulates insulin secretion in a glucose-dependent manner, suppresses glucagon release, slows gastric emptying, and reduces appetite. Administered as a once-weekly subcutaneous injection, Ozempic has gained considerable attention not only for its glycaemic control but also for its associated weight loss effects, which occur as a secondary benefit in many patients. It is important to note that Ozempic is not licensed for weight management in the UK.
Hashimoto's thyroiditis, also known as chronic lymphocytic thyroiditis, is an autoimmune condition and the most common cause of hypothyroidism in the UK. In this disorder, the immune system produces antibodies—primarily thyroid peroxidase (TPO) antibodies and thyroglobulin antibodies—that attack the thyroid gland, leading to progressive destruction of thyroid tissue. Over time, this results in reduced production of thyroid hormones (thyroxine and triiodothyronine), causing symptoms such as fatigue, weight gain, cold intolerance, constipation, dry skin, and cognitive difficulties.
Many individuals with Hashimoto's thyroiditis struggle with weight management, even when their thyroid hormone levels are adequately replaced with levothyroxine. This has led to interest in adjunctive therapies, including medications like Ozempic, to address metabolic concerns. However, it is important to understand that there is no official link between Ozempic and the treatment of Hashimoto's disease itself. Ozempic is not licensed for thyroid conditions, and its use in this context would be considered off-label. Understanding the distinct roles of these conditions and their treatments is essential for informed decision-making.
Can Ozempic Be Used for Hashimoto's Disease?
Ozempic is not indicated for the treatment of Hashimoto's thyroiditis or any other thyroid disorder. Its licence from the Medicines and Healthcare products Regulatory Agency (MHRA) is specifically for improving glycaemic control in adults with type 2 diabetes, either as monotherapy or in combination with other glucose-lowering medications. There is no established clinical benefit on thyroid autoimmunity or hormone production in Hashimoto's disease.
The standard treatment for Hashimoto's thyroiditis remains levothyroxine replacement therapy, which aims to restore normal thyroid hormone levels and alleviate symptoms of hypothyroidism. NICE guidance (NG145) recommends offering levothyroxine for overt hypothyroidism (elevated TSH with low free T4). For subclinical hypothyroidism (elevated TSH with normal free T4), treatment should be considered if TSH ≥10 mIU/L on two tests 3 months apart, or as a time-limited trial in symptomatic adults, especially if TPO-antibody positive. Different considerations apply for older adults.
That said, some patients with Hashimoto's may also have coexisting type 2 diabetes or meet criteria for weight management interventions. In such cases, Ozempic might be prescribed for its licensed indication of diabetes control. Alternatively, semaglutide 2.4 mg (Wegovy) is recommended by NICE (TA875) for weight management only within specialist weight management services for people meeting specific BMI and comorbidity criteria. Any decision to use semaglutide in a patient with Hashimoto's should be made by a healthcare professional after careful assessment of the individual's metabolic profile, comorbidities, and treatment goals.
Off-label use of Ozempic purely for weight loss in Hashimoto's patients without diabetes is not supported by current evidence or guidelines. Patients should not seek or use Ozempic as a treatment for thyroid disease itself, and any concerns about weight or metabolic health should be discussed with a GP or endocrinologist who can provide appropriate, evidence-based recommendations.
Weight Management in Hashimoto's Thyroiditis
Weight gain is a common and distressing symptom for many individuals with Hashimoto's thyroiditis, often persisting even after thyroid hormone replacement has normalised TSH levels. The mechanisms behind this are multifactorial and include a reduced basal metabolic rate due to hypothyroidism, fluid retention, and potential changes in appetite regulation and energy expenditure. Additionally, fatigue and reduced exercise tolerance associated with hypothyroidism can contribute to a more sedentary lifestyle, further complicating weight management.
Once thyroid function is optimised with levothyroxine, many patients find that weight stabilises, though significant weight loss may not occur without additional lifestyle interventions. NICE guidance (NG208) on obesity management emphasises a multicomponent approach, including dietary modification, increased physical activity, and behavioural support.
Currently, orlistat is a commonly prescribed weight-loss medication in the UK, licensed for adults with a BMI ≥30 kg/m², or ≥28 kg/m² with risk factors. GLP-1 receptor agonists like semaglutide 2.4 mg (Wegovy) are available through NHS specialist weight management services (Tier 3/4) for eligible patients meeting NICE TA875 criteria. It is important to note that ethnicity-adjusted BMI thresholds (e.g., 27.5 kg/m² for certain ethnic groups) inform risk assessment and some referral criteria but do not automatically change medicine licensing criteria.
Weight management in Hashimoto's should not rely solely on medication. A holistic approach that includes regular monitoring of thyroid function, nutritional counselling, and physical activity tailored to the individual's capacity is essential.
Patients should be encouraged to set realistic weight loss goals and understand that thyroid disease may make weight management more challenging. Regular follow-up with healthcare professionals, including GPs, practice nurses, and dietitians, can provide ongoing support and ensure that any additional metabolic or hormonal issues are identified and addressed appropriately.
Safety Considerations and Contraindications
When considering any medication, including Ozempic, in patients with Hashimoto's thyroiditis, several safety considerations must be taken into account. Semaglutide is generally well tolerated, but common adverse effects include gastrointestinal symptoms such as nausea, vomiting, diarrhoea, constipation, and abdominal pain. These effects are usually mild to moderate and tend to diminish over time, particularly with gradual dose escalation.
A critical safety concern with GLP-1 receptor agonists is the potential risk of thyroid C-cell tumours. In rodent studies, semaglutide was associated with an increased incidence of thyroid C-cell tumours, including medullary thyroid carcinoma (MTC). Although the relevance of these findings to humans is uncertain, the UK SmPC includes this as a precaution. Patients with a personal or family history of MTC or multiple endocrine neoplasia syndrome type 2 (MEN 2) should discuss this risk with their healthcare provider. Patients should be counselled about symptoms of thyroid tumours, such as a lump in the neck, hoarseness, dysphagia, or dyspnoea, and advised to seek medical attention if these occur.
Other important safety considerations include:
-
Pregnancy and breastfeeding: Semaglutide should be avoided during pregnancy and breastfeeding. Women of childbearing potential should use effective contraception and stop semaglutide at least 2 months before a planned pregnancy.
-
Pancreatitis: Patients should seek urgent medical attention for sudden, severe, persistent abdominal pain radiating to the back (with or without vomiting), which may indicate acute pancreatitis.
-
Gallbladder disease: Semaglutide may increase the risk of cholelithiasis and cholecystitis. Patients should seek urgent care for severe, persistent upper abdominal pain, especially if accompanied by fever or jaundice.
-
Hypoglycaemia: When used with insulin or sulfonylureas, there is an increased risk of hypoglycaemia; dose reduction of these agents may be necessary.
-
Dehydration and acute kidney injury: Severe gastrointestinal side effects may lead to dehydration. Patients should maintain adequate fluid intake and seek medical review if unable to keep fluids down.
Subcutaneous semaglutide has minimal clinically relevant effects on most oral drug absorption, including levothyroxine. However, monitoring thyroid function is advisable after significant weight change or if symptoms change. Patients should take levothyroxine consistently, ideally on an empty stomach at least 30 minutes before breakfast.
Patients are encouraged to report any suspected adverse effects to the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Evidence-Based Approaches to Managing Hashimoto's
The cornerstone of managing Hashimoto's thyroiditis is levothyroxine replacement therapy, which should be titrated to achieve a TSH level within the reference range, typically 0.4–4.0 mU/L, though individual targets may vary. NICE guidance (NG145) recommends starting with a dose of 1.6 micrograms per kilogram of body weight per day in most adults, with lower starting doses (25–50 micrograms daily) in older patients or those with cardiovascular disease. Thyroid function tests should be rechecked 6–8 weeks after initiation or dose adjustment, and annually once stable.
Beyond hormone replacement, lifestyle interventions play a vital role in managing symptoms and improving quality of life. A balanced diet rich in nutrients supports thyroid health. Routine supplementation with selenium is not recommended, and iodine supplements should be avoided in autoimmune thyroiditis. Focus should be on addressing confirmed nutritional deficiencies only.
For patients with persistent symptoms despite optimal thyroid hormone replacement, further investigation may be warranted to exclude other conditions such as coeliac disease, vitamin D deficiency, iron deficiency anaemia, or depression, all of which are more common in individuals with autoimmune thyroid disease.
Pregnancy planning requires special consideration. Women should aim for trimester-specific TSH targets, with pre-conception optimisation of thyroid function. Once pregnancy is confirmed, levothyroxine dose often needs to be increased promptly, with urgent thyroid function testing arranged.
Referral to an endocrinologist may be appropriate for:
-
Persistent symptoms with normal TSH
-
Goitre or thyroid nodules
-
Uncertain diagnosis
-
Pregnancy or planning pregnancy
-
Failed control with standard treatment
-
Significant TSH abnormalities
Patient education is essential. Individuals should understand the chronic nature of Hashimoto's, the importance of medication adherence, and when to seek medical advice—such as if they experience worsening fatigue, unexplained weight changes, palpitations, or symptoms of hyperthyroidism (which may indicate overtreatment). Empowering patients with knowledge and support enables them to take an active role in managing their condition effectively.
Scientific References
- Ozempic 0.5 mg solution for injection in pre-filled pen - Summary of Product Characteristics (SmPC).
- Thyroid disease: assessment and management. NICE guideline NG145.
- Semaglutide for managing overweight and obesity. Technology appraisal guidance TA875.
- Ozempic - European Public Assessment Report (EPAR).
- Society for Endocrinology Guidance.
- Underactive thyroid (hypothyroidism).
Frequently Asked Questions
Can Ozempic treat Hashimoto's thyroiditis?
No, Ozempic is not licensed or indicated for treating Hashimoto's thyroiditis or any thyroid disorder. It is approved in the UK only for type 2 diabetes mellitus, and the standard treatment for Hashimoto's remains levothyroxine replacement therapy.
Why do people with Hashimoto's struggle with weight management?
Weight gain in Hashimoto's results from reduced basal metabolic rate due to hypothyroidism, fluid retention, fatigue, and reduced exercise tolerance. Even with optimised levothyroxine therapy, many patients require additional lifestyle interventions including dietary modification and increased physical activity to achieve weight loss.
Are there any safety concerns using Ozempic in patients with thyroid conditions?
Rodent studies have shown semaglutide is associated with thyroid C-cell tumours, including medullary thyroid carcinoma. Patients with a personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2 should discuss this risk with their healthcare provider before considering semaglutide.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript