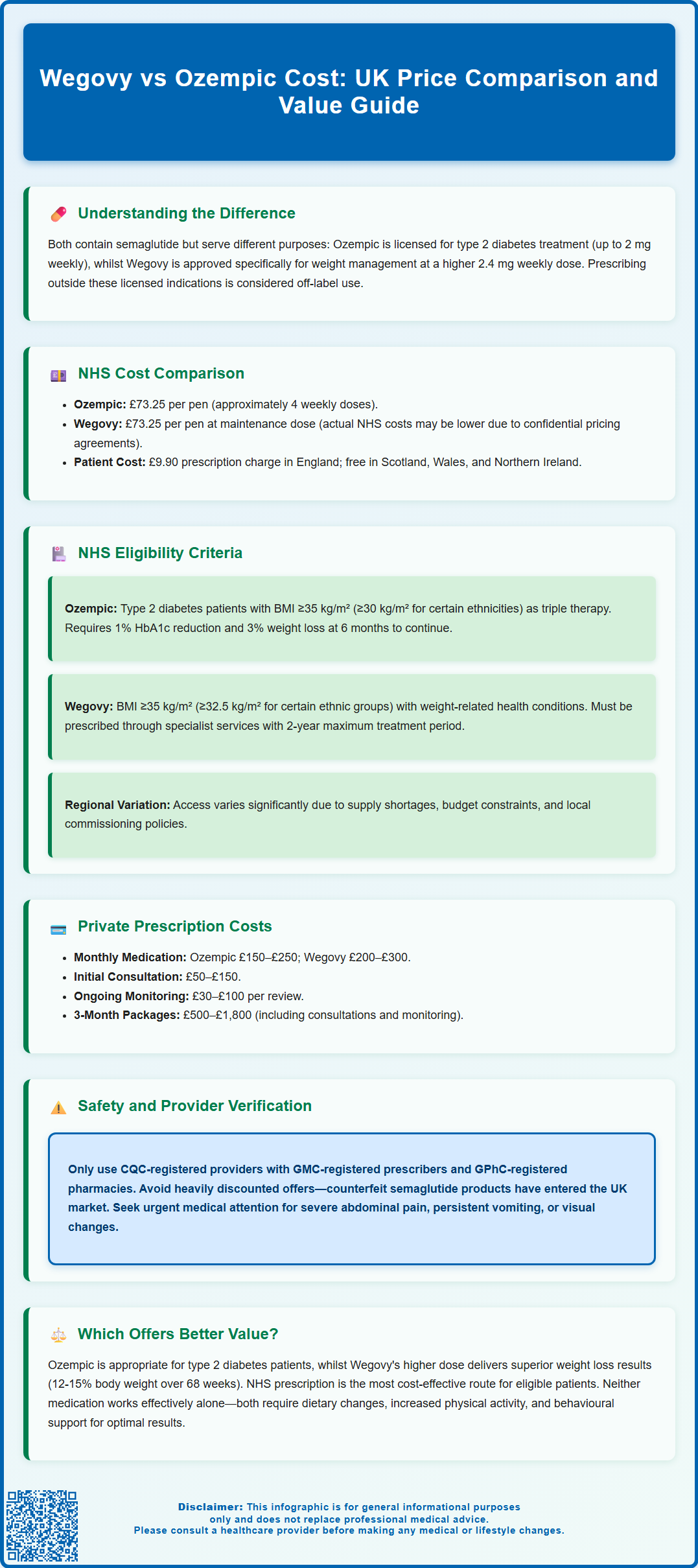
Wegovy vs Ozempic cost is a common concern for patients considering semaglutide treatment in the UK. Whilst both medications contain the same active ingredient—a GLP-1 receptor agonist—they differ significantly in licensed indications, dosing, and pricing. Ozempic is approved for type 2 diabetes management, whilst Wegovy is specifically licensed for weight management in adults with obesity or overweight with comorbidities. Understanding the cost differences, NHS eligibility criteria, and private prescription options is essential for making informed treatment decisions. This article examines the financial and clinical considerations to help patients navigate their options.
Summary: Wegovy typically costs £200–£300 monthly privately (£73.25 NHS list price), whilst Ozempic costs £150–£250 privately (£73.25 NHS list price), with NHS availability determined by strict eligibility criteria for their respective licensed indications.
- Both medications contain semaglutide, a GLP-1 receptor agonist, but Ozempic is licensed for type 2 diabetes whilst Wegovy is licensed for weight management.
- Wegovy uses a higher maintenance dose (2.4 mg weekly) compared to Ozempic's maximum diabetes dose (2 mg weekly).
- NHS access to Ozempic requires confirmed type 2 diabetes diagnosis; Wegovy requires BMI ≥35 kg/m² with comorbidities and specialist service referral.
- Private prescription costs include consultation fees, monitoring, and medication supply, with significant variation between providers.
- Both medications require long-term use for sustained benefit, with weight regain common after discontinuation.
- Treatment should be combined with lifestyle modification and is contraindicated in pregnancy; patients require regular monitoring for adverse effects including pancreatitis.
Table of Contents
Understanding Wegovy and Ozempic: What's the Difference?
Wegovy and Ozempic are both brand names for medications containing semaglutide, a glucagon-like peptide-1 (GLP-1) receptor agonist. Despite sharing the same active ingredient, these medications are licensed for different therapeutic indications and are available in different dosing regimens.
Ozempic is primarily licensed for the treatment of type 2 diabetes mellitus. It works by stimulating insulin secretion in a glucose-dependent manner, suppressing glucagon release, and slowing gastric emptying. This helps to improve glycaemic control in adults with type 2 diabetes. Ozempic is available in pre-filled pens containing doses of 0.25 mg, 0.5 mg, 1 mg, and 2 mg for once-weekly subcutaneous injection. Treatment typically begins with 0.25 mg weekly for 4 weeks, then increases to 0.5 mg, with further increases to 1 mg or 2 mg if needed for glycaemic control. Weight loss is a recognised secondary benefit observed in clinical trials, though this is not the primary indication.
Wegovy, by contrast, is specifically licensed for weight management in adults with obesity (BMI ≥30 kg/m²) or those who are overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity, such as hypertension, dyslipidaemia, or obstructive sleep apnoea. In the UK, Wegovy is also licensed for adolescents aged 12 years and older with obesity (BMI ≥30 kg/m²), although NHS funding currently focuses on adults. Wegovy is administered as a once-weekly subcutaneous injection, with a dose escalation schedule reaching a maintenance dose of 2.4 mg weekly—higher than the maximum Ozempic dose used for diabetes.
Whilst both medications utilise the same pharmacological mechanism, the key distinction lies in their licensed indications, dosing schedules, and regulatory approval pathways. The Medicines and Healthcare products Regulatory Agency (MHRA) has approved each medication for its specific indication, and prescribing outside these licensed uses would constitute off-label prescribing. Off-label prescribing requires additional considerations, including explicit informed consent, documented rationale, and careful assessment of evidence, risks and benefits, in line with General Medical Council guidance.
Wegovy vs Ozempic Cost Comparison in the UK
The cost difference between Wegovy and Ozempic in the UK reflects their different licensing, supply arrangements, and market positioning. Understanding these cost variations is essential for patients considering either medication, whether through NHS or private routes.
Ozempic pricing in the UK is consistent across dose strengths. According to the British National Formulary (BNF), the NHS indicative price for Ozempic is approximately:
-
0.25 mg/0.5 mg pre-filled pen (1.5 ml): £73.25 per pen
-
1 mg pre-filled pen (3 ml): £73.25 per pen
-
2 mg pre-filled pen (3 ml): £73.25 per pen
Each pen typically provides four weekly doses at maintenance dose, making the monthly cost approximately £73.25 for most patients. These prices represent the list cost to the NHS and may differ in private settings.
Wegovy pricing is generally higher, reflecting its specific formulation and licensed indication for weight management. The NHS list price for Wegovy maintenance dose (2.4 mg) is approximately £73.25 per pen (4-week supply), though the actual NHS acquisition cost may be lower due to a confidential commercial arrangement under NICE guidance (TA875). The initial titration phase, which involves lower doses over several weeks, has similar list pricing per pen.
In private prescription settings, costs can vary considerably between pharmacies and online providers. Private Ozempic prescriptions typically range from £150–£250 per month, whilst Wegovy private prescriptions commonly cost £200–£300 monthly. These prices usually include consultation fees, prescription charges, and medication supply. Prices should be checked at the time of prescription as they are subject to change.
It is important to note that supply constraints have affected both medications periodically, with the MHRA and NHS England implementing measures to prioritise supply for licensed indications. Price variations may also reflect market demand, pharmacy dispensing fees, and whether the prescription includes clinical monitoring and follow-up consultations.
NHS Availability and Prescription Criteria
Access to Wegovy and Ozempic through the NHS is governed by strict eligibility criteria aligned with their licensed indications and NICE (National Institute for Health and Care Excellence) guidance. Understanding these criteria is essential for patients considering NHS-funded treatment.
Ozempic NHS availability is determined by NICE guidance (NG28) for type 2 diabetes management. Ozempic may be prescribed on the NHS when:
-
The patient has a confirmed diagnosis of type 2 diabetes mellitus
-
It is used as part of a treatment strategy that includes triple therapy or where insulin is not appropriate
-
The patient has a BMI ≥35 kg/m² (or ≥30 kg/m² in people of certain ethnicities with increased diabetes risk) or weight-related comorbidities
-
The patient has specific problems with high-dose insulin or would benefit from weight loss
Continuation criteria apply at 6 months: treatment should only continue if there has been a beneficial metabolic response (reduction in HbA1c of at least 11 mmol/mol [1%] and weight loss of at least 3% of initial body weight).
Ozempic is not routinely funded by the NHS solely for weight management in patients without diabetes, as this constitutes off-label use outside its marketing authorisation.
Wegovy NHS availability has been more restricted due to supply constraints and commissioning decisions. NICE published guidance (TA875) recommending Wegovy for weight management in specific circumstances, but implementation has been phased. Current NHS eligibility criteria for Wegovy typically require:
-
BMI ≥35 kg/m² (or ≥32.5 kg/m² for certain ethnic groups with higher risk)
-
At least one weight-related comorbidity
-
Previous engagement with specialist weight management services
-
Participation in a structured lifestyle modification programme
Importantly, NICE TA875 specifies that Wegovy should only be prescribed within specialist weight management services with multidisciplinary team support, and treatment is limited to a maximum of 2 years.
Many NHS areas have implemented waiting lists or restricted access due to supply limitations and budget considerations. Patients should consult their GP to determine local commissioning policies and eligibility. The NHS has prioritised patients with the highest clinical need, and availability may vary significantly between different integrated care boards (ICBs) across England, with separate arrangements in Scotland, Wales, and Northern Ireland.
Private Prescription Costs and Payment Options
For patients who do not meet NHS eligibility criteria or face lengthy waiting times, private prescription options provide an alternative route to access Wegovy or Ozempic. However, this involves significant out-of-pocket costs and requires careful consideration.
Private consultation and prescription fees typically include:
-
Initial medical consultation: £50–£150 (in-person or online)
-
Ongoing monitoring consultations: £30–£100 per review
-
Prescription fees: Often included in consultation or £10–£30 separately
-
Medication cost: £150–£300 per month depending on the drug and dose
Many private providers offer package deals that bundle consultations, prescriptions, and medication supply for 3–6 month periods, potentially reducing overall costs. These packages typically range from £500–£1,800 for a three-month supply, including clinical support.
Online prescribing services have become increasingly popular, offering remote consultations via video or questionnaire-based assessments. Whilst often more affordable than traditional private clinics, patients should ensure providers are registered with the Care Quality Commission (CQC), employ GMC-registered prescribers, and dispense through GPhC-registered pharmacies. Reputable services include baseline health checks, regular monitoring, and access to clinical support.
Payment options vary by provider but commonly include:
-
One-off payments for monthly supplies
-
Subscription models with monthly direct debits
-
Instalment plans for longer treatment courses
-
Some providers accept medical insurance, though coverage is rare for weight management medications
Important safety considerations: These medications are contraindicated during pregnancy and breastfeeding. Women of childbearing potential should use effective contraception and stop treatment at least 2 months before a planned pregnancy. Patients should be aware of red flag symptoms requiring urgent medical attention, including severe or persistent abdominal pain (possible pancreatitis), persistent vomiting/dehydration, symptoms of gallstones, and visual changes (potential diabetic retinopathy). Those taking insulin or sulfonylureas may need dose adjustments to prevent hypoglycaemia.
Patients should be cautious of significantly discounted offers or suppliers that do not require thorough medical assessment. The MHRA has warned about counterfeit semaglutide products entering the UK market. Always verify that medications are sourced from licensed UK pharmacies and that prescribers conduct appropriate medical assessments, including contraindication screening and monitoring plans. Patients with cardiovascular disease, renal impairment, or history of pancreatitis require particularly careful evaluation before commencing treatment. Suspected side effects should be reported via the MHRA Yellow Card scheme.
Which Treatment Offers Better Value for Money?
Determining which treatment offers better value requires consideration beyond simple price comparison, encompassing clinical appropriateness, treatment outcomes, and individual patient circumstances.
For patients with type 2 diabetes, Ozempic represents the appropriate choice, as it is licensed for this indication and may be available through NHS prescription. The dual benefits of improved glycaemic control and weight loss make it clinically valuable for this population. Using Wegovy off-label for diabetes management would not be appropriate and would incur unnecessary additional costs without therapeutic advantage.
For patients seeking weight management without diabetes, Wegovy is the licensed option, though the higher cost reflects its specific formulation and dosing. The 2.4 mg maintenance dose has demonstrated superior weight loss outcomes in clinical trials compared to lower semaglutide doses. The STEP clinical trial programme showed average weight loss of 12–15% of body weight over 68 weeks with Wegovy, alongside improvements in cardiovascular risk factors. However, extension studies have shown that weight regain is common after discontinuation.
Cost-effectiveness considerations should include:
-
Treatment duration: Both medications typically require long-term use, with weight regain common after discontinuation. For Wegovy, NICE guidance (TA875) limits NHS-funded treatment to a maximum of 2 years
-
Monitoring costs: Regular follow-up, blood tests, and clinical reviews add to overall expenditure
-
Potential cost savings: Successful weight management may reduce costs associated with obesity-related complications, including diabetes, cardiovascular disease, and joint problems
-
Alternative options: Lifestyle interventions, other weight management medications (such as orlistat), or bariatric surgery may offer different cost-benefit profiles
Value for money ultimately depends on individual circumstances. Patients meeting NHS criteria should pursue this route first, as out-of-pocket costs are limited to prescription charges (currently £9.90 per item in England as of April 2024, free in Scotland, Wales, and Northern Ireland). For private patients, the decision should be made in consultation with a qualified healthcare professional, considering clinical suitability, financial sustainability over the likely treatment duration, and realistic expectations about outcomes. Neither medication should be viewed as a standalone solution; both are most effective when combined with dietary modification, increased physical activity, and behavioural support.
Frequently Asked Questions
Can I get Wegovy or Ozempic free on the NHS?
Ozempic may be available on NHS prescription for patients with type 2 diabetes meeting specific NICE criteria. Wegovy is available through specialist NHS weight management services for eligible patients with BMI ≥35 kg/m² and weight-related comorbidities, though access is currently limited due to supply constraints and local commissioning decisions.
Why does Wegovy cost more than Ozempic privately?
Wegovy typically costs more privately due to its higher maintenance dose (2.4 mg), specific formulation for weight management, market positioning, and higher demand. Private costs also reflect consultation fees, monitoring requirements, and pharmacy dispensing charges, which vary between providers.
How long do I need to take Wegovy or Ozempic to see results?
Most patients begin to see weight loss or improved glycaemic control within 8–12 weeks of reaching maintenance dose. However, both medications typically require long-term use for sustained benefit, with NICE guidance limiting NHS-funded Wegovy to a maximum of 2 years and continuation criteria requiring meaningful clinical response at 6 months.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript