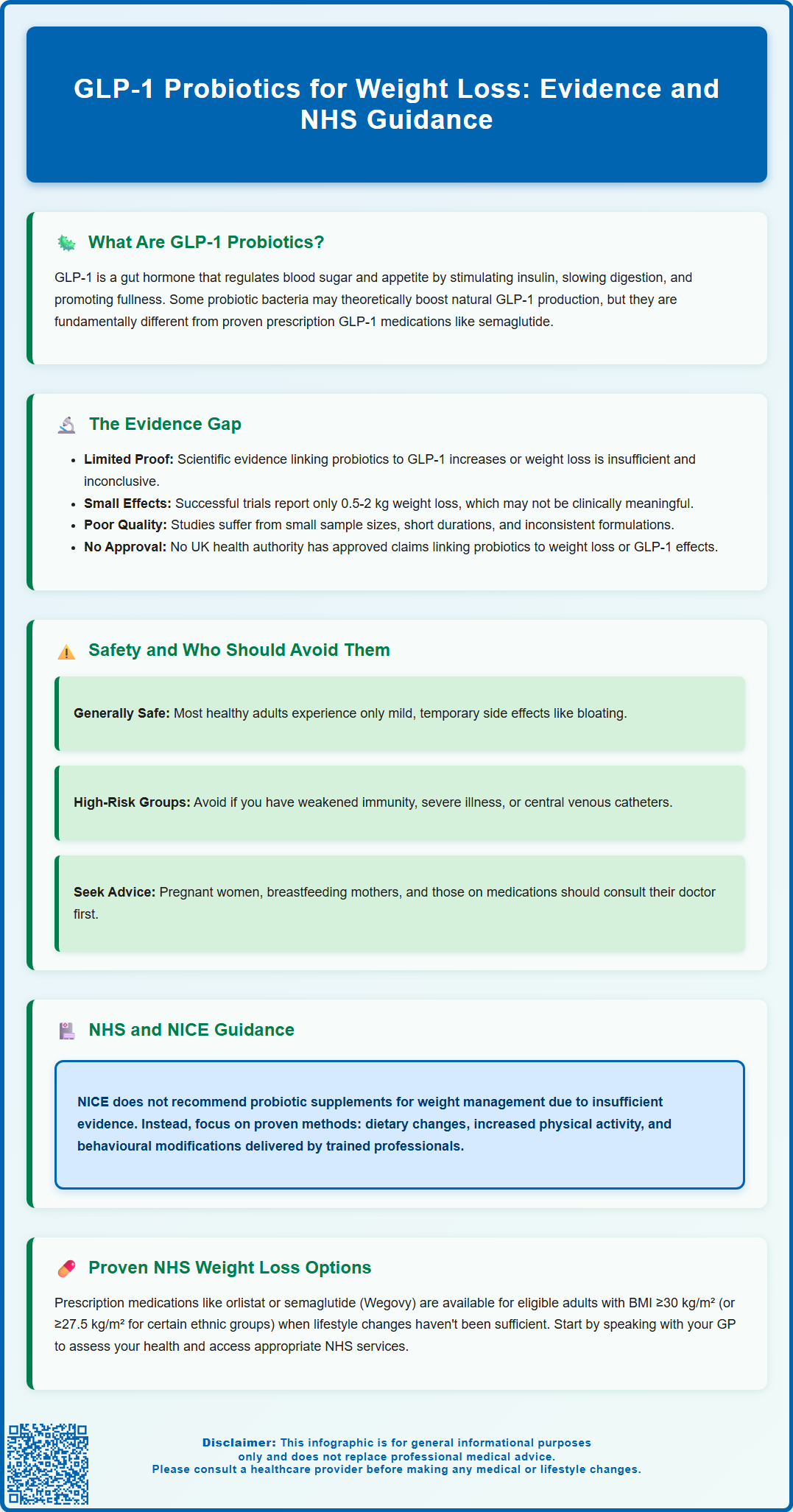
GLP-1 probiotics have emerged as a popular topic in weight management discussions, with some supplements claiming to enhance the body's natural production of glucagon-like peptide-1 (GLP-1), a gut hormone involved in appetite regulation and glucose control. Whilst certain probiotic strains may influence gut hormone secretion through metabolite production, it is crucial to understand that no probiotic supplement is licensed in the UK to modulate GLP-1 or treat obesity. These products differ fundamentally from prescription GLP-1 receptor agonist medications, which have robust clinical evidence and MHRA approval. This article examines the science behind GLP-1 probiotics, evaluates the current evidence, and outlines NHS-recommended approaches to weight management.
Summary: No probiotic supplement is licensed in the UK to modulate GLP-1 or treat obesity, and current evidence does not support their use as effective weight loss interventions.
- GLP-1 probiotics refer to bacterial strains theoretically influencing endogenous GLP-1 production through metabolites like short-chain fatty acids, distinct from licensed pharmaceutical GLP-1 receptor agonists.
- Clinical evidence for probiotics in weight management remains limited and inconclusive, with modest effects typically not meeting standards for regulatory health claims approval.
- Probiotics are generally safe for healthy adults but should be avoided by immunocompromised individuals, critically ill patients, and those with severe acute pancreatitis without medical supervision.
- NICE guidelines recommend multicomponent lifestyle interventions as the foundation for weight management, with pharmacological options like semaglutide reserved for specific patient groups meeting eligibility criteria.
- Probiotic supplements are regulated as food products rather than medicines in the UK, without the rigorous safety and efficacy testing required for pharmaceutical treatments.
Table of Contents
What Are GLP-1 Probiotics and How Do They Work?
Glucagon-like peptide-1 (GLP-1) is a naturally occurring hormone produced in the intestines that plays a crucial role in regulating blood glucose levels and appetite. When food enters the digestive system, specialised cells in the gut release GLP-1, which stimulates insulin secretion, slows gastric emptying, and promotes feelings of satiety. These mechanisms have made GLP-1 a target for pharmaceutical interventions in type 2 diabetes and obesity management.
The concept of 'GLP-1 probiotics' refers to specific strains of beneficial bacteria that may influence the body's natural production of GLP-1. Certain probiotic strains, particularly those from the Lactobacillus and Bifidobacterium families, have been studied for their potential to modulate gut hormone secretion. The proposed mechanism involves these bacteria producing metabolites—such as short-chain fatty acids (SCFAs)—that interact with enteroendocrine cells in the intestinal lining, potentially stimulating endogenous GLP-1 release.
It is important to distinguish between GLP-1 receptor agonist medications (such as semaglutide and liraglutide, which are licensed pharmaceutical treatments) and probiotic supplements marketed with claims about GLP-1 modulation. Whilst prescription GLP-1 agonists have robust clinical evidence and regulatory approval from the MHRA for weight management and diabetes control, probiotic products claiming to enhance GLP-1 activity represent a different category entirely. These supplements are classified as food products rather than medicines and are not subject to the same rigorous testing standards.
No probiotic supplement is licensed or authorised in the UK to modulate GLP-1 or treat obesity. Such claims would breach the Great Britain Nutrition and Health Claims Register rules and may be considered unlicensed medicinal claims.
The theoretical basis for GLP-1 probiotics centres on the gut microbiome's influence on metabolic health. Research has demonstrated that gut bacteria composition affects various aspects of metabolism, including glucose homeostasis and energy balance. However, translating these observations into effective probiotic interventions for weight loss remains an area of ongoing investigation, with significant gaps between laboratory findings and clinical applications.
Evidence for Probiotics in Weight Loss and Metabolic Health
The scientific evidence supporting probiotics specifically for GLP-1 modulation and weight loss remains limited and inconclusive. Whilst some laboratory studies and small-scale human trials have suggested that certain probiotic strains may influence gut hormone levels, there is currently no robust clinical evidence demonstrating that probiotic supplements can reliably increase GLP-1 production or lead to clinically significant weight loss in humans.
A systematic review of probiotic interventions for weight management has shown mixed and modest results. Some studies report small reductions in body weight or body mass index (BMI) with specific strains, whilst others find no significant effect. The heterogeneity in study designs, probiotic strains used, dosages, treatment durations, and participant populations makes it difficult to draw firm conclusions. Where positive effects have been observed, the magnitude of weight loss is typically small—generally in the range of 0.5-2 kg—which may not be clinically meaningful for most individuals seeking weight management.
Regarding GLP-1 specifically, research has demonstrated that certain gut bacteria can produce metabolites that stimulate GLP-1 secretion in animal models and cell culture studies. Short-chain fatty acids, particularly butyrate and propionate, have been shown to activate receptors on enteroendocrine L-cells, triggering GLP-1 release. However, there is no established link between taking probiotic supplements and achieving therapeutic increases in circulating GLP-1 levels comparable to those seen with pharmaceutical GLP-1 agonists.
The quality of available evidence is further limited by methodological concerns, including small sample sizes, short study durations, lack of standardisation in probiotic formulations, and potential publication bias favouring positive results. Neither the European Food Safety Authority (EFSA) nor the Great Britain Nutrition and Health Claims Register has approved health claims linking specific probiotics to weight loss or GLP-1 modulation due to insufficient evidence. Individuals considering probiotics for weight management should be aware that current scientific support does not justify replacing evidence-based treatments with probiotic supplements.
Safety Considerations and Who Should Avoid GLP-1 Probiotics
Probiotic supplements are generally considered safe for most healthy adults when taken as directed, with a long history of use and a favourable safety profile. Common side effects, when they occur, are typically mild and gastrointestinal in nature, including bloating, flatulence, and temporary changes in bowel habits. These symptoms usually resolve within a few days as the body adjusts to the supplement.
However, certain populations should exercise caution or avoid probiotics altogether without medical supervision. Individuals with compromised immune systems—including those undergoing chemotherapy, taking immunosuppressive medications, or living with HIV/AIDS—face a small but significant risk of probiotic-related infections. Whilst rare, cases of bacteraemia and fungaemia have been reported in immunocompromised patients taking probiotics. People with central venous catheters or other indwelling medical devices may also be at increased risk.
Critically ill patients and those with severe acute pancreatitis should avoid probiotics. The PROPATRIA trial published in the New England Journal of Medicine showed potential harm in patients with severe acute pancreatitis. Individuals with short bowel syndrome or compromised intestinal barrier function should consult their healthcare provider before starting probiotic supplements. Pregnant and breastfeeding women should seek medical advice, although many probiotic strains are considered safe during pregnancy.
It is crucial to understand that probiotic supplements are not regulated as medicines in the UK. They are classified as food supplements and do not undergo the same rigorous safety and efficacy testing required for pharmaceutical products. Quality, purity, and accurate labelling can vary significantly between manufacturers. Some products may not contain the bacterial strains or quantities listed on the label. The Food Standards Agency (FSA) oversees food supplement regulation in the UK, with enforcement through local Trading Standards.
Patients taking prescription medications for weight management or diabetes should not replace these treatments with probiotic supplements. If you are considering probiotics alongside existing treatments, discuss this with your GP or specialist to ensure there are no contraindications. Anyone experiencing severe or persistent side effects from probiotic supplements should discontinue use and seek medical advice. Warning signs requiring prompt medical attention include high fever, severe abdominal pain, bloody stools, or signs of allergic reaction. Suspected adverse reactions can be reported through the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
NHS and NICE Guidance on Weight Loss Treatments
The National Institute for Health and Care Excellence (NICE) provides comprehensive, evidence-based guidance on weight management interventions for adults. NICE guidelines emphasise a multicomponent approach focusing on dietary modification, increased physical activity, and behavioural change as the foundation of weight management. These lifestyle interventions should be tailored to individual circumstances and delivered by appropriately trained healthcare professionals.
For individuals with a body mass index (BMI) of 30 kg/m² or above (or 27.5 kg/m² for people from South Asian, Chinese, other Asian, Middle Eastern, Black African, or African-Caribbean backgrounds), NICE recommends considering pharmacological interventions alongside lifestyle changes when dietary and exercise modifications alone have been insufficient. Currently, NICE-approved pharmaceutical options include orlistat (a lipase inhibitor) and, more recently, semaglutide (Wegovy) for specific patient groups meeting eligibility criteria. Orlistat treatment should be continued beyond 12 weeks only if the person has lost at least 5% of their initial body weight.
Semaglutide (Wegovy) is now available through NHS specialist weight management services for adults with at least one weight-related comorbidity and a BMI of 35 kg/m² or above (or 32.5 kg/m² for certain ethnic groups), as recommended in NICE TA875. Treatment is typically limited to a maximum of 2 years. While liraglutide 3 mg (Saxenda) is licensed by the MHRA for weight management, it is not currently recommended by NICE for routine NHS commissioning.
Importantly, NICE guidance does not currently recommend probiotic supplements for weight management or obesity treatment. The evidence base for probiotics in this context does not meet the standards required for inclusion in clinical guidelines. The NHS advises that individuals seeking weight loss should focus on evidence-based approaches, including reducing calorie intake, increasing physical activity, and accessing support through services such as the NHS Weight Loss Plan or local weight management programmes.
Referral pathways for weight management typically begin with your GP, who can assess your overall health, identify any underlying medical conditions contributing to weight gain, and discuss appropriate treatment options. Your GP may refer you to specialist weight management services, dietitians, or, in cases of severe obesity with significant comorbidities, bariatric surgery services. NICE recommends considering bariatric surgery for adults with a BMI of 40 kg/m² or more, or between 35-40 kg/m² with significant obesity-related conditions, with expedited consideration for those with recent-onset type 2 diabetes. If you are considering any supplements or alternative approaches to weight loss, discuss these with your healthcare provider to ensure they do not interfere with evidence-based treatments or pose safety concerns. The most effective and sustainable weight loss occurs through personalised, professionally supported programmes that address diet, physical activity, and behavioural factors rather than relying on supplements with unproven efficacy.
Frequently Asked Questions
Can probiotic supplements increase GLP-1 levels like prescription medications?
No, probiotic supplements cannot replicate the therapeutic GLP-1 increases achieved by licensed pharmaceutical GLP-1 receptor agonists such as semaglutide. Whilst some probiotic strains may theoretically influence endogenous GLP-1 secretion through metabolite production, there is no established evidence that supplements achieve clinically meaningful increases in circulating GLP-1 levels.
Are GLP-1 probiotics recommended by NICE for weight management?
No, NICE guidance does not currently recommend probiotic supplements for weight management or obesity treatment. The evidence base for probiotics in this context does not meet the standards required for inclusion in clinical guidelines, and NICE emphasises multicomponent lifestyle interventions alongside licensed pharmacological options when appropriate.
Who should avoid taking probiotic supplements for weight loss?
Immunocompromised individuals, critically ill patients, those with severe acute pancreatitis, people with central venous catheters, and individuals with short bowel syndrome should avoid probiotics without medical supervision. Pregnant and breastfeeding women should consult their healthcare provider before starting any probiotic supplement.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript