Ozempic (semaglutide) is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes management, administered as a once-weekly injection to improve glycaemic control. Concerns about Ozempic and blood clots occasionally arise among patients, prompting questions about thrombotic risk. Currently, no established causal link exists between semaglutide and increased venous or arterial thromboembolism according to MHRA and EMA guidance. This article examines the evidence surrounding Ozempic and blood clots, explores individual risk factors, and provides essential safety guidance for patients taking this medication.
Summary: There is no established causal link between Ozempic (semaglutide) and increased risk of blood clots according to current UK regulatory guidance from the MHRA and EMA.
- Ozempic is a GLP-1 receptor agonist licensed for type 2 diabetes, not listed as causing thromboembolism in product information.
- Clinical trials including SUSTAIN-6 showed cardiovascular benefits rather than increased thrombotic events compared to placebo.
- Type 2 diabetes itself increases blood clot risk through endothelial damage, platelet reactivity, and altered coagulation independent of medication.
- Patients should seek immediate medical attention (999) for symptoms of pulmonary embolism, stroke, or myocardial infarction regardless of medication use.
- Never discontinue Ozempic without medical guidance, as stopping diabetes treatment may worsen glycaemic control and increase cardiovascular risk.
- Report any suspected adverse reactions through the MHRA Yellow Card Scheme to support ongoing medication safety surveillance.
Table of Contents
Understanding Ozempic: What It Is and How It Works
Ozempic is the brand name for semaglutide, a glucagon-like peptide-1 (GLP-1) receptor agonist that has a UK marketing authorisation for the treatment of type 2 diabetes mellitus. It is licensed as an adjunct to diet and exercise to improve glycaemic control in adults, either as monotherapy when metformin is inappropriate or contraindicated, or in combination with other diabetes medications. Semaglutide is administered as a once-weekly subcutaneous injection with stepwise dose escalation, offering convenience compared to daily diabetes medications.
The mechanism of action centres on mimicking the naturally occurring hormone GLP-1, which plays several crucial roles in glucose regulation. When semaglutide binds to GLP-1 receptors in the pancreas, it stimulates insulin secretion in a glucose-dependent manner, meaning insulin release occurs primarily when blood glucose levels are elevated. This reduces the risk of hypoglycaemia compared to some other diabetes treatments. Simultaneously, the medication suppresses glucagon secretion, a hormone that raises blood glucose levels, thereby contributing to better overall glycaemic control.
Beyond its effects on insulin and glucagon, Ozempic slows gastric emptying, which helps reduce post-meal glucose spikes and promotes satiety. Many patients experience weight loss as a secondary benefit, although it's important to note that Ozempic is not licensed for weight management in the UK (a higher dose formulation called Wegovy is specifically licensed for weight management). The National Institute for Health and Care Excellence (NICE) recognises semaglutide as an effective option within its type 2 diabetes treatment pathways (NG28), particularly for patients who require additional glycaemic control or who may benefit from weight reduction. Understanding how Ozempic works provides essential context when considering any potential adverse effects, including concerns about thrombotic events.
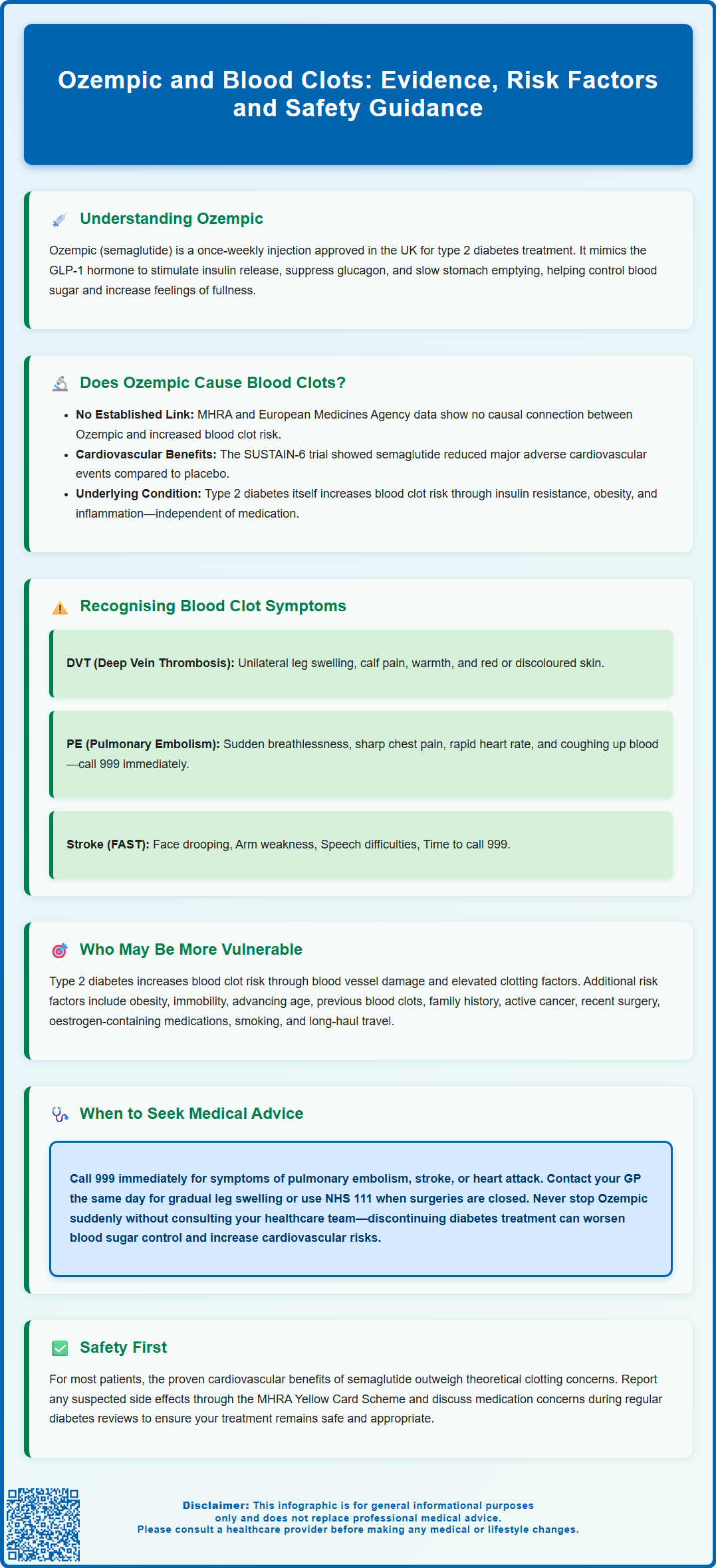
Does Ozempic Cause Blood Clots? Examining the Evidence
The question of whether Ozempic directly causes blood clots requires careful examination of available clinical evidence and pharmacovigilance data. Currently, there is no established causal link between semaglutide and an increased risk of venous or arterial thromboembolism in the licensed product information approved by the MHRA or the European Medicines Agency (EMA). Blood clots, including deep vein thrombosis and pulmonary embolism, are not listed among the common or uncommon adverse reactions in the Summary of Product Characteristics for Ozempic.
Extensive clinical trials conducted during the drug's development, including the SUSTAIN programme, involved thousands of patients with type 2 diabetes followed over several years. While most SUSTAIN trials focused on glycaemic control and weight changes, the SUSTAIN-6 cardiovascular outcomes trial specifically evaluated cardiovascular safety. This study, published in the New England Journal of Medicine (2016), showed that semaglutide reduced the risk of major adverse cardiovascular events compared to placebo, suggesting potential cardiovascular benefits rather than harm. Thrombotic events were monitored throughout the clinical programme and did not demonstrate a significant increase compared to placebo or active comparators.
However, it is important to acknowledge that patients with type 2 diabetes inherently carry elevated thrombotic risk due to the prothrombotic state associated with insulin resistance, obesity, inflammation, and endothelial dysfunction. Any thrombotic events occurring in patients taking Ozempic may reflect underlying diabetes-related risk rather than a drug effect. Post-marketing surveillance continues to monitor for rare or unexpected adverse effects, and healthcare professionals are encouraged to report any suspected reactions through the MHRA Yellow Card Scheme. Patients concerned about blood clots should discuss their individual risk profile with their GP or diabetes specialist rather than discontinuing treatment without medical guidance.
Recognising Blood Clot Symptoms While Taking Ozempic
Regardless of medication use, all patients should be aware of the signs and symptoms of blood clots, as prompt recognition enables timely medical intervention. Deep vein thrombosis (DVT) typically presents with unilateral leg swelling, pain or tenderness (often in the calf), warmth over the affected area, and visible changes in skin colour, which may appear red or discoloured. The discomfort often worsens when walking or standing and superficial veins may become more visible in some cases. It is worth noting that DVT can occasionally occur without obvious symptoms, making vigilance important for those with risk factors.
Pulmonary embolism (PE), which occurs when a blood clot travels to the lungs, constitutes a medical emergency requiring immediate attention. Characteristic symptoms include sudden-onset breathlessness or difficulty breathing, sharp chest pain that may worsen with deep breathing or coughing, rapid heart rate, light-headedness or fainting, and coughing up blood (haemoptysis). Some patients may experience a sense of anxiety or feeling that something is seriously wrong. The presentation can vary considerably, with some individuals experiencing subtle symptoms whilst others develop dramatic, life-threatening manifestations.
Arterial thrombosis presents differently depending on the affected vessel. Symptoms of stroke include sudden facial drooping, arm weakness, and speech difficulties (remember the FAST acronym used in NHS campaigns: Face, Arms, Speech, Time to call 999). Myocardial infarction typically causes central chest pain, often radiating to the jaw or left arm, accompanied by sweating, nausea, and breathlessness. Peripheral arterial thrombosis may cause sudden limb pain, pallor, coldness, and absent pulses. Anyone experiencing these symptoms should seek immediate medical assessment, as early treatment significantly improves outcomes. It is essential to emphasise that these symptoms warrant urgent evaluation regardless of current medications, as blood clots can occur in any individual.
Risk Factors and Who May Be More Vulnerable
Understanding individual risk factors for thromboembolism helps patients and clinicians make informed decisions about diabetes management and monitoring. Type 2 diabetes itself confers increased thrombotic risk through multiple mechanisms, including hyperglycaemia-induced endothelial damage, increased platelet reactivity, elevated coagulation factors, and reduced fibrinolysis. Patients with poorly controlled diabetes face higher risk than those achieving target HbA1c levels, emphasising the importance of optimal glycaemic management.
Obesity, commonly present in individuals with type 2 diabetes, independently increases venous thromboembolism risk through mechanical factors, chronic inflammation, and altered coagulation profiles. Immobility or prolonged sedentary behaviour further compounds this risk, as does advancing age. Previous history of blood clots represents one of the strongest predictors of future thrombotic events, and such patients typically require careful assessment before starting any new medication. Family history of thrombophilia or known inherited clotting disorders also elevates baseline risk.
Additional factors warranting consideration include active malignancy, recent surgery or trauma, use of oestrogen-containing contraceptives or hormone replacement therapy, smoking, and certain inflammatory conditions such as inflammatory bowel disease. For long-haul travel, general preventive measures include staying mobile, maintaining hydration, and wearing compression stockings; pharmacological thromboprophylaxis is reserved only for very high-risk individuals after clinical assessment. It's important to note that semaglutide is not recommended during pregnancy or breastfeeding, and women of childbearing potential should use effective contraception. The medication should be discontinued at least two months before a planned pregnancy, as stated in the product information.
Clinicians should conduct individualised risk assessments, considering the benefits of improved glycaemic control against any theoretical concerns. For most patients, the cardiovascular benefits demonstrated in clinical trials likely outweigh unsubstantiated thrombotic concerns. Those with significant risk factors should receive appropriate education about symptoms and may require more frequent monitoring, though this reflects good diabetes care rather than specific Ozempic-related precautions.
When to Seek Medical Advice: Safety Guidance for Patients
Patients taking Ozempic should understand when to contact healthcare services and how urgently different situations require attention. Any symptoms suggestive of blood clots, as described previously, warrant immediate medical assessment. For suspected pulmonary embolism, stroke, or myocardial infarction, patients should call 999 or attend the nearest Emergency Department without delay. These conditions require urgent investigation and treatment to prevent serious complications or death. Time-critical interventions, such as thrombolysis for stroke or anticoagulation for PE, significantly improve outcomes when administered promptly.
For less acute concerns, such as unilateral leg swelling developing over hours to days without severe pain or breathing difficulties, patients should contact their GP practice on the same day for assessment. Many surgeries offer urgent appointments or telephone triage to evaluate symptoms and determine appropriate next steps. NHS 111 provides an alternative route for advice when GP surgeries are closed, helping patients navigate whether symptoms require emergency attention or can wait for routine review.
Beyond thrombotic concerns, patients should be aware of other important Ozempic side effects that may require medical input. Gastrointestinal symptoms including nausea, vomiting, diarrhoea, and abdominal pain affect many users, particularly during dose escalation. Persistent vomiting leading to dehydration or inability to maintain adequate fluid intake requires medical review. Signs of pancreatitis, including severe persistent abdominal pain radiating to the back, necessitate urgent assessment. Symptoms of gallbladder disease (severe right upper quadrant pain, fever, jaundice) also warrant prompt medical attention. Patients with pre-existing diabetic retinopathy should attend regular eye screening as rapid improvement in glucose control may temporarily worsen retinopathy. Hypoglycaemia, though uncommon with Ozempic monotherapy, becomes more likely when combined with insulin or sulfonylureas.
Patients should never discontinue Ozempic abruptly due to unsubstantiated concerns about blood clots without consulting their diabetes team. Stopping effective diabetes treatment may lead to deteriorating glycaemic control, which itself increases cardiovascular and thrombotic risk. Any concerns about medication safety should be discussed with a GP, diabetes specialist nurse, or consultant, who can provide evidence-based guidance tailored to individual circumstances. The MHRA Yellow Card Scheme allows patients to report suspected side effects directly, contributing to ongoing medication safety surveillance. Regular diabetes reviews provide opportunities to discuss any concerns and ensure treatment remains appropriate and well-tolerated.
Frequently Asked Questions
Can Ozempic increase my risk of developing blood clots?
Currently, there is no established causal link between Ozempic and increased blood clot risk according to MHRA and EMA guidance. Clinical trials including cardiovascular outcomes studies have not demonstrated increased thrombotic events compared to placebo.
What symptoms should I watch for that might indicate a blood clot?
Deep vein thrombosis symptoms include unilateral leg swelling, pain, warmth, and skin discolouration. Pulmonary embolism presents with sudden breathlessness, sharp chest pain, rapid heart rate, and potentially coughing blood, requiring immediate emergency assessment by calling 999.
Should I stop taking Ozempic if I'm worried about blood clots?
Never discontinue Ozempic without consulting your GP or diabetes specialist, as stopping effective diabetes treatment may worsen glycaemic control and actually increase cardiovascular risk. Discuss any concerns with your healthcare team for evidence-based guidance tailored to your individual circumstances.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript