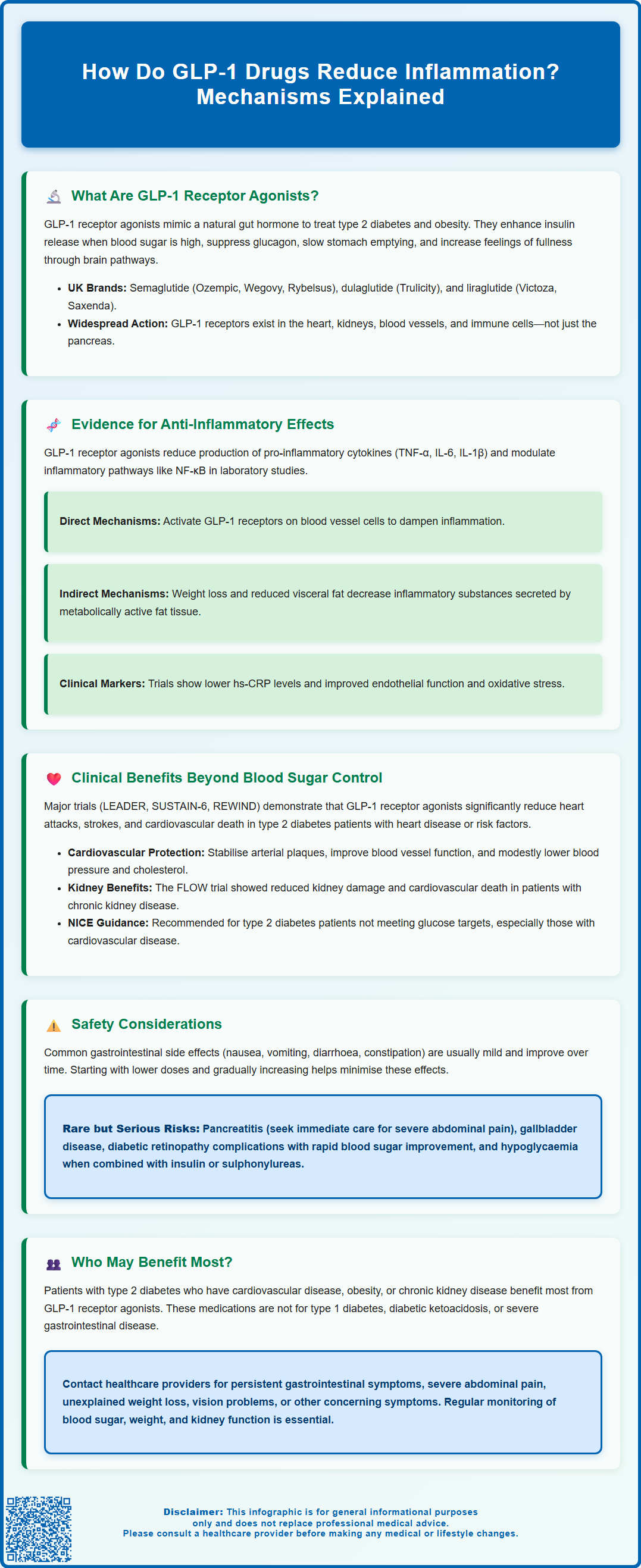
GLP-1 receptor agonists, such as semaglutide and liraglutide, are medications primarily used to manage type 2 diabetes and obesity. Emerging research suggests these drugs may reduce inflammation through multiple mechanisms, potentially contributing to their cardiovascular and renal benefits. Whilst their anti-inflammatory properties are not yet fully understood, evidence indicates they may lower pro-inflammatory markers and modulate immune pathways. This article explores how GLP-1 drugs may reduce inflammation, the clinical implications of these effects, and important safety considerations for patients and healthcare professionals in the UK.
Summary: GLP-1 receptor agonists may reduce inflammation by decreasing pro-inflammatory cytokines, modulating immune signalling pathways, and indirectly through weight loss and improved metabolic health.
- GLP-1 receptor agonists are medications for type 2 diabetes and obesity that mimic the incretin hormone GLP-1.
- These drugs may lower inflammatory markers including C-reactive protein, TNF-α, IL-6, and IL-1β through direct receptor activation and indirect metabolic improvements.
- Anti-inflammatory effects may contribute to cardiovascular and renal benefits observed in clinical trials beyond glucose control alone.
- Common side effects include gastrointestinal symptoms; rare serious effects include pancreatitis and gallbladder disease requiring monitoring.
- GLP-1 receptor agonists are not licensed specifically as anti-inflammatory agents and prescribing follows diabetes and weight management indications under NICE guidance.
Table of Contents
What Are GLP-1 Receptor Agonists?
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications primarily prescribed for the management of type 2 diabetes mellitus and, more recently, for weight management in adults with obesity. These drugs mimic the action of naturally occurring GLP-1, an incretin hormone released by the intestine in response to food intake.
The mechanism of action involves binding to GLP-1 receptors found predominantly in pancreatic beta cells, where they enhance glucose-dependent insulin secretion. Crucially, this glucose-dependent mechanism means insulin is only released when blood glucose levels are elevated, thereby reducing the risk of hypoglycaemia compared with some other diabetes medications. GLP-1 receptor agonists also suppress glucagon secretion from pancreatic alpha cells, slow gastric emptying, and promote satiety through central nervous system pathways.
Commonly prescribed GLP-1 receptor agonists in the UK include semaglutide (available as injectable Ozempic and Wegovy, and oral Rybelsus), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda). Most of these medications are administered via subcutaneous injection, with dosing frequencies ranging from twice daily to once weekly depending on the specific formulation. Oral semaglutide (Rybelsus) is taken once daily in a fasting state.
Whilst their primary indication remains glycaemic control, emerging evidence suggests GLP-1 receptor agonists exert effects beyond glucose metabolism. GLP-1 receptors have been identified in various tissues throughout the body, including the cardiovascular system, kidneys, and vascular endothelium. Some preclinical studies suggest expression on certain immune cells, though human evidence is variable. This widespread receptor distribution has prompted investigation into potential pleiotropic effects, including anti-inflammatory properties that may contribute to their broader clinical benefits in cardiometabolic disease.
Evidence for Anti-Inflammatory Effects of GLP-1 Drugs
Accumulating preclinical and clinical evidence suggests that GLP-1 receptor agonists may possess anti-inflammatory properties that extend beyond their metabolic effects. Multiple mechanisms have been proposed to explain these observations, though the precise pathways remain an active area of research.
Laboratory studies have demonstrated that GLP-1 receptor activation can reduce the production of pro-inflammatory cytokines, including tumour necrosis factor-alpha (TNF-α), interleukin-6 (IL-6), and interleukin-1 beta (IL-1β). These cytokines play central roles in chronic low-grade inflammation associated with obesity, insulin resistance, and cardiovascular disease. In preclinical models, GLP-1 receptor agonists appear to modulate inflammatory signalling pathways such as nuclear factor kappa B (NF-κB), a key transcription factor regulating inflammatory gene expression.
In human studies, treatment with GLP-1 receptor agonists has been associated with reductions in circulating inflammatory markers. Clinical trials have reported decreases in high-sensitivity C-reactive protein (hs-CRP), a well-established biomarker of systemic inflammation and cardiovascular risk. Some studies have also documented improvements in markers of endothelial dysfunction and oxidative stress, processes intimately linked with vascular inflammation.
The anti-inflammatory effects may be both direct and indirect. Potential direct mechanisms involve GLP-1 receptor activation on vascular endothelial cells and possibly immune cells, though human evidence for the latter is variable. Indirect mechanisms relate to weight loss, improved glycaemic control, and reduced visceral adiposity—all of which independently contribute to lower inflammatory burden. Adipose tissue, particularly visceral fat, is metabolically active and secretes pro-inflammatory adipokines; reduction in adipose mass therefore diminishes this inflammatory source.
It is important to note that whilst these findings are promising, there is no official consensus on GLP-1 receptor agonists being prescribed specifically as anti-inflammatory agents. Current prescribing remains guided by licensed indications for diabetes and weight management.
Clinical Benefits Beyond Blood Sugar Control
The potential anti-inflammatory properties of GLP-1 receptor agonists may contribute to their demonstrated cardiovascular and renal benefits, which have been observed in large-scale cardiovascular outcome trials. These benefits appear to exceed what would be expected from glucose lowering alone, suggesting additional protective mechanisms.
Cardiovascular outcomes trials such as LEADER (liraglutide), SUSTAIN-6 (semaglutide), and REWIND (dulaglutide) have shown that certain GLP-1 receptor agonists significantly reduce major adverse cardiovascular events (MACE), including cardiovascular death, non-fatal myocardial infarction, and non-fatal stroke in patients with type 2 diabetes and established cardiovascular disease or multiple risk factors. The MHRA and European Medicines Agency (EMA) have recognised these benefits in their product information. It's important to note that these cardiovascular benefits are not uniform across all GLP-1 receptor agonists.
Reduction in vascular inflammation may contribute to these cardioprotective effects. Atherosclerosis is fundamentally an inflammatory disease, characterised by chronic inflammation within arterial walls. By potentially dampening inflammatory processes, GLP-1 receptor agonists may help stabilise atherosclerotic plaques, improve endothelial function, and reduce thrombotic risk. Additionally, these medications have been shown to modestly reduce blood pressure and improve lipid profiles, further supporting cardiovascular health.
Renal protection has also been documented, with trials demonstrating reduced progression of diabetic kidney disease. The FLOW trial with semaglutide showed significant reductions in kidney disease progression and cardiovascular death in patients with type 2 diabetes and chronic kidney disease. Anti-inflammatory mechanisms may play a role here, as chronic inflammation contributes to glomerular injury and tubulointerstitial fibrosis.
NICE guidance (NG28) recommends considering GLP-1 receptor agonists for adults with type 2 diabetes when glycaemic targets are not achieved with other therapies, particularly in those with established cardiovascular disease or at high cardiovascular risk. For patients with chronic kidney disease or heart failure, SGLT2 inhibitors are generally prioritised, with GLP-1 receptor agonists as complementary therapy where appropriate. The broader benefits beyond glucose control are increasingly recognised in clinical decision-making, though prescribing decisions should be individualised based on patient characteristics, comorbidities, and treatment goals.
Safety Considerations and Who May Benefit
Whilst GLP-1 receptor agonists are generally well-tolerated, understanding their adverse effect profile is essential for appropriate patient selection and monitoring. The most common side effects are gastrointestinal, including nausea, vomiting, diarrhoea, and constipation. These symptoms are typically mild to moderate, occur most frequently during dose titration, and often improve with continued treatment. Starting at lower doses and gradually increasing can help minimise these effects.
Rare but serious adverse effects include pancreatitis, though causality remains debated. Patients should be advised to seek immediate medical attention if they experience severe, persistent abdominal pain. There have been reports of gallbladder disease, including cholelithiasis and cholecystitis, possibly related to rapid weight loss. UK product information includes warnings about thyroid C-cell tumours observed in rodent studies, though this is not a formal contraindication in the UK as it is in some other countries.
Patients should be aware of the risk of diabetic retinopathy complications, particularly with semaglutide, especially in those with pre-existing retinopathy and rapid improvements in blood glucose. When GLP-1 receptor agonists are used with insulin or sulfonylureas, there is an increased risk of hypoglycaemia, and dose reductions of these medications may be needed.
GLP-1 receptor agonists are not indicated for type 1 diabetes and should not be used in patients with diabetic ketoacidosis. Caution is advised in those with severe gastrointestinal disease, including gastroparesis, as delayed gastric emptying may exacerbate symptoms. These medications are not recommended during pregnancy or breastfeeding, and women of childbearing potential should use effective contraception. For planned pregnancies, semaglutide should be discontinued at least 2 months before conception due to its long half-life.
Patients who may particularly benefit from GLP-1 receptor agonists include those with type 2 diabetes and established cardiovascular disease, obesity, or chronic kidney disease (where SGLT2 inhibitors are not suitable or as additional therapy). GLP-1 receptor agonists should not be combined with DPP-4 inhibitors as there is limited added benefit.
Patients should contact their healthcare professional if they experience persistent gastrointestinal symptoms, signs of pancreatitis, unexplained weight loss beyond expected, new or worsening vision problems, or any concerning symptoms. Regular follow-up is recommended to monitor glycaemic control, weight, renal function, and tolerability. Patients should report any suspected side effects via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk or via the Yellow Card app). Healthcare professionals should provide comprehensive counselling about realistic expectations, potential side effects, and the importance of lifestyle modifications alongside pharmacotherapy for optimal outcomes in cardiometabolic health.
Frequently Asked Questions
Can GLP-1 receptor agonists be prescribed specifically to reduce inflammation?
No, GLP-1 receptor agonists are not currently licensed or prescribed specifically as anti-inflammatory agents. Their approved indications in the UK remain type 2 diabetes management and weight management in adults with obesity, though anti-inflammatory effects may contribute to their broader cardiovascular and metabolic benefits.
Which inflammatory markers do GLP-1 drugs affect?
Clinical studies have shown GLP-1 receptor agonists may reduce high-sensitivity C-reactive protein (hs-CRP), tumour necrosis factor-alpha (TNF-α), interleukin-6 (IL-6), and interleukin-1 beta (IL-1β). These are key markers of systemic inflammation associated with cardiovascular disease and metabolic disorders.
Are the anti-inflammatory effects of GLP-1 drugs direct or indirect?
The anti-inflammatory effects appear to be both direct and indirect. Direct mechanisms may involve GLP-1 receptor activation on vascular endothelial cells, whilst indirect effects result from weight loss, improved glycaemic control, and reduced visceral adiposity, all of which independently lower inflammatory burden.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript