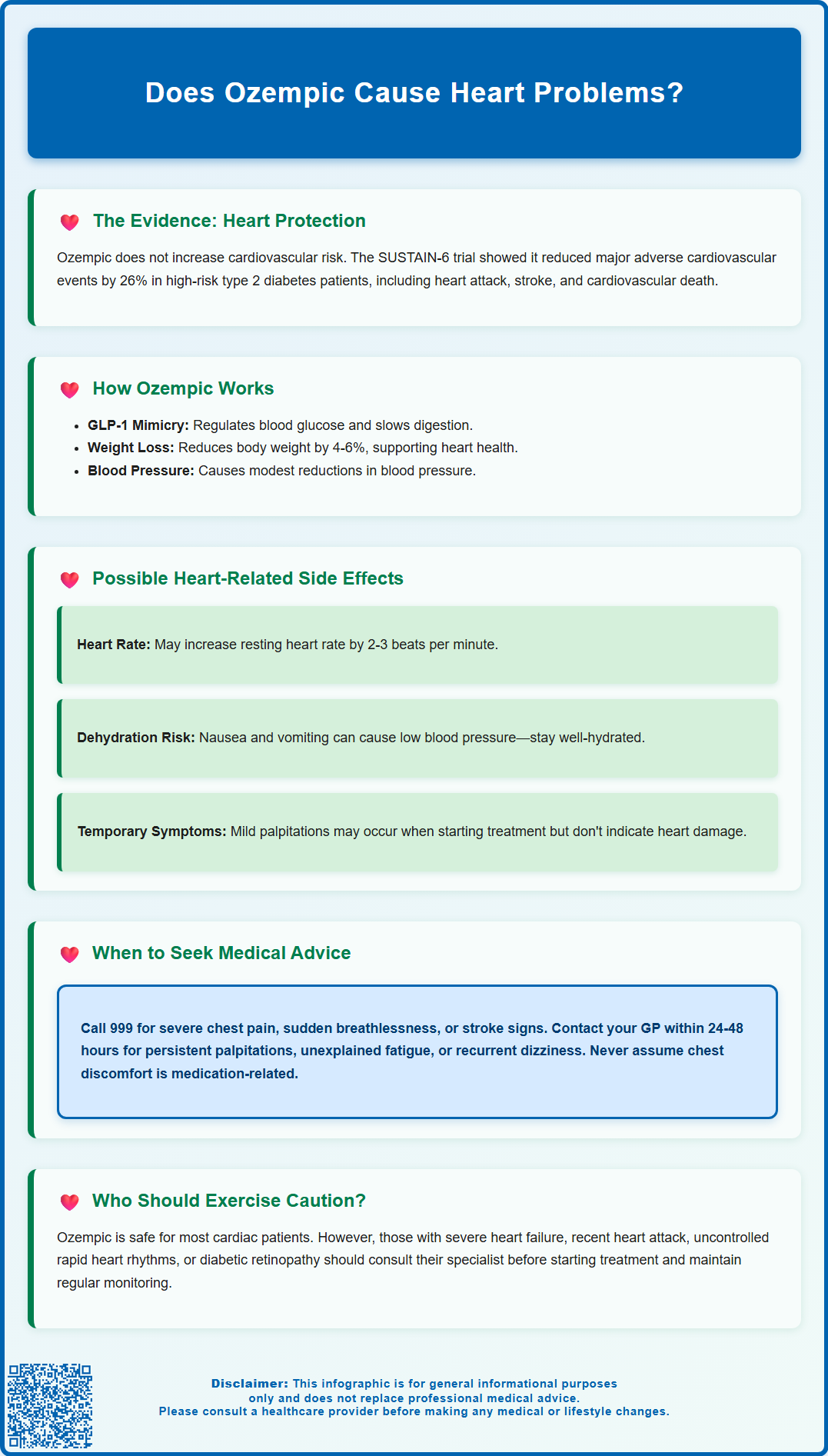
Does Ozempic cause heart problems? This is a common concern for patients prescribed semaglutide for type 2 diabetes management. Clinical evidence from large-scale trials, including SUSTAIN-6, demonstrates that Ozempic does not increase cardiovascular risk and may offer protective benefits for certain high-risk patients. This GLP-1 receptor agonist has been associated with reduced major adverse cardiovascular events in people with type 2 diabetes and established cardiovascular risk factors. Understanding the cardiovascular profile of Ozempic, including potential benefits, monitoring requirements, and when to seek medical advice, is essential for safe and effective treatment. This article examines the evidence surrounding Ozempic and heart health, providing guidance for patients and healthcare professionals.
Summary: Ozempic (semaglutide) does not cause heart problems and clinical trials demonstrate it may reduce cardiovascular risk in patients with type 2 diabetes.
- Semaglutide is a GLP-1 receptor agonist that regulates blood glucose, slows gastric emptying, and reduces appetite.
- The SUSTAIN-6 trial showed a 26% reduction in major adverse cardiovascular events in high-risk patients with type 2 diabetes.
- Ozempic may cause a modest increase in resting heart rate of approximately 2-3 beats per minute.
- Patients should monitor for heart-related symptoms including persistent palpitations, chest discomfort, or breathlessness and report these to their healthcare provider.
- The MHRA has approved Ozempic for glycaemic control in adults with type 2 diabetes, though it is not specifically licensed for cardiovascular risk reduction.
- Patients with severe heart failure, recent myocardial infarction, or uncontrolled tachyarrhythmias require careful assessment before starting treatment.
Table of Contents
Does Ozempic Cause Heart Problems?
Ozempic (semaglutide) has not been shown to increase cardiovascular risk in clinical studies. Research demonstrates that this glucagon-like peptide-1 (GLP-1) receptor agonist may offer cardiovascular benefits for certain patients. The SUSTAIN-6 trial, which included over 3,000 participants with type 2 diabetes at high cardiovascular risk, showed that Ozempic reduced the risk of major adverse cardiovascular events compared to placebo.
The medication works by mimicking the natural hormone GLP-1, which regulates blood glucose levels, slows gastric emptying, and reduces appetite. Beyond its glucose-lowering effects, semaglutide has been associated with modest improvements in several cardiovascular risk factors, including modest blood pressure reduction and weight loss. These effects may contribute to cardiovascular outcomes.
It is important to distinguish between causing heart problems and experiencing heart-related symptoms during treatment. Some patients may notice changes in heart rate or experience palpitations, particularly when starting Ozempic or during dose escalation. These symptoms are typically mild and transient.
In the UK, the Medicines and Healthcare products Regulatory Agency (MHRA) has approved Ozempic for improving glycaemic control in adults with type 2 diabetes. It is not specifically licensed for cardiovascular risk reduction. According to NICE guidance, SGLT2 inhibitors are generally prioritised for patients with established cardiovascular disease, while GLP-1 receptor agonists like semaglutide are recommended based on glycaemic control and weight management criteria.
Cardiovascular Benefits and Risks of Ozempic
The cardiovascular effects of Ozempic have been studied in clinical trials. The SUSTAIN-6 study demonstrated a 26% reduction in major adverse cardiovascular events (MACE), which includes cardiovascular death, non-fatal myocardial infarction, and non-fatal stroke in high-risk patients with type 2 diabetes.
Several factors may contribute to these cardiovascular outcomes. Weight reduction achieved through Ozempic treatment—typically around 4-6% of body weight at doses used for type 2 diabetes—may help reduce cardiovascular burden. The medication also produces modest reductions in systolic blood pressure, which may contribute to cardiovascular effects. Other potential mechanisms have been proposed, though their clinical significance remains under investigation.
Despite these benefits, clinicians should be aware of specific considerations. There is no evidence that Ozempic increases the risk of heart failure, arrhythmias, or myocardial infarction in the general population. However, the medication can cause a modest increase in resting heart rate (average 2-3 beats per minute), as noted in the product information.
Patients with a history of diabetic retinopathy require careful consideration, as the SUSTAIN-6 trial identified a higher incidence of retinopathy complications in the semaglutide group, particularly in those with pre-existing retinopathy and rapid improvement in blood glucose control. The National Institute for Health and Care Excellence (NICE) guidance for type 2 diabetes management (NG28) recommends SGLT2 inhibitors as the preferred option for patients with established cardiovascular disease, while GLP-1 receptor agonists like semaglutide are positioned based on glycaemic control and weight management criteria.
Heart-Related Side Effects to Monitor
Whilst Ozempic does not typically cause serious heart problems, patients and healthcare professionals should monitor for certain cardiovascular symptoms during treatment. Increased heart rate is a recognised effect, with clinical trials showing a mean increase of approximately 2-3 beats per minute. Patients who notice persistent palpitations, particularly if accompanied by chest discomfort or breathlessness, should report these symptoms to their healthcare provider.
Gastrointestinal side effects—including nausea, vomiting, and diarrhoea—can indirectly affect cardiovascular function through dehydration and electrolyte disturbances. Severe or prolonged gastrointestinal symptoms may lead to volume depletion, which can cause postural hypotension, dizziness, and compensatory tachycardia. Patients should maintain adequate hydration, particularly during the initial weeks of treatment when gastrointestinal effects are most pronounced.
Some patients report experiencing chest discomfort or tightness during treatment. It is crucial that any chest symptoms are properly evaluated, particularly in patients with cardiovascular risk factors. Patients should seek urgent medical attention for any concerning chest symptoms rather than assuming they are medication-related or gastrointestinal in origin.
Blood pressure changes should be monitored as clinically indicated, especially in patients taking antihypertensive medications. Whilst Ozempic typically produces modest reductions in blood pressure, this may necessitate adjustment of existing blood pressure medications to prevent hypotension. Healthcare professionals should be alert to symptoms of hypotension, including dizziness, light-headedness, and syncope, particularly when patients rise from sitting or lying positions.
Patients who experience any suspected side effects should report them to the MHRA through the Yellow Card Scheme (yellowcard.mhra.gov.uk).
Who Should Avoid Ozempic Due to Heart Conditions?
Ozempic has relatively few absolute contraindications related to cardiovascular conditions. The medication is not contraindicated in patients with established cardiovascular disease. However, certain clinical scenarios require careful consideration and may benefit from specialist input before initiating treatment.
Patients with severe heart failure (NYHA Class IV) have limited representation in clinical trials. While there is no evidence that Ozempic worsens heart failure, the limited data in patients with advanced cardiac dysfunction means treatment decisions should involve cardiology input and individualised risk-benefit assessment. The modest increase in heart rate associated with semaglutide may be a consideration in patients with compromised cardiac function.
Individuals with unstable angina or recent myocardial infarction (within the previous two months) were excluded from major clinical trials. This does not constitute an absolute contraindication, but reflects the need for cardiovascular stabilisation before introducing new medications. Patients who have recently experienced acute coronary events should have their cardiac status optimised before considering Ozempic initiation.
Uncontrolled tachyarrhythmias represent another scenario requiring caution. The medication's tendency to increase resting heart rate, albeit modestly, may be relevant in patients with atrial fibrillation, atrial flutter, or supraventricular tachycardia. These patients should have their arrhythmia adequately controlled before starting Ozempic, with appropriate monitoring during treatment.
Patients with pre-existing diabetic retinopathy should be aware of the potential risk of worsening retinopathy, particularly with rapid improvement in blood glucose control. Regular retinopathy screening is important for these patients. The presence of stable cardiovascular disease or cardiovascular risk factors should not preclude Ozempic use when clinically indicated according to NICE guidance.
When to Seek Medical Advice About Heart Symptoms
Patients taking Ozempic should be educated about symptoms that warrant prompt medical evaluation. Immediate medical attention (via 999 or emergency department) is required for symptoms suggesting acute cardiovascular events, including:
-
Severe chest pain or pressure, particularly if radiating to the arm, jaw, or back
-
Sudden onset breathlessness at rest or with minimal exertion
-
Loss of consciousness or near-syncope
-
Rapid or irregular heartbeat accompanied by chest pain, breathlessness, or dizziness
-
Symptoms of stroke, including facial drooping, arm weakness, or speech difficulties (remember the FAST acronym: Face, Arms, Speech, Time to call 999)
These symptoms require urgent assessment regardless of whether they are related to Ozempic, as they may indicate serious cardiovascular events requiring immediate intervention.
Non-urgent GP consultation (within 24-48 hours) is appropriate for less severe but concerning symptoms, including persistent palpitations without associated chest pain or breathlessness, unexplained fatigue or exercise intolerance that develops after starting Ozempic, recurrent dizziness or light-headedness (particularly postural), or new-onset ankle swelling. For urgent concerns that are not immediately life-threatening, patients can contact NHS 111 for advice.
Patients should also contact their GP or diabetes specialist nurse if they experience persistent gastrointestinal symptoms leading to inadequate fluid intake, as dehydration can affect cardiovascular function. Similarly, symptoms of hypoglycaemia (particularly in patients taking insulin or sulphonylureas concurrently) warrant medical review, as severe hypoglycaemia can precipitate cardiovascular events in susceptible individuals.
Monitoring should be individualised based on clinical need and risk factors. Patients with pre-existing cardiovascular disease may benefit from more frequent monitoring as determined by their healthcare team. The NHS recommends that patients attend their routine diabetes reviews (at least annually) and any additional appointments as advised by their diabetes care team. Open communication between patients and healthcare professionals remains essential for safe and effective Ozempic therapy.
Any suspected side effects should be reported to the MHRA through the Yellow Card Scheme (yellowcard.mhra.gov.uk).
Frequently Asked Questions
Can Ozempic increase my risk of heart attack or stroke?
No, clinical trials show that Ozempic does not increase the risk of heart attack or stroke. The SUSTAIN-6 study demonstrated a 26% reduction in major adverse cardiovascular events, including cardiovascular death, non-fatal myocardial infarction, and non-fatal stroke in high-risk patients with type 2 diabetes.
What heart-related side effects should I watch for whilst taking Ozempic?
Monitor for persistent palpitations, chest discomfort, breathlessness, or dizziness, particularly during treatment initiation or dose escalation. Ozempic can cause a modest increase in resting heart rate of 2-3 beats per minute. Report any concerning cardiovascular symptoms to your healthcare provider promptly.
Should I avoid Ozempic if I have existing heart disease?
Ozempic is not contraindicated in patients with established cardiovascular disease and may offer cardiovascular benefits. However, patients with severe heart failure, recent myocardial infarction, or uncontrolled tachyarrhythmias require individualised assessment and specialist input before starting treatment.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript