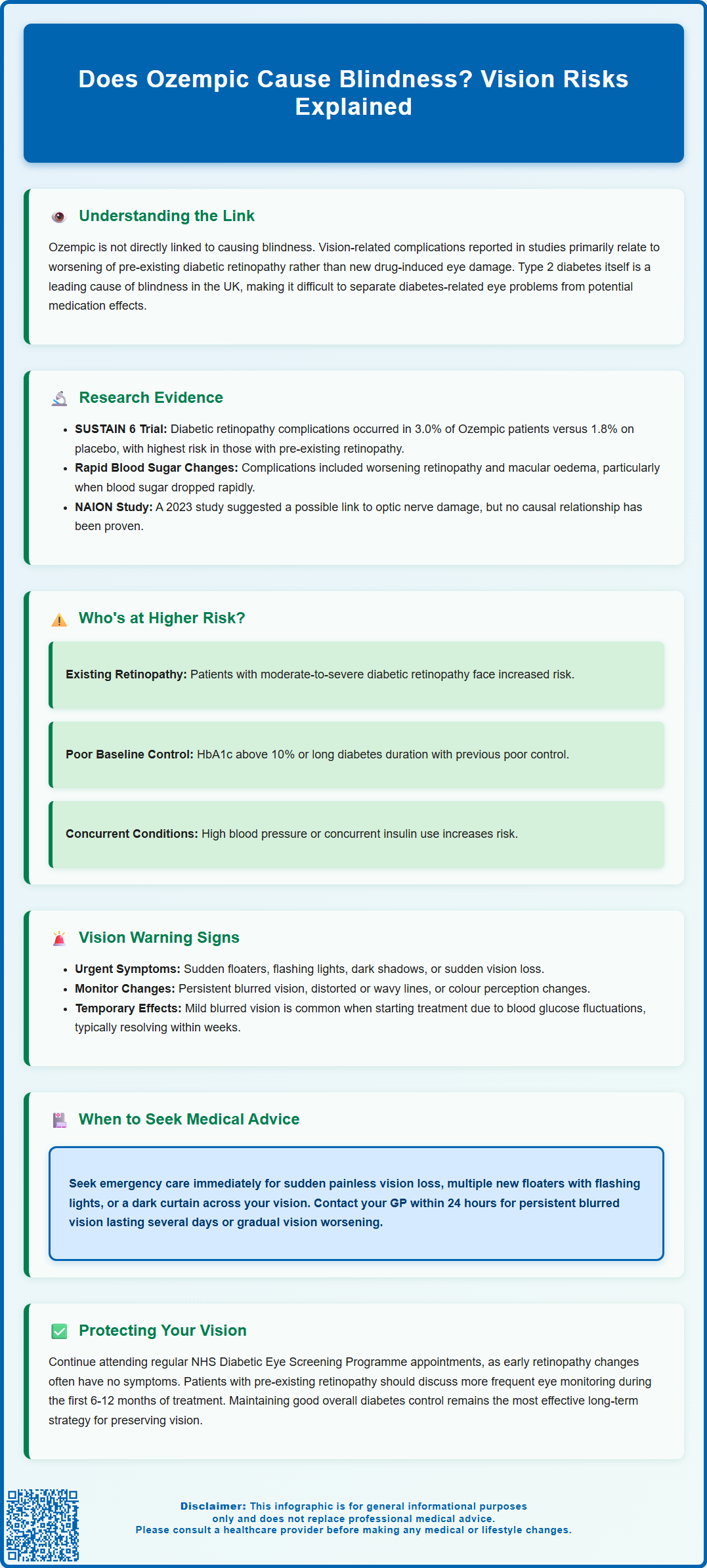
Does Ozempic cause blindness? This question has generated significant concern among patients prescribed semaglutide for type 2 diabetes. While there is no established direct causal link between Ozempic and blindness, clinical trials have identified an increased risk of diabetic retinopathy complications, particularly in patients with pre-existing eye disease. Understanding the relationship between this GLP-1 receptor agonist and vision health requires careful consideration of diabetes-related eye complications, the effects of rapid glycaemic improvement, and appropriate monitoring strategies. This article examines the current evidence, risk factors, and guidance for UK patients and healthcare professionals.
Summary: Ozempic does not directly cause blindness, but clinical trials show it may increase diabetic retinopathy complications in patients with pre-existing eye disease.
- Semaglutide is a GLP-1 receptor agonist licensed in the UK for type 2 diabetes treatment, administered as a once-weekly subcutaneous injection.
- SUSTAIN 6 trial found retinopathy complications in 3.0% of semaglutide patients versus 1.8% on placebo, particularly in those with pre-existing retinopathy.
- Rapid HbA1c reduction may trigger early worsening phenomenon, temporarily affecting retinal blood flow and growth factor expression in compromised tissue.
- The UK Summary of Product Characteristics warns about diabetic retinopathy complications, especially in patients with existing retinopathy or using insulin.
- Patients should report persistent blurred vision, sudden floaters, flashing lights, or vision loss immediately to healthcare professionals or eye casualty services.
- Regular NHS Diabetic Eye Screening Programme attendance remains essential, with more frequent monitoring recommended for high-risk patients during treatment initiation.
Table of Contents
Understanding Ozempic and Vision-Related Concerns
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Administered as a once-weekly subcutaneous injection, it works by enhancing insulin secretion in response to elevated blood glucose levels, suppressing glucagon release, and slowing gastric emptying. These mechanisms collectively improve glycaemic control and often result in weight reduction as a secondary effect, though it's important to note that Ozempic is not licensed for weight management in the UK.
Recent media attention and patient concerns have focused on whether Ozempic might cause blindness or serious vision problems. It is important to clarify that there is no established direct causal link between semaglutide and blindness. However, like all medications, Ozempic has a recognised adverse effect profile, and vision-related complications have been reported in clinical studies and post-marketing surveillance. These reports primarily relate to diabetic retinopathy complications rather than a novel drug-induced mechanism causing blindness.
The UK Summary of Product Characteristics (SmPC) for Ozempic contains a specific warning (section 4.4) about diabetic retinopathy complications, particularly in patients with pre-existing diabetic retinopathy and when co-administered with insulin. The SmPC advises appropriate monitoring in these higher-risk patients.
The relationship between Ozempic and eye health is complex and must be understood within the broader context of diabetes management. Type 2 diabetes itself is a leading cause of visual impairment and blindness in the UK, predominantly through diabetic retinopathy, diabetic macular oedema, and increased risk of cataracts and glaucoma. When evaluating vision concerns in patients taking Ozempic, clinicians must distinguish between pre-existing diabetic eye disease, the natural progression of retinopathy, and potential medication-related effects. This article examines the current evidence, explores the mechanisms involved, and provides guidance on monitoring and managing vision-related concerns in patients prescribed this medication.
Research Evidence: Ozempic and Eye Complications
The primary evidence regarding Ozempic and vision complications comes from the SUSTAIN clinical trial programme, particularly SUSTAIN 6, a cardiovascular outcomes trial published in the New England Journal of Medicine in 2016. This study identified a statistically significant increase in diabetic retinopathy complications among patients treated with semaglutide compared to placebo. Specifically, retinopathy complications occurred in 3.0% of semaglutide-treated patients versus 1.8% in the placebo group, representing a hazard ratio of 1.76 (95% CI, 1.11 to 2.78).
These complications included progression of existing retinopathy, development of proliferative retinopathy, macular oedema requiring treatment (including laser photocoagulation or intravitreal injections), and in some cases, vitreous haemorrhage. Importantly, the increased risk was most pronounced in patients with pre-existing diabetic retinopathy at baseline and those who experienced rapid improvements in glycaemic control. The magnitude and speed of HbA1c reduction appeared to correlate with retinopathy worsening, a phenomenon previously documented with intensive insulin therapy.
Subsequent real-world studies and post-marketing surveillance have provided additional data. A 2023 observational study published in JAMA Ophthalmology suggested a possible association between GLP-1 receptor agonists and non-arteritic anterior ischaemic optic neuropathy (NAION), though this remains under investigation and no definitive causal relationship has been established. As of the time of writing, the MHRA has not issued any specific safety communications regarding NAION and semaglutide, though they continue to monitor safety signals related to GLP-1 agonists as part of routine pharmacovigilance.
The European Medicines Agency's European Public Assessment Report (EPAR) for Ozempic acknowledges the retinopathy findings and supports the warnings in the SmPC. For most patients, according to NICE guidance (NG28), the benefits of improved glycaemic control with Ozempic may outweigh the potential risks, particularly in those with established cardiovascular disease. However, these findings underscore the importance of individualised risk assessment, particularly in patients with established diabetic eye disease, and the need for appropriate ophthalmological monitoring during treatment initiation and dose escalation.
Diabetic Retinopathy and GLP-1 Receptor Agonists
Diabetic retinopathy develops as a microvascular complication of prolonged hyperglycaemia, affecting the blood vessels of the retina. It progresses through stages from mild non-proliferative changes to proliferative diabetic retinopathy, where abnormal new blood vessels form, potentially leading to vitreous haemorrhage, retinal detachment, and vision loss. Diabetic macular oedema, characterised by fluid accumulation in the macula, can occur at any stage and significantly impairs central vision.
The mechanism by which rapid glycaemic improvement might worsen retinopathy is not fully understood but is thought to relate to early worsening phenomenon. When blood glucose levels drop quickly, there may be temporary alterations in retinal blood flow, changes in growth factor expression (particularly vascular endothelial growth factor), and metabolic stress on already compromised retinal tissue. This phenomenon was first documented in the Diabetes Control and Complications Trial (DCCT) with intensive insulin therapy and appears to be a class effect related to the rate of HbA1c reduction rather than a specific property of semaglutide.
Patients at highest risk include those with:
-
Moderate to severe non-proliferative or proliferative diabetic retinopathy at baseline
-
Poor baseline glycaemic control (HbA1c >10%) with anticipated rapid improvement
-
Long duration of diabetes with suboptimal previous control
-
Concurrent hypertension or other microvascular complications
-
Concomitant insulin therapy, as specifically noted in the Ozempic SmPC
The NHS Diabetic Eye Screening Programme provides screening at risk-based intervals (typically 1-2 yearly) for all patients with diabetes. For those commencing GLP-1 receptor agonists with known retinopathy, more frequent ophthalmological review may be warranted, particularly during the first year of treatment when glycaemic changes are most pronounced. Close ophthalmic monitoring during periods of rapid HbA1c change is important, as noted in NICE guidance (NG28) and the Ozempic SmPC, though this must be balanced against the benefits of improved glucose control.
Recognising Vision Changes While Taking Ozempic
Patients taking Ozempic should be educated about potential vision changes and encouraged to report any new or worsening symptoms promptly. While serious complications are uncommon, early detection and intervention can prevent progression to sight-threatening disease.
Symptoms that warrant attention include:
-
Blurred vision that persists beyond a few days or progressively worsens
-
Floaters (dark spots or strings drifting through the visual field), particularly if sudden in onset or increasing in number
-
Flashing lights or photopsia, which may indicate retinal traction or detachment
-
Dark curtain or shadow encroaching on peripheral or central vision
-
Distorted vision where straight lines appear wavy (metamorphopsia)
-
Difficulty with colour perception or reduced contrast sensitivity
-
Sudden vision loss in one or both eyes, which constitutes a medical emergency
It is important to note that mild, transient blurred vision is relatively common when starting diabetes medications or when blood glucose levels fluctuate. Changes in blood glucose can temporarily alter the refractive properties of the lens, causing vision to seem unclear. This typically resolves within a few weeks as glucose levels stabilise and does not indicate serious pathology. However, persistent or progressive symptoms require professional assessment.
Patients should maintain a record of any vision changes, noting their onset, duration, and relationship to medication initiation or dose increases. This information is valuable for healthcare professionals in determining whether symptoms represent benign, transient effects or require urgent ophthalmological referral. Regular attendance at NHS Diabetic Eye Screening Programme appointments remains essential, as many retinopathy changes are asymptomatic in early stages and only detectable through fundoscopy or retinal photography. For urgent eye symptoms, patients can contact NHS 111, their local eye casualty department, or in some areas, optometrists providing Minor Eye Conditions Services (MECS).
When to Seek Medical Advice About Your Eyesight
Understanding when vision changes require urgent attention versus routine review is crucial for patient safety. The following guidance helps patients and healthcare professionals determine appropriate action.
Seek immediate medical attention (attend A&E, eye casualty, or call 999/NHS 111) if you experience:
-
Sudden, painless vision loss in one or both eyes
-
Sudden onset of multiple new floaters, especially with flashing lights
-
A dark curtain or shadow moving across your field of vision
-
Severe eye pain accompanied by vision changes, nausea, or headache (possible acute angle-closure glaucoma)
These symptoms may indicate serious conditions such as retinal detachment, vitreous haemorrhage, or retinal artery occlusion, which require emergency ophthalmological assessment.
Contact your GP, diabetes care team, or seek same-day optometrist assessment within 24 hours if you notice:
-
Persistent blurred vision lasting more than a few days
-
Gradual worsening of vision not explained by refractive changes
-
New distortion of straight lines or difficulty reading
-
Increasing difficulty with night vision or glare sensitivity
In many areas, optometrists provide urgent eye care through Minor Eye Conditions Services (MECS) or Community Eyecare Services (CES), which may offer faster access than GP appointments.
Arrange routine review if:
-
You experience mild, intermittent blurred vision during the first few weeks of treatment
-
You have missed your scheduled diabetic eye screening appointment
-
You have known diabetic retinopathy and are starting or increasing Ozempic dosage
For patients with pre-existing retinopathy, discuss with your diabetes specialist whether more frequent ophthalmological monitoring is appropriate during the first 6-12 months of GLP-1 therapy, particularly if you are also using insulin. Remember that maintaining good overall diabetes control, including blood pressure and lipid management, alongside attending your invited eye screening appointments, remains the most effective strategy for preserving vision long-term. The benefits of improved glycaemic control with Ozempic should be assessed on an individual basis, in line with NICE guidance, taking into account your personal risk factors and existing eye health.
Scientific References
- Ozempic 0.5 mg solution for injection in pre-filled pen - Summary of Product Characteristics (SmPC).
- Ozempic - European Public Assessment Report (EPAR).
- Type 2 diabetes in adults: management. NICE guideline [NG28].
- Semaglutide and Cardiovascular Outcomes in Patients with Type 2 Diabetes (SUSTAIN-6).
- Diabetic eye screening programme: standards.
- Clinical Predictors of Diabetic Retinopathy Progression; A Systematic Review.
Frequently Asked Questions
Can Ozempic directly cause blindness?
No, there is no established direct causal link between Ozempic and blindness. However, clinical trials have shown an increased risk of diabetic retinopathy complications, particularly in patients with pre-existing eye disease or when experiencing rapid improvements in blood glucose control.
What vision symptoms should I report while taking Ozempic?
Report persistent blurred vision lasting more than a few days, sudden onset of floaters, flashing lights, dark shadows across your vision, or any sudden vision loss immediately. Mild, transient blurred vision during the first few weeks is common and typically resolves as glucose levels stabilise.
Who is at highest risk for eye complications with Ozempic?
Patients at highest risk include those with moderate to severe diabetic retinopathy at baseline, poor glycaemic control (HbA1c >10%), long diabetes duration with suboptimal control, concurrent insulin therapy, or other microvascular complications. These patients may require more frequent ophthalmological monitoring during treatment.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript