Does Ozempic affect TSH levels? This question concerns many patients prescribed semaglutide for type 2 diabetes. Ozempic is a GLP-1 receptor agonist that improves blood glucose control and often leads to weight reduction. While animal studies raised theoretical thyroid concerns, current clinical evidence does not demonstrate that Ozempic directly affects TSH levels in humans. The MHRA and EMA have reviewed extensive safety data without establishing a link between semaglutide and thyroid function changes. Understanding the actual evidence helps patients and clinicians make informed decisions about this widely prescribed diabetes medication.
Summary: Current clinical evidence does not demonstrate that Ozempic directly affects TSH levels in humans.
- Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes treatment.
- The MHRA and EMA have not established a link between Ozempic use and TSH level changes in clinical practice.
- Routine thyroid function monitoring is not required for patients taking Ozempic unless specific clinical indications exist.
- Thyroid dysfunction occurs more frequently in people with diabetes independently of their treatment.
- Substantial weight loss from Ozempic may modestly affect thyroid function and levothyroxine requirements in some patients.
Table of Contents
Understanding Ozempic and Thyroid Function
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the United Kingdom for the treatment of type 2 diabetes mellitus. The medication works by mimicking the action of naturally occurring GLP-1, a hormone that stimulates insulin secretion in a glucose-dependent manner in response to food intake, suppresses glucagon release, slows gastric emptying, and reduces appetite. This glucose-dependent action helps reduce hypoglycaemia risk. These combined effects help improve glycaemic control and often result in weight loss, which has led to its increasing use in clinical practice.
The thyroid gland produces hormones that regulate metabolism, energy production, and numerous bodily functions. Thyroid-stimulating hormone (TSH), produced by the pituitary gland, controls the thyroid's production of thyroxine (T4) and triiodothyronine (T3). TSH levels are routinely measured to assess thyroid function, with elevated TSH typically indicating hypothyroidism (underactive thyroid) and suppressed TSH suggesting hyperthyroidism (overactive thyroid).
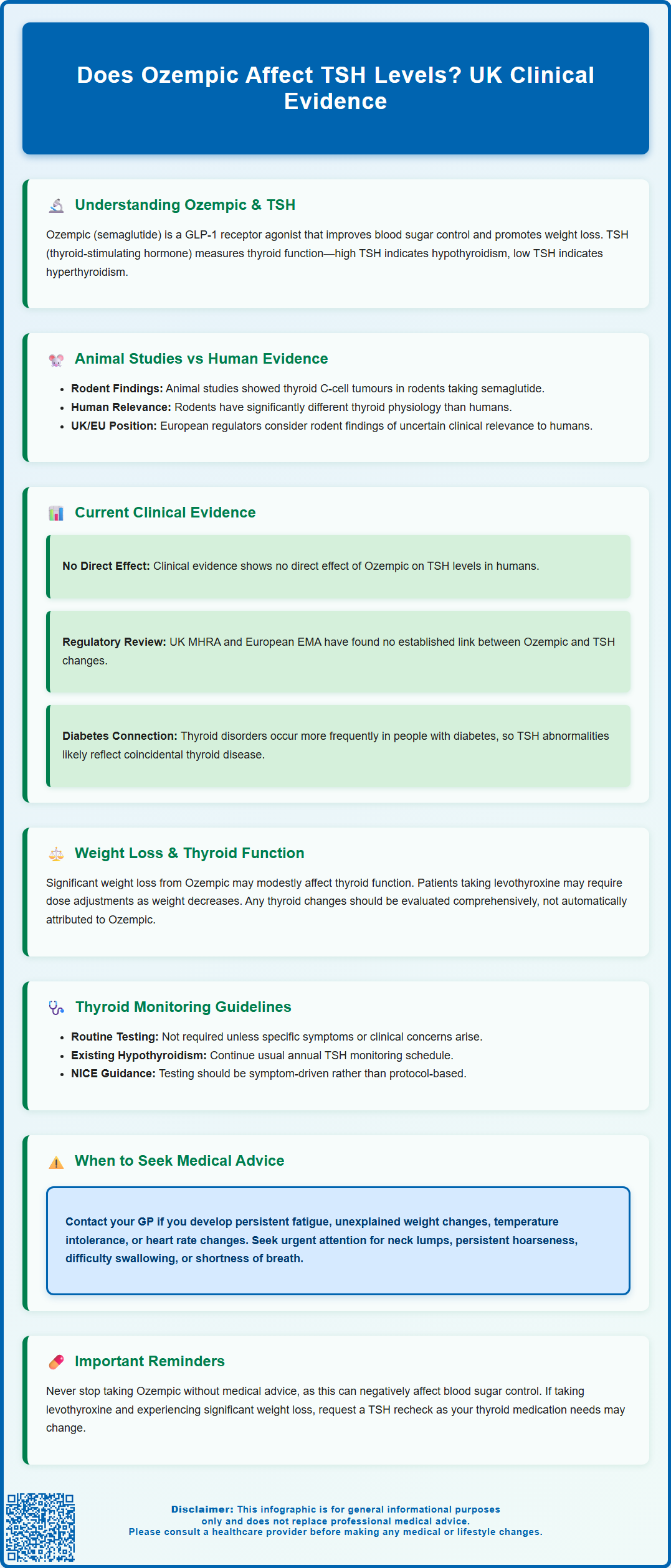
Concerns about GLP-1 receptor agonists and thyroid function arose primarily from preclinical animal studies, particularly in rodents, where semaglutide and similar medications were associated with thyroid C-cell tumours, including medullary thyroid carcinoma. However, the relevance of these animal findings to human patients remains uncertain, as rodents have substantially different thyroid physiology compared to humans. According to the European Medicines Agency's assessment, these rodent findings are of uncertain clinical relevance to humans, and unlike in the US, there is no contraindication for patients with a history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2 in the UK and EU prescribing information.
Does Ozempic Affect TSH Levels?
Current clinical evidence does not demonstrate a direct effect of Ozempic on TSH levels in humans, though thyroid function tests were not systematically reported in all clinical trials. The available data from clinical studies involving semaglutide have not identified clinically significant changes in thyroid function parameters. The Summary of Product Characteristics for Ozempic does not list thyroid function abnormalities or TSH alterations as recognised adverse effects of the medication.
The Medicines and Healthcare products Regulatory Agency (MHRA) and the European Medicines Agency (EMA) have reviewed extensive safety data for semaglutide, and there is no official link established between Ozempic use and changes in TSH levels in clinical practice. The European Public Assessment Report (EPAR) for Ozempic discusses the preclinical thyroid findings but does not identify thyroid function changes as a safety concern in humans based on clinical trial data.
It is important to recognise that patients with type 2 diabetes may have pre-existing thyroid disorders or develop them independently of their diabetes treatment. Thyroid dysfunction occurs more frequently in people with diabetes than in the general population, with autoimmune thyroid disease being particularly associated with type 1 diabetes. Therefore, if TSH abnormalities are detected in a patient taking Ozempic, this more likely reflects coincidental thyroid disease rather than a medication effect.
It's worth noting that substantial weight loss, which can occur with Ozempic therapy, may itself modestly affect thyroid function parameters and potentially reduce levothyroxine requirements in patients already receiving thyroid replacement therapy. Any changes in thyroid function should be evaluated comprehensively, considering the patient's medical history, symptoms, and other potential contributing factors rather than automatically attributing them to semaglutide therapy.
Thyroid Monitoring While Taking Ozempic
Routine thyroid function monitoring is not required for patients taking Ozempic unless there are specific clinical indications. The Summary of Product Characteristics for semaglutide does not recommend regular TSH testing as part of standard monitoring during treatment. Similarly, routine calcitonin measurement or thyroid ultrasound screening is not recommended in the UK and EU, unlike some other jurisdictions.
For patients with pre-existing thyroid disease, particularly those already receiving levothyroxine replacement therapy for hypothyroidism, continuing their usual thyroid monitoring schedule is appropriate. This typically involves annual TSH testing, though more frequent monitoring may be necessary if thyroid medication doses are being adjusted. Patients experiencing significant weight loss on Ozempic may require TSH rechecking and potential levothyroxine dose adjustment, as weight loss can alter thyroid hormone requirements.
Patients who develop symptoms suggestive of thyroid dysfunction whilst taking Ozempic should undergo thyroid function testing. Hypothyroid symptoms include fatigue, weight gain, cold intolerance, constipation, dry skin, and cognitive slowing, whilst hyperthyroid symptoms encompass weight loss, heat intolerance, palpitations, tremor, and anxiety. However, some of these symptoms overlap with either diabetes itself or expected effects of GLP-1 therapy, particularly weight changes and gastrointestinal symptoms, making clinical assessment essential.
NICE guidance (NG28) on type 2 diabetes management does not specify additional thyroid monitoring requirements for patients prescribed GLP-1 receptor agonists. Standard diabetes care includes periodic comprehensive reviews, during which clinicians should remain alert to symptoms suggesting thyroid dysfunction and arrange appropriate investigations when clinically indicated rather than following a protocol of routine screening.
When to Seek Medical Advice About Thyroid Symptoms
Patients taking Ozempic should contact their GP or diabetes care team if they develop symptoms that might indicate thyroid problems, though it is important to emphasise that such symptoms are unlikely to be caused by the medication itself. Persistent fatigue that interferes with daily activities, unexplained weight changes beyond those expected from the medication's appetite effects, or new onset of heat or cold intolerance warrant medical review. Changes in heart rate, particularly a persistently rapid or irregular heartbeat, should prompt earlier assessment.
In line with NICE guidance (NG12) on suspected cancer referral, specific symptoms requiring urgent medical attention include the development of a lump or swelling in the neck, persistent hoarseness or voice changes, difficulty swallowing, or shortness of breath, as these could indicate thyroid enlargement or, rarely, thyroid malignancy. Whilst there is no established link between Ozempic and thyroid cancer in humans, any neck mass requires prompt evaluation regardless of medication history. Patients should attend their GP surgery for assessment rather than discontinuing Ozempic without medical advice, as abrupt cessation may adversely affect glycaemic control.
For patients with known thyroid disease who are stable on levothyroxine replacement, significant changes in symptoms previously well-controlled by treatment should trigger medical review. This includes recurrence of hypothyroid or hyperthyroid symptoms, which might indicate that thyroid medication doses require adjustment. Patients experiencing substantial weight loss on Ozempic who are also taking levothyroxine should consider having their TSH levels rechecked, as weight loss can reduce levothyroxine requirements in some cases.
Healthcare professionals should maintain open communication with patients about the distinction between theoretical risks identified in animal studies and actual clinical evidence in humans. This helps prevent unnecessary anxiety whilst ensuring patients remain appropriately vigilant about symptoms requiring medical assessment. The NHS provides helpful resources on both underactive and overactive thyroid conditions that can guide patients in recognising symptoms requiring medical attention. Any concerns about continuing Ozempic therapy should be discussed with the prescribing clinician, who can provide individualised advice based on the patient's complete medical history, current symptoms, and overall benefit-risk profile of treatment.
Frequently Asked Questions
Do I need regular thyroid tests while taking Ozempic?
Routine thyroid function monitoring is not required for patients taking Ozempic unless you have pre-existing thyroid disease or develop symptoms suggesting thyroid dysfunction. The Summary of Product Characteristics does not recommend regular TSH testing as part of standard monitoring during treatment.
Can Ozempic cause thyroid problems in humans?
Current clinical evidence does not demonstrate that Ozempic causes thyroid problems in humans. While animal studies showed thyroid concerns in rodents, the MHRA and EMA have reviewed extensive human safety data without identifying thyroid function changes as a recognised adverse effect.
Should I stop taking Ozempic if my TSH levels change?
Do not stop Ozempic without medical advice, as abrupt cessation may adversely affect your blood glucose control. TSH changes in patients taking Ozempic more likely reflect coincidental thyroid disease rather than a medication effect and should be discussed with your GP or diabetes care team for proper evaluation.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript