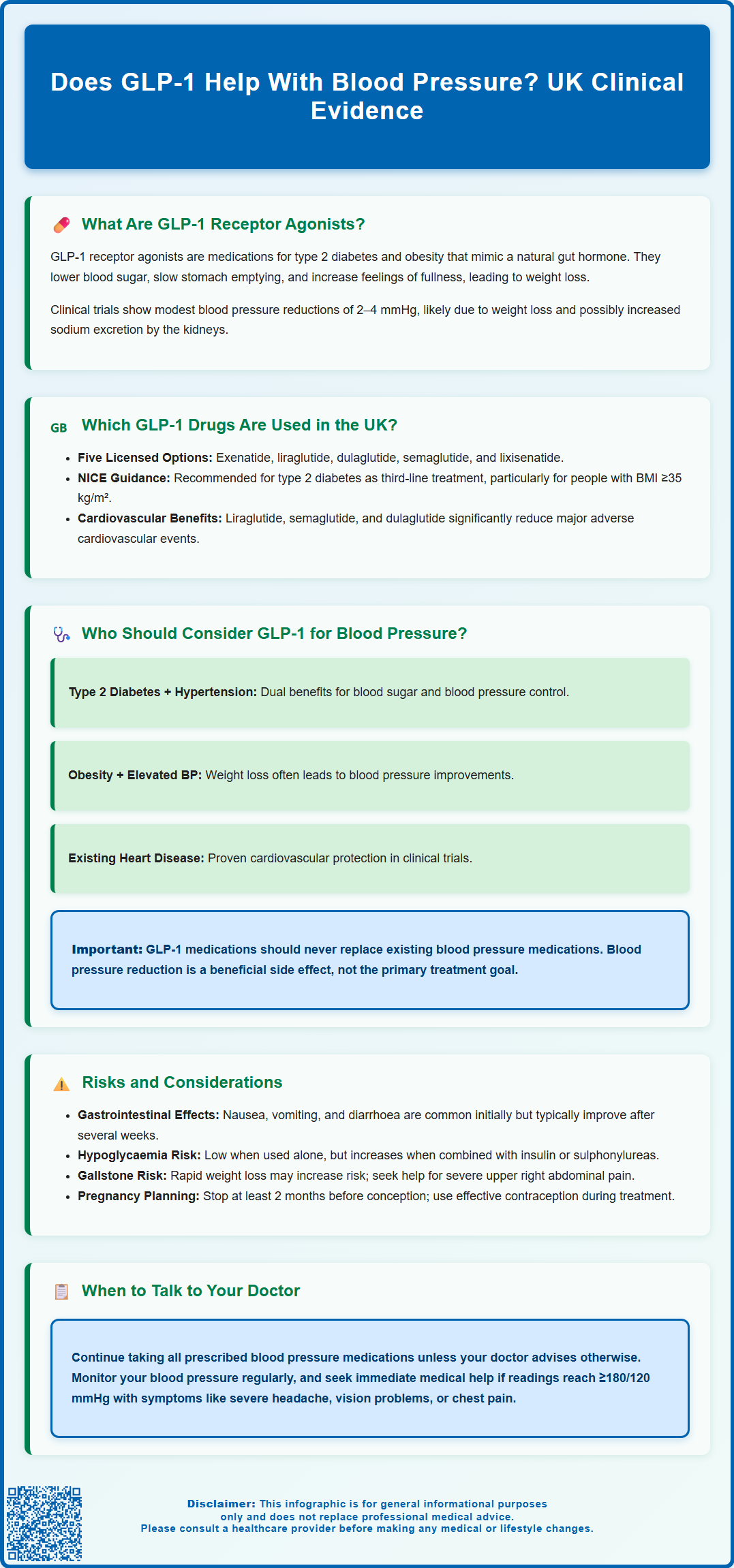
GLP-1 receptor agonists, primarily licensed for type 2 diabetes and obesity management, have demonstrated modest blood pressure-lowering effects in clinical trials. Whilst not approved specifically as antihypertensive agents in the UK, these medications may reduce systolic blood pressure by approximately 2–4 mmHg alongside their metabolic benefits. This article examines the evidence for blood pressure reduction with GLP-1 therapy, identifies which patients may benefit most from this additional effect, and outlines important safety considerations. Understanding these cardiovascular effects helps clinicians and patients make informed decisions when managing coexisting metabolic and cardiovascular conditions.
Summary: GLP-1 receptor agonists can modestly reduce systolic blood pressure by approximately 2–4 mmHg, though they are not licensed specifically as antihypertensive medications in the UK.
- GLP-1 receptor agonists are primarily licensed for type 2 diabetes mellitus and obesity management, not hypertension treatment.
- Blood pressure reduction likely occurs through multiple mechanisms including weight loss, potential natriuresis, and possible improvements in endothelial function.
- Cardiovascular outcome trials for liraglutide, semaglutide, and dulaglutide demonstrated modest blood pressure reductions alongside reduced major adverse cardiovascular events.
- Patients with coexisting type 2 diabetes and hypertension, or obesity with elevated blood pressure, may derive particular benefit from these additional cardiovascular effects.
- Common adverse effects include gastrointestinal symptoms, and patients taking multiple antihypertensive medications require regular blood pressure monitoring to avoid excessive lowering.
- GLP-1 therapy should not replace established antihypertensive medications and must be prescribed according to NICE guidance for licensed indications.
Table of Contents
What Are GLP-1 Receptor Agonists?
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications primarily licensed for the management of type 2 diabetes mellitus and, more recently, obesity. These drugs are mostly available as injectable formulations, though an oral option (semaglutide/Rybelsus) is also available. They work by mimicking the action of naturally occurring GLP-1, an incretin hormone released from the intestine in response to food intake.
The mechanism of action involves several physiological pathways. GLP-1 receptor agonists bind to GLP-1 receptors on pancreatic beta cells, stimulating glucose-dependent insulin secretion whilst suppressing glucagon release. This dual action helps regulate blood glucose levels with a low risk of hypoglycaemia when used alone (though this risk increases when combined with insulin or sulphonylureas). Additionally, these medications slow gastric emptying, which contributes to improved postprandial glucose control and promotes satiety, leading to reduced caloric intake and weight loss.
Beyond their primary metabolic effects, emerging evidence suggests cardiovascular benefits, including potential blood pressure reduction. GLP-1 receptors are expressed in various tissues beyond the pancreas, including the heart, blood vessels, and kidneys. Several mechanisms may potentially contribute to blood pressure effects, including: weight loss (a well-established factor in blood pressure reduction), possible promotion of natriuresis (sodium excretion by the kidneys), and theoretical improvements in endothelial function—though many of these mechanisms remain hypothetical rather than definitively proven.
Whilst GLP-1 receptor agonists are not licensed specifically as antihypertensive agents in the UK, the Medicines and Healthcare products Regulatory Agency (MHRA) has approved several formulations for glycaemic control and weight management. The observed modest blood pressure reductions in clinical trials have generated considerable interest amongst clinicians managing patients with coexisting metabolic conditions and hypertension.
Which GLP-1 Drugs Are Used in the UK?
Several GLP-1 receptor agonists are available through the NHS and private prescription in the United Kingdom, each with distinct pharmacokinetic profiles and administration schedules. Understanding these differences helps clinicians and patients make informed treatment decisions.
Currently licensed GLP-1 receptor agonists in the UK include:
-
Exenatide (Bydureon) – once-weekly formulation (note: Byetta twice-daily formulation has been discontinued in the UK)
-
Liraglutide (Victoza for diabetes; Saxenda for weight management) – administered once daily
-
Dulaglutide (Trulicity) – once-weekly injection
-
Semaglutide (Ozempic for diabetes; Wegovy for weight management) – once-weekly injection; oral formulation (Rybelsus) also available
-
Lixisenatide (Lyxumia) – once-daily injection
NICE guidance for type 2 diabetes (NG28) recommends GLP-1 receptor agonists in specific circumstances: typically as a third-line option when other treatments haven't achieved adequate glycaemic control, particularly in people with a BMI ≥35 kg/m² (adjusted for ethnicity), or for whom weight loss would benefit other obesity-related comorbidities, or for whom insulin would have significant occupational implications. For obesity management, NICE technology appraisals recommend liraglutide 3.0 mg or semaglutide 2.4 mg only as part of a specialist weight management service for adults with a BMI of ≥35 kg/m² (or ≥32.5 kg/m² for people from certain ethnic backgrounds) and at least one weight-related comorbidity. Treatment continuation depends on achieving specific weight loss targets at defined intervals.
The cardiovascular outcome trials for several of these agents have demonstrated varying results. Liraglutide (LEADER trial), semaglutide (SUSTAIN-6), and dulaglutide (REWIND trial) demonstrated significant reductions in major adverse cardiovascular events, while others showed cardiovascular safety without superiority. These trials consistently reported modest reductions in systolic blood pressure, typically ranging from 2–4 mmHg, which may contribute to their cardiovascular effects. The magnitude of blood pressure reduction varies between agents and individual patient factors.
Who Should Consider GLP-1 for Blood Pressure Management?
Whilst GLP-1 receptor agonists are not prescribed solely for hypertension management, certain patient populations may derive particular benefit from their blood pressure-lowering effects alongside their primary metabolic indications.
Patients who may benefit most include:
-
Adults with type 2 diabetes and hypertension – This represents a common clinical scenario where metabolic and cardiovascular risk factors coexist. GLP-1 therapy addresses hyperglycaemia whilst potentially contributing to blood pressure reduction, simplifying the therapeutic regimen.
-
Individuals with obesity and elevated blood pressure – Weight loss achieved through GLP-1 therapy often correlates with blood pressure improvements. For patients meeting NICE criteria for weight management therapy (BMI ≥35 kg/m² with adjustment for ethnicity, presence of weight-related comorbidities, and treatment through specialist weight management services), the dual benefit of weight reduction and blood pressure lowering may be particularly valuable.
-
Patients with established cardiovascular disease – Those with previous myocardial infarction, stroke, or peripheral arterial disease may benefit from the cardioprotective effects of certain GLP-1 receptor agonists, which include modest blood pressure reductions alongside other cardiovascular benefits.
-
People with type 2 diabetes requiring multiple antihypertensive medications – For patients struggling to achieve blood pressure targets despite multiple antihypertensive drugs, the additional blood pressure-lowering effect of GLP-1 therapy may contribute to better overall control.
Important considerations: GLP-1 receptor agonists should not replace established antihypertensive medications and should only be initiated for their licensed indications according to NICE guidance. Any blood pressure reduction should be viewed as a beneficial additional effect rather than the primary therapeutic goal.
According to NICE guidance (NG136), hypertension is generally diagnosed when clinic blood pressure is ≥140/90 mmHg and subsequent ambulatory or home blood pressure monitoring confirms readings ≥135/85 mmHg. If you experience very high blood pressure (≥180/120 mmHg) with symptoms such as severe headache, vision problems, chest pain, or difficulty breathing, seek immediate medical attention.
Patients should continue their prescribed antihypertensive regimen unless advised otherwise by their healthcare professional. Regular blood pressure monitoring remains essential, and adjustments to antihypertensive therapy should be made in consultation with healthcare professionals.
Risks and Considerations When Using GLP-1
Like all medications, GLP-1 receptor agonists carry potential adverse effects that patients and prescribers must consider carefully. Understanding these risks enables informed decision-making and appropriate monitoring.
Common adverse effects include:
-
Gastrointestinal symptoms – Nausea, vomiting, diarrhoea, and constipation are the most frequently reported side effects, particularly during treatment initiation. These symptoms typically diminish over several weeks as tolerance develops. Gradual dose titration helps minimise gastrointestinal disturbance. Maintaining adequate hydration is important, especially if experiencing vomiting or diarrhoea, to prevent dehydration and potential kidney problems.
-
Injection site reactions – Mild redness, itching, or discomfort at injection sites may occur but are generally self-limiting.
-
Hypoglycaemia risk – When used as monotherapy, GLP-1 receptor agonists carry minimal hypoglycaemia risk due to their glucose-dependent mechanism. However, when combined with insulin or sulphonylureas, the risk increases, and dose adjustments of these concurrent medications may be necessary.
Other important considerations:
-
Gallbladder disease – GLP-1 receptor agonists, particularly when causing rapid weight loss, may increase the risk of gallstones and gallbladder inflammation. Contact your doctor if you experience severe abdominal pain, particularly in the upper right side, with or without fever and jaundice.
-
Thyroid concerns – Animal studies identified thyroid C-cell tumours with GLP-1 receptor agonists. The relevance to humans is uncertain, but patients should report any symptoms such as a lump in the neck, difficulty swallowing, or persistent hoarseness.
-
Diabetic retinopathy – Rapid improvement in glycaemic control, particularly with semaglutide, may temporarily worsen diabetic retinopathy. Patients with pre-existing retinopathy require careful ophthalmological monitoring.
-
Pregnancy and breastfeeding – GLP-1 receptor agonists are generally not recommended during pregnancy or breastfeeding. Women of childbearing potential should use effective contraception and discontinue treatment before planned pregnancy (for semaglutide, at least 2 months before conception).
-
Medication interactions – By slowing gastric emptying, GLP-1 receptor agonists may affect the absorption of some oral medications. Discuss all medications with your healthcare provider.
Regarding blood pressure specifically, the modest reductions observed are generally beneficial. However, patients taking multiple antihypertensive medications should have their blood pressure monitored regularly, as excessive lowering could potentially cause symptomatic hypotension, particularly in elderly patients or those with autonomic dysfunction. If you experience dizziness, light-headedness, or fainting whilst taking GLP-1 therapy, contact your GP promptly for blood pressure assessment and potential medication adjustment.
If you suspect you're experiencing side effects from GLP-1 receptor agonists, report them to your healthcare provider and consider using the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk) to help monitor medication safety.
Frequently Asked Questions
Can GLP-1 receptor agonists replace my blood pressure medications?
No, GLP-1 receptor agonists should not replace established antihypertensive medications. They are licensed for diabetes and obesity management, and any blood pressure reduction should be viewed as a beneficial additional effect rather than the primary therapeutic goal.
Which GLP-1 medications have shown cardiovascular benefits in clinical trials?
Liraglutide (LEADER trial), semaglutide (SUSTAIN-6), and dulaglutide (REWIND trial) demonstrated significant reductions in major adverse cardiovascular events. These trials consistently reported modest systolic blood pressure reductions of 2–4 mmHg.
Should I monitor my blood pressure differently when taking GLP-1 therapy?
Yes, regular blood pressure monitoring remains essential, particularly if you take multiple antihypertensive medications. Contact your GP if you experience dizziness, light-headedness, or fainting, as medication adjustments may be needed to prevent excessive blood pressure lowering.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript