Mounjaro®
Dual-agonist support that helps curb appetite, hunger, and cravings to drive substantial, sustained weight loss.
- ~22.5% average body weight loss
- Significant weight reduction
- Improves blood sugar levels
- Clinically proven weight loss
Does Ozempic help PCOS weight loss? This question reflects growing interest in GLP-1 receptor agonists for managing polycystic ovary syndrome (PCOS), a condition affecting 1 in 10 UK women. Whilst Ozempic (semaglutide) is licensed for type 2 diabetes and has demonstrated weight loss effects, it is not currently approved for PCOS treatment in the UK. Women with PCOS face unique metabolic challenges, including insulin resistance and hormonal imbalances, which complicate weight management. This article examines the evidence, NHS guidance, safety considerations, and alternative evidence-based approaches for PCOS-related weight management.
Summary: Ozempic is not licensed for PCOS or weight loss in people without diabetes in the UK, though it may secondarily benefit PCOS symptoms in women prescribed it for type 2 diabetes.
Polycystic ovary syndrome (PCOS) affects approximately 1 in 10 women in the UK and represents one of the most common endocrine disorders of reproductive age. The condition is characterised by hormonal imbalances, irregular menstrual cycles, elevated androgen levels, and often (though not always) polycystic ovaries. According to the Rotterdam criteria, diagnosis requires two of these three features. Weight management presents a particularly complex challenge for women with PCOS due to the underlying metabolic dysfunction associated with the condition.
Women with PCOS frequently experience insulin resistance, where the body's cells become less responsive to insulin, leading to elevated blood glucose levels and compensatory hyperinsulinaemia. This metabolic disturbance creates a vicious cycle: excess insulin promotes fat storage (particularly around the abdomen), stimulates androgen production from the ovaries, and makes weight loss more challenging. Studies suggest that approximately 50–70% of women with PCOS have some degree of insulin resistance, regardless of their body mass index (BMI).
The weight management challenges extend beyond simple caloric balance. Many women with PCOS report that traditional diet and exercise approaches may yield slower or less substantial results compared to what might be expected. This can lead to frustration, reduced motivation, and psychological distress. The excess weight itself worsens insulin resistance and hormonal imbalances, creating additional barriers to achieving a healthy weight. Furthermore, the hormonal disruptions associated with PCOS can affect appetite regulation, energy levels, and metabolism, compounding the difficulty of sustainable weight loss.
Given these challenges, there has been growing interest in pharmacological interventions that address the underlying metabolic dysfunction in PCOS, rather than relying solely on lifestyle modifications. This has led to increased attention on medications originally developed for type 2 diabetes, including GLP-1 receptor agonists such as Ozempic (semaglutide).
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. It is important to distinguish Ozempic from Wegovy, which is also semaglutide but at a higher maximum dose (2.4 mg) and is specifically licensed for weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity.
Semaglutide mimics the action of naturally occurring GLP-1, a hormone produced in the intestines in response to food intake. It works through several complementary mechanisms. Firstly, semaglutide stimulates glucose-dependent insulin secretion from pancreatic beta cells, meaning it increases insulin release only when blood glucose levels are elevated. This reduces the risk of hypoglycaemia when used alone. Secondly, it suppresses glucagon secretion from pancreatic alpha cells, which helps prevent excessive glucose production by the liver.
Perhaps most relevant to weight management, semaglutide acts on appetite regulation centres in the brain, particularly in the hypothalamus and brainstem. It slows gastric emptying, prolonging the sensation of fullness after meals, and reduces appetite through central nervous system pathways. Clinical trials in people with type 2 diabetes using Ozempic have demonstrated weight loss, with participants typically losing around 3-7% of their body weight at therapeutic doses (0.5-1 mg weekly). The higher-dose Wegovy formulation (2.4 mg) has shown greater weight loss of approximately 15% in clinical trials for obesity management.
For women with PCOS, these mechanisms are potentially relevant because they address multiple aspects of the condition: improving glycaemic control, reducing hyperinsulinaemia, and facilitating weight loss which may secondarily improve insulin sensitivity. The medication is administered as a once-weekly subcutaneous injection, with doses typically starting at 0.25 mg (an initiation dose for tolerability, not therapeutic effect) and gradually increasing according to the licensed titration schedule. It is crucial to emphasise that Ozempic is not currently licensed for PCOS treatment or weight loss in people without diabetes in the UK, and should not be co-administered with other GLP-1 receptor agonists.
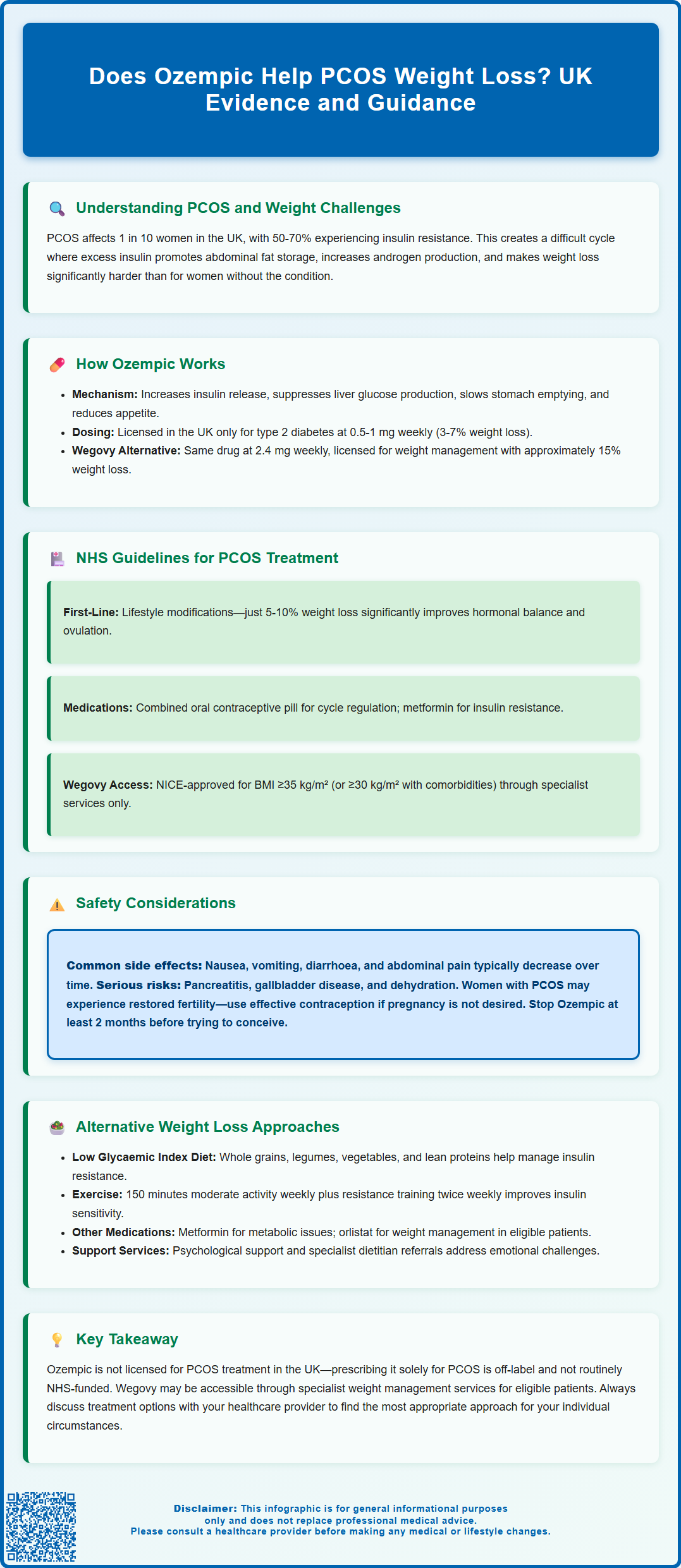
The NHS Clinical Knowledge Summary (CKS) on PCOS provides guidance on management, though current recommendations do not include Ozempic as a treatment for PCOS. According to NHS guidance, the cornerstone of PCOS management involves lifestyle modifications, including dietary changes and increased physical activity, particularly for women who are overweight or obese. Weight loss of just 5–10% of body weight can significantly improve hormonal balance, restore ovulation, and reduce metabolic complications.
First-line pharmacological treatments for PCOS typically include the combined oral contraceptive pill (COCP) to regulate menstrual cycles and reduce androgen levels, helping with symptoms like hirsutism and acne. Anti-androgen medications may be considered for persistent symptoms despite COCP use.
For women with PCOS and insulin resistance, metformin is commonly prescribed within the NHS framework. Metformin improves insulin sensitivity and can assist with modest weight loss, though it is not licensed specifically for PCOS in the UK. It is particularly considered for women with PCOS who have not responded adequately to lifestyle interventions, especially those with glucose intolerance or type 2 diabetes. The typical dose ranges from 500 mg to 2,000 mg daily, taken with meals to minimise gastrointestinal side effects.
Regarding GLP-1 receptor agonists, Wegovy (semaglutide 2.4 mg) is now licensed and recommended by NICE (TA875) for weight management in adults with a BMI ≥35 kg/m² (or ≥30 kg/m² with weight-related comorbidities) who have been referred to specialist weight management services. Ozempic is licensed only for type 2 diabetes mellitus. Some women with PCOS who also have type 2 diabetes may be prescribed Ozempic as part of their diabetes management, which may secondarily benefit their PCOS symptoms. However, prescribing Ozempic solely for PCOS or weight management in the absence of diabetes would be considered off-label use and is not routinely funded by the NHS. There are currently supply constraints affecting GLP-1 receptor agonists, and NHS England has issued alerts discouraging off-label prescribing of Ozempic for weight loss.
Women seeking treatment for PCOS should consult their GP or specialist endocrinologist to discuss appropriate, evidence-based options. The NHS approach emphasises individualised care, considering factors such as BMI, metabolic health, fertility goals, and symptom severity.
While Ozempic has demonstrated efficacy for glycaemic control and weight loss, it is essential to understand the potential adverse effects and safety considerations before considering its use. The most commonly reported side effects are gastrointestinal in nature and include nausea, vomiting, diarrhoea, constipation, and abdominal pain. These symptoms typically occur during the initial weeks of treatment or following dose increases, and often diminish over time as the body adjusts to the medication.
More serious, though less common, adverse effects require careful monitoring. Pancreatitis (inflammation of the pancreas) has been reported in patients taking GLP-1 receptor agonists, presenting with severe abdominal pain that may radiate to the back. Patients should be advised to seek immediate medical attention if they experience persistent, severe abdominal pain. The UK SmPC notes findings of thyroid C-cell tumours in rodent studies, though the relevance to humans remains uncertain.
Additional safety considerations include the risk of gallbladder disease (including cholelithiasis and cholecystitis), particularly with substantial weight loss. Severe gastrointestinal adverse reactions can lead to dehydration and acute kidney injury in susceptible individuals. In people with diabetes and pre-existing diabetic retinopathy, rapid improvement in glucose control has been associated with temporary worsening of retinopathy.
For women with PCOS specifically, there are additional considerations. Weight loss associated with semaglutide may restore ovulation in women who were previously anovulatory, potentially leading to unplanned pregnancy. Women of reproductive age should be counselled about effective contraception if pregnancy is not desired. Semaglutide should be discontinued at least 2 months before a planned pregnancy and is not recommended during pregnancy or breastfeeding.
Patient safety advice includes:
Contact your GP immediately if you experience severe abdominal pain, persistent vomiting, or signs of pancreatitis
Report any unusual symptoms including severe abdominal pain, jaundice, or dark urine
Be aware of hypoglycaemia symptoms if taking other diabetes medications (particularly insulin or sulfonylureas)
Ensure adequate hydration, especially during episodes of gastrointestinal upset
Discuss pregnancy plans with your healthcare provider and stop treatment at least 2 months before trying to conceive
Ozempic should only be used under medical supervision, with regular monitoring of weight, metabolic parameters, and potential adverse effects. Suspected side effects should be reported through the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk or the Yellow Card app).
Given the current limitations of Ozempic availability through the NHS for PCOS, and the importance of evidence-based approaches, women should be aware of alternative strategies that have demonstrated effectiveness for PCOS-related weight management. These approaches often work synergistically and may be combined for optimal results.
Dietary interventions form the foundation of PCOS management. Research suggests that low glycaemic index (GI) diets, which minimise blood sugar spikes, may be particularly beneficial for women with insulin resistance. This approach emphasises whole grains, legumes, vegetables, lean proteins, and healthy fats whilst limiting refined carbohydrates and sugary foods. Some women find success with Mediterranean-style eating patterns, which have been associated with improved insulin sensitivity and cardiovascular health. Portion control and regular meal timing can also help regulate insulin levels throughout the day.
Physical activity plays a crucial role beyond simple calorie expenditure. Both aerobic exercise (such as brisk walking, cycling, or swimming) and resistance training improve insulin sensitivity, even in the absence of significant weight loss. The UK Chief Medical Officers recommend at least 150 minutes of moderate-intensity activity per week, plus muscle-strengthening activities on at least two days. High-intensity interval training (HIIT) has shown promise in improving metabolic markers in women with PCOS, though any sustainable increase in activity is beneficial.
Pharmacological alternatives include metformin, as previously mentioned, which remains the most commonly prescribed medication for PCOS-related metabolic dysfunction. Inositol supplements (particularly myo-inositol and D-chiro-inositol) have emerging evidence for improving insulin sensitivity and ovarian function, though these are supplements rather than licensed medicines and more research is needed. Orlistat, a lipase inhibitor that reduces fat absorption, is licensed for weight management in the UK and may be prescribed for adults with a BMI ≥30 kg/m² (or ≥28 kg/m² with comorbidities), with appropriate monitoring for nutritional adequacy and side effects.
Psychological support should not be overlooked. Many women with PCOS experience anxiety, depression, or disordered eating patterns. Cognitive behavioural therapy (CBT) and support groups can address the emotional aspects of living with PCOS and facilitate sustainable lifestyle changes. Referral to specialist dietitians with PCOS expertise can provide personalised nutritional guidance.
For women who have not achieved adequate results with conservative measures, bariatric surgery may be considered in severe obesity (BMI ≥40 kg/m² or ≥35 kg/m² with comorbidities) after assessment in specialist Tier 3 weight management services, as per NICE guidance. Surgical interventions have demonstrated improvements in PCOS symptoms, insulin resistance, and fertility outcomes, though they carry surgical risks and require lifelong dietary modifications and monitoring.
Ozempic is not routinely funded by the NHS for PCOS or weight loss without diabetes. It is licensed only for type 2 diabetes mellitus, and prescribing it solely for PCOS would be considered off-label use.
NHS guidance recommends lifestyle modifications including dietary changes and increased physical activity as first-line treatment. Metformin may be prescribed for insulin resistance, particularly when lifestyle interventions have not achieved adequate results.
Common side effects include gastrointestinal symptoms such as nausea and vomiting. Serious but rare risks include pancreatitis and gallbladder disease. Additionally, weight loss may restore ovulation, potentially leading to unplanned pregnancy if effective contraception is not used.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
Unordered list
Bold text
Emphasis
Superscript
Subscript