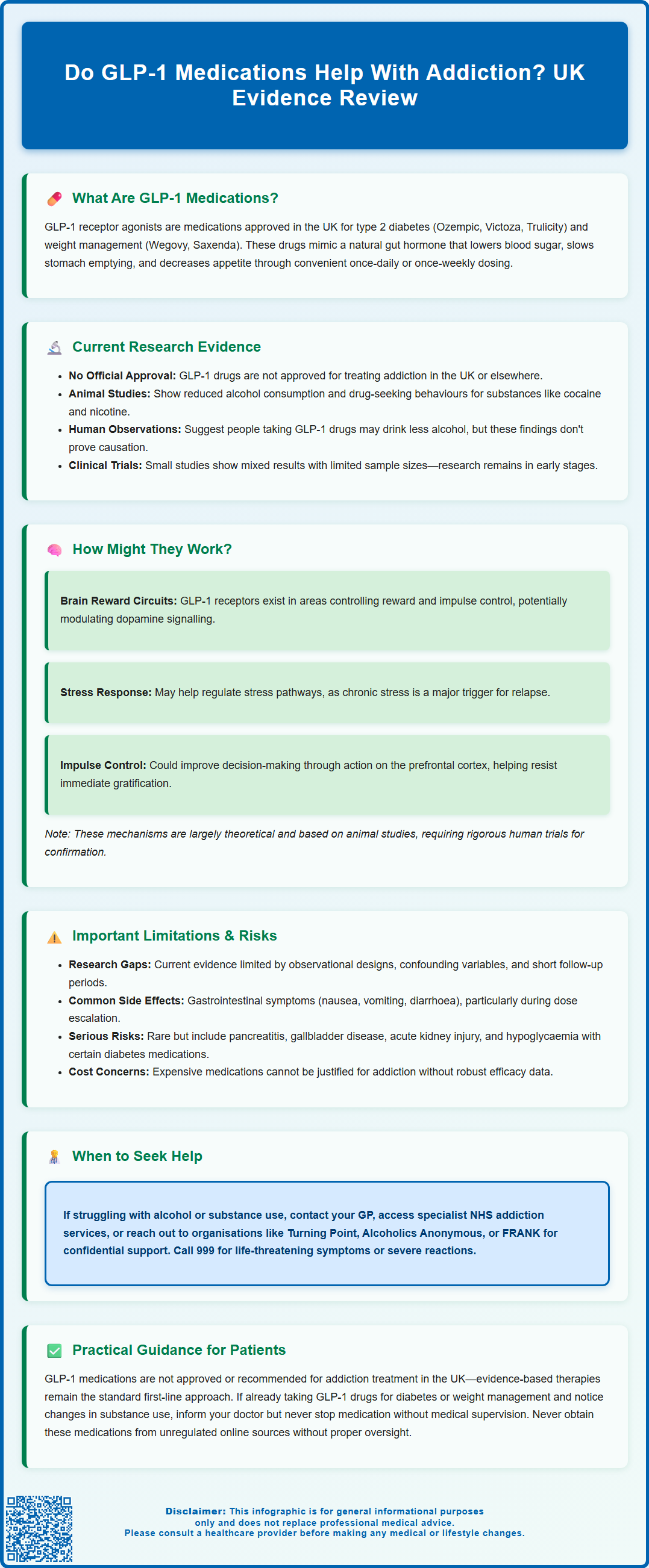
Glucagon-like peptide-1 (GLP-1) receptor agonists, such as semaglutide and liraglutide, are licensed in the UK for managing type 2 diabetes and obesity. Emerging research has sparked interest in whether these medications might influence addictive behaviours, following observations that GLP-1 receptors exist in brain reward pathways. Whilst preclinical studies and early observational data suggest potential effects on substance use, it is crucial to emphasise that GLP-1 medications are not licensed or recommended for treating addiction in the UK. This article examines the current evidence, proposed mechanisms, clinical limitations, and practical guidance for patients and healthcare professionals.
Summary: GLP-1 receptor agonists are not licensed or recommended for treating addiction in the UK, though emerging research suggests they may influence reward pathways and substance use behaviours.
- GLP-1 medications are licensed only for type 2 diabetes and weight management, not addiction treatment.
- Preclinical studies show reduced substance-seeking behaviours in animals; human evidence remains preliminary and observational.
- GLP-1 receptors in brain reward circuits may modulate dopamine signalling and impulse control, though mechanisms are theoretical.
- Current research has significant limitations including small sample sizes, short follow-up, and inability to establish causation.
- Evidence-based addiction treatments—psychological interventions and licensed pharmacotherapies—remain the standard of care in the UK.
Table of Contents
What Are GLP-1 Medications and How Do They Work?
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications originally developed for the management of type 2 diabetes mellitus and, more recently, some have been approved for weight management. In the UK, these medications have specific licensed indications:
-
Semaglutide: Available as Ozempic (for type 2 diabetes) and Wegovy (for weight management)
-
Liraglutide: Available as Victoza (for type 2 diabetes) and Saxenda (for weight management)
-
Dulaglutide: Available as Trulicity (for type 2 diabetes only)
GLP-1 is a naturally occurring incretin hormone released by the intestine in response to food intake. It plays a crucial role in glucose homeostasis by:
-
Enhancing insulin secretion from pancreatic beta cells in a glucose-dependent manner
-
Suppressing glucagon release, thereby reducing hepatic glucose production
-
Slowing gastric emptying, which moderates postprandial glucose excursions
-
Promoting satiety through actions on appetite centres in the brain
GLP-1 receptor agonists mimic these physiological effects but with extended half-lives, allowing for once-weekly or once-daily administration. The medications bind to GLP-1 receptors located not only in the pancreas and gastrointestinal tract but also in various brain regions, including areas involved in reward processing and appetite regulation.
Beyond their established metabolic benefits, emerging research has identified GLP-1 receptors in the mesolimbic dopamine system—the brain's reward pathway—which has sparked scientific interest in whether these medications might influence behaviours beyond eating, including addictive behaviours. This observation forms the basis for ongoing investigations into potential applications beyond diabetes and obesity management.
Current Evidence: GLP-1 Drugs and Addiction Research
The potential role of GLP-1 receptor agonists in modulating addictive behaviours represents an emerging area of research, though it is important to emphasise that there is no official indication or licence for these medications in treating addiction in the UK or elsewhere. Any use for addiction should be confined to clinical trials or specialist research settings.
Preclinical studies in animal models have demonstrated that GLP-1 receptor agonists can reduce the consumption of and preference for alcohol, as well as decrease drug-seeking behaviours for substances including cocaine, amphetamines, and nicotine. These findings have generated considerable scientific interest in translating such observations to human populations.
Observational human studies have provided preliminary signals that warrant further investigation. Several retrospective analyses of healthcare databases have suggested that individuals prescribed GLP-1 receptor agonists for diabetes or obesity may report reduced alcohol consumption compared to those on alternative treatments. A Swedish registry study published in 2023 found associations between GLP-1 agonist use and lower rates of hospitalisation for alcohol-related disorders, though such observational data cannot establish causation.
Small-scale clinical trials are now underway examining GLP-1 medications in alcohol use disorder and other substance dependencies. Early phase studies have shown mixed results. For example, a randomised controlled trial of exenatide in alcohol use disorder found benefits only in specific subgroups, highlighting the preliminary nature of this research. Most studies have small sample sizes and short follow-up periods.
It is crucial to recognise that this research is in its infancy. The National Institute for Health and Care Excellence (NICE) has not issued guidance on GLP-1 receptor agonists for addiction treatment, and these medications should not be considered established therapies for substance use disorders. Current evidence-based treatments for addiction—including psychological interventions, mutual support groups, and licensed pharmacotherapies—remain the standard of care.
Potential Mechanisms Behind GLP-1 Effects on Addictive Behaviours
Understanding the biological mechanisms through which GLP-1 receptor agonists might influence addictive behaviours requires examining the neuroanatomy of reward processing and how these medications interact with relevant brain circuits.
GLP-1 receptors are expressed in key reward-related brain regions, including:
-
The ventral tegmental area (VTA) and nucleus accumbens, which form the core of the mesolimbic dopamine pathway
-
The prefrontal cortex, involved in executive function and impulse control
-
The amygdala, which processes emotional salience and stress responses
The prevailing hypothesis suggests that GLP-1 receptor activation may modulate dopamine signalling in reward circuits. Addictive substances typically cause supraphysiological dopamine release in the nucleus accumbens, reinforcing drug-seeking behaviour. Preclinical research suggests GLP-1 receptor agonists may influence this reward response, potentially affecting the reinforcing properties of addictive substances, though human evidence remains limited.
Additionally, these medications may influence stress and anxiety pathways. Chronic stress is a well-established trigger for relapse in substance use disorders, and GLP-1 signalling has been implicated in stress response regulation in animal models. By potentially modulating stress-induced craving, GLP-1 agonists might offer a dual mechanism of action, though this remains hypothetical in humans.
Another proposed mechanism involves impulse control and decision-making. GLP-1 receptors in the prefrontal cortex may enhance executive function, potentially improving an individual's ability to resist immediate gratification in favour of longer-term goals—a cognitive process often impaired in addiction.
It is important to note that these mechanisms remain theoretical and are based largely on preclinical research. The translation of these findings to clinical practice requires rigorous investigation through properly designed randomised controlled trials with appropriate outcome measures and safety monitoring.
Clinical Considerations and Limitations of Current Research
Healthcare professionals and patients should approach the potential use of GLP-1 receptor agonists for addiction with appropriate caution, recognising significant limitations in the current evidence base.
Methodological limitations of existing research include:
-
Observational study designs that cannot establish causation—individuals prescribed GLP-1 agonists may differ systematically from comparison groups
-
Confounding variables such as concurrent lifestyle interventions, psychological support, or other medications
-
Short follow-up periods that do not capture long-term outcomes or relapse patterns
-
Publication bias, with positive findings more likely to be reported than null results
Safety considerations are paramount. GLP-1 receptor agonists carry recognised adverse effects that must be weighed against any potential benefits:
-
Gastrointestinal symptoms (nausea, vomiting, diarrhoea) occur commonly, particularly during dose escalation
-
Risk of pancreatitis, though rare, requires clinical vigilance; treatment should be discontinued if pancreatitis is suspected
-
Gallbladder disease including cholelithiasis and cholecystitis has been reported, particularly with weight loss
-
Dehydration and acute kidney injury risk, especially during treatment initiation
-
Diabetic retinopathy complications have been associated with rapid glucose improvement (particularly with semaglutide)
-
Hypoglycaemia risk when combined with insulin or sulphonylureas
According to UK product information, GLP-1 receptor agonists are not recommended during pregnancy or breastfeeding when used for weight management. Those used for diabetes require individual benefit-risk assessment in pregnancy.
Regarding drug interactions, UK SmPCs indicate few clinically significant pharmacokinetic interactions. However, the delayed gastric emptying effect may affect the absorption of some oral medications, which may need to be considered for certain drugs with narrow therapeutic windows.
Cost-effectiveness represents another consideration. GLP-1 receptor agonists are expensive medications, and without robust efficacy data for addiction treatment, their use for this indication cannot be justified from a health economics perspective. NHS resources must be allocated based on evidence-based interventions with demonstrated clinical and cost-effectiveness.
What This Means for Patients: Practical Guidance
If you are struggling with addiction or substance use concerns, it is essential to understand that GLP-1 receptor agonists are not currently recommended or licensed treatments for addiction in the UK. Evidence-based treatments remain the appropriate first-line approach.
If you are experiencing problems with alcohol or substance use, you should:
-
Contact your GP to discuss your concerns in a confidential, non-judgemental setting
-
Access specialist addiction services through NHS referral pathways or organisations such as Turning Point, We Are With You, or Alcoholics Anonymous
-
Consider evidence-based treatments including cognitive behavioural therapy, motivational interviewing, and where appropriate, licensed pharmacotherapies
-
Visit NHS support pages for alcohol support (www.nhs.uk/live-well/alcohol-advice/alcohol-support) or drug addiction help (www.nhs.uk/live-well/addiction-support/drug-addiction-getting-help)
-
Contact FRANK (www.talktofrank.com) for confidential drug information and advice
If you are already taking a GLP-1 receptor agonist for diabetes or weight management and notice changes in your substance use patterns:
-
Inform your prescribing clinician about any changes you observe
-
Do not alter your medication regimen without medical supervision
-
Continue with your prescribed treatment plan for your licensed indication
-
Seek appropriate addiction support through established pathways if needed
Important safety advice:
-
Never obtain GLP-1 medications from unregulated sources or online pharmacies without proper medical oversight
-
These medications require careful dose titration and monitoring for adverse effects
-
Self-medication for addiction is potentially dangerous and may delay access to effective treatments
-
Report any suspected side effects to the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk)
When to seek medical attention:
-
Call 999 for life-threatening symptoms
-
Contact NHS 111 for urgent medical advice when your GP is unavailable
-
Seek immediate medical help for severe, persistent abdominal pain (potential pancreatitis)
-
Signs of allergic reaction (rash, difficulty breathing, facial swelling)
-
Symptoms of severe hypoglycaemia if taking other diabetes medications
-
Any concerning symptoms or medication side effects
Whilst research into GLP-1 receptor agonists and addiction continues, patients deserve access to proven, evidence-based treatments. Speak with your healthcare provider about the most appropriate support for your individual circumstances.
Frequently Asked Questions
Are GLP-1 medications approved for treating addiction in the UK?
No, GLP-1 receptor agonists are not licensed or approved for addiction treatment in the UK. They are only licensed for managing type 2 diabetes and weight management, and any use for addiction should be confined to clinical trials or specialist research settings.
What evidence exists for GLP-1 drugs reducing addictive behaviours?
Evidence is preliminary and includes animal studies showing reduced substance-seeking behaviours and observational human data suggesting lower alcohol consumption. However, these studies cannot establish causation, and rigorous randomised controlled trials are needed before any clinical recommendations can be made.
What should I do if I'm struggling with addiction?
Contact your GP to discuss concerns confidentially, access specialist NHS addiction services, or contact organisations such as We Are With You, FRANK, or Alcoholics Anonymous. Evidence-based treatments including psychological therapies and licensed pharmacotherapies remain the appropriate first-line approach for substance use disorders.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript