A bubble or lump under the skin after an Ozempic injection is a common concern for patients using this GLP-1 receptor agonist for type 2 diabetes management. These localised reactions typically occur when semaglutide pools in the subcutaneous tissue rather than dispersing evenly, often due to suboptimal injection technique or inadequate site rotation. Whilst generally harmless and self-resolving, understanding why these bubbles form and how to prevent them can improve treatment comfort and medication absorption. This article explores the causes of injection site reactions, when to seek medical advice, and evidence-based techniques to minimise lumps and optimise your Ozempic administration.
Summary: A bubble under the skin after Ozempic injection is typically caused by medication pooling in subcutaneous tissue due to suboptimal injection technique, and usually resolves spontaneously within a few days.
- Ozempic (semaglutide) is a GLP-1 receptor agonist administered subcutaneously for type 2 diabetes management
- Bubbles form when medication is injected too superficially, the needle is withdrawn too quickly, or injection sites are not properly rotated
- Most lumps are benign and resolve as semaglutide is absorbed systemically over several days
- Seek medical attention if lumps persist beyond one week, become painful or infected, or are accompanied by systemic symptoms
- Prevention requires proper site rotation (spacing injections 1–2cm apart), holding the needle in place for at least six seconds after injection, and using correct 90-degree angle technique
- Report persistent side effects to your healthcare professional or via the MHRA Yellow Card Scheme
Table of Contents
What Causes a Bubble Under the Skin After Ozempic Injection?
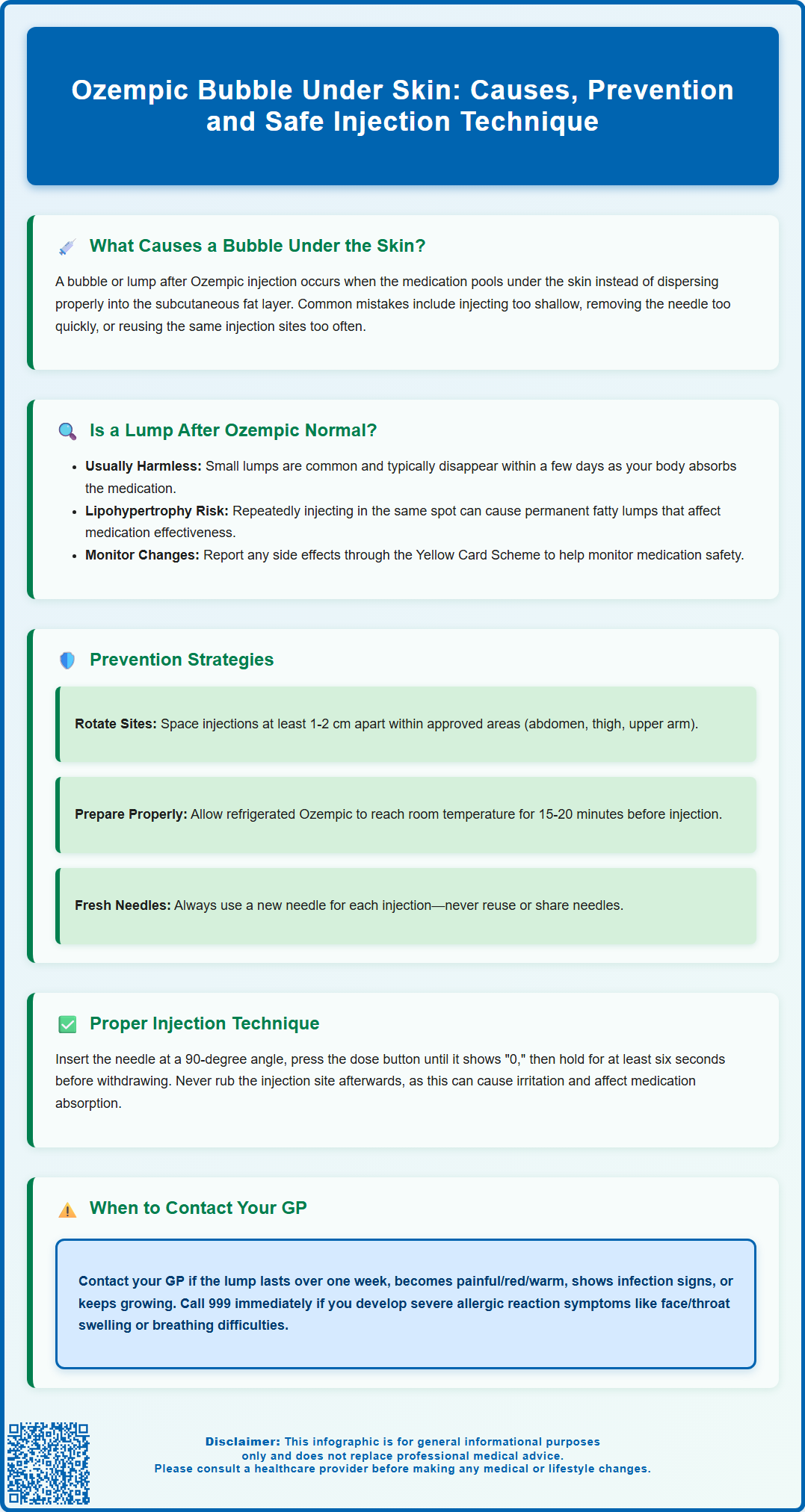
A bubble or lump under the skin following an Ozempic (semaglutide) injection is typically caused by the medication pooling in the subcutaneous tissue rather than dispersing properly. This occurs when the injection technique is suboptimal or when the needle is not correctly placed in the subcutaneous fat layer. Ozempic is formulated as a clear, colourless solution designed for subcutaneous administration, and when injected correctly, it should distribute evenly within the fatty tissue beneath the skin.
Several factors contribute to bubble formation at injection sites. Injecting too superficially into the dermis rather than the subcutaneous layer can cause visible swelling and discomfort. Not holding the needle in place long enough after pressing the dose button may result in medication leaking back along the needle track. Additionally, incomplete needle insertion can prevent proper delivery into the subcutaneous space.
The pharmacological properties of semaglutide itself may also play a role. As a glucagon-like peptide-1 (GLP-1) receptor agonist with a molecular weight of approximately 4,113 daltons, semaglutide requires time to be absorbed from the injection site into systemic circulation. When the medication accumulates in one area, it creates a temporary depot that manifests as a palpable lump or visible bubble.
Other contributing factors include:
-
Injecting into areas with insufficient subcutaneous fat
-
Reusing injection sites too frequently, leading to tissue changes
-
Not using the correct injection technique for your body type
-
Withdrawing the needle too quickly after injection
Whilst these bubbles are generally harmless and resolve spontaneously, understanding their cause helps patients optimise their injection technique and minimise discomfort.
Is a Lump or Bubble After Ozempic Normal?
Experiencing a small lump or bubble after administering Ozempic is relatively common, particularly when patients are new to self-injection or adjusting their technique. According to the electronic Medicines Compendium (emc), injection site reactions are listed as potential side effects of Ozempic, though they are generally uncommon.
These localised reactions are considered normal and benign when they present as small, painless swellings that gradually diminish. The lump represents medication that has not yet been fully absorbed into the bloodstream and typically indicates that the injection was delivered into the subcutaneous tissue, albeit with suboptimal dispersion. Most patients notice the bubble decreasing in size as the semaglutide is absorbed systemically, usually settling within a few days.
However, certain characteristics warrant closer attention. You should contact your GP or diabetes team if:
-
The lump persists for more than one week
-
The area becomes increasingly painful, red, or warm to touch
-
You develop signs of infection (fever, spreading redness, discharge)
-
The lump continues to grow rather than resolve
-
You experience systemic symptoms such as dizziness or difficulty breathing
Call 999 or go to A&E immediately if you develop signs of a severe allergic reaction such as swelling of the face, lips, tongue or throat, breathing difficulties, or a fast heartbeat.
For urgent concerns that aren't emergencies, contact NHS 111 for advice.
It is important to distinguish between a simple medication depot and more serious complications such as lipohypertrophy (fatty lumps from repeated injections in the same site) or injection site abscesses. Lipohypertrophy develops over time with poor site rotation and appears as firm, rubbery areas that can affect medication absorption. True infections are rare but require prompt medical assessment.
If you experience any side effects, talk to your healthcare professional. You can also report side effects directly via the Yellow Card Scheme at https://yellowcard.mhra.gov.uk/
How to Prevent Injection Site Reactions with Ozempic
Preventing bubbles and lumps after Ozempic injections requires a systematic approach to injection site selection, preparation, and rotation. The most critical preventive measure is proper site rotation, which means rotating within and between injection areas (abdomen, thigh, and upper arm), spacing injections at least 1-2 cm apart. Ozempic should be administered subcutaneously, and patients should maintain a rotation schedule to allow tissue recovery and avoid injecting into areas with lipohypertrophy.
When selecting an injection site, choose areas with adequate subcutaneous fat. The abdomen (excluding a 5cm radius around the navel) is often preferred as it typically has consistent fat distribution and allows for easy access. The anterior and lateral thigh provides a large surface area for rotation, whilst the upper outer arm may be used, though this site can be more challenging for self-injection and may require assistance from another person. Avoid injecting into areas with scars, bruises, or existing lumps, as altered tissue architecture can impair medication absorption.
Key preparation steps include:
-
If the pen has been refrigerated, allowing the Ozempic pen to reach room temperature (about 15–20 minutes out of the refrigerator) before injection may reduce discomfort
-
Cleaning the injection site with an alcohol wipe and allowing it to dry completely
-
Inspecting the medication for particles or discolouration before each use
-
Performing a flow check with a new pen as directed in the patient information leaflet
-
Always using a new needle for each injection – never reuse needles
-
Never sharing your pen with anyone else, even if the needle is changed
Patients should also consider their injection timing and environment. Administering Ozempic when relaxed and unhurried reduces the likelihood of technical errors. Some patients find it helpful to mark injection sites on a body diagram to track their rotation pattern systematically.
After use, dispose of used needles safely in an NHS-provided sharps bin. Your GP practice, pharmacy, or local council can provide information on obtaining and disposing of sharps bins in your area.
Proper Ozempic Injection Technique to Avoid Lumps
Mastering the correct injection technique is fundamental to preventing bubbles and ensuring optimal medication absorption. The process begins with thorough hand hygiene—wash hands with soap and water for at least 20 seconds before handling the Ozempic pen. Gather all necessary supplies: the pen, a new needle, alcohol wipes, and a sharps container for safe needle disposal.
Once the injection site is selected and cleaned, consider whether you need to create a skin fold. Using your thumb and forefinger, gently pinch approximately 2–3cm of skin to lift the subcutaneous tissue away from underlying muscle. This technique is particularly important for very lean individuals. For most adults using a 4mm needle (the standard recommendation), a skin fold may not be necessary unless advised by your healthcare professional.
The injection sequence should follow these steps:
- Insert the needle at a 90-degree angle with a swift, confident motion (a 45-degree angle may be appropriate if specifically advised by your healthcare professional)
- If using a skin fold, maintain it gently throughout the injection
- Press and hold the dose button until the dose counter shows "0"
- Continue holding the button and count to at least six before withdrawing the needle—this crucial pause allows the full dose to be delivered and prevents medication leakage
- Withdraw the needle straight out at the same angle it was inserted
- If using a skin fold, release it after withdrawing the needle
- Do not rub the injection site afterwards, as this can cause irritation and affect absorption
A common mistake leading to bubble formation is withdrawing the needle too quickly after injection. The six-second hold time (as specified in the Ozempic patient information leaflet) is essential for allowing the medication to begin dispersing within the subcutaneous tissue. Premature withdrawal can result in medication leaking back through the needle track, creating a visible bubble or reducing the delivered dose.
Patients should use the appropriate needle length. For most adults, a 4mm needle is suitable regardless of body mass index, as recommended by the Forum for Injection Technique (FIT UK). These shorter needles reduce the risk of intramuscular injection while ensuring adequate subcutaneous delivery.
If you consistently experience bubbles despite following proper technique, request a practical demonstration from your practice nurse or diabetes educator. They can observe your technique, identify specific areas for improvement, and provide hands-on coaching. Many NHS diabetes services offer structured education programmes that include injection technique training as a core component.
Remember to report any persistent side effects to your healthcare professional or via the Yellow Card Scheme at https://yellowcard.mhra.gov.uk/
Frequently Asked Questions
How long does a bubble under the skin last after Ozempic injection?
Most bubbles or lumps after Ozempic injection resolve spontaneously within a few days as the semaglutide is absorbed into systemic circulation. If a lump persists for more than one week or becomes increasingly painful, contact your GP or diabetes team for assessment.
Should I be worried about a lump after my Ozempic injection?
Small, painless lumps that gradually diminish are generally normal and benign. However, seek medical advice if the area becomes red, warm, increasingly painful, shows signs of infection, or if you develop systemic symptoms such as fever or difficulty breathing.
How can I prevent bubbles forming after Ozempic injections?
Prevent bubbles by rotating injection sites properly (spacing injections at least 1–2cm apart), holding the needle in place for at least six seconds after pressing the dose button, inserting the needle at a 90-degree angle into subcutaneous fat, and avoiding rubbing the injection site afterwards.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript