Bloating is one of the most commonly reported side effects of GLP-1 receptor agonists such as semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and liraglutide (Saxenda, Victoza). These medications slow gastric emptying to promote satiety and support weight loss or diabetes management, but this mechanism can cause uncomfortable abdominal distension and gas. Whilst bloating typically improves as your body adjusts to treatment, targeted dietary changes, lifestyle modifications, and appropriate medical guidance can significantly reduce symptoms. Understanding why bloating occurs and implementing evidence-based strategies helps you continue benefiting from GLP-1 therapy whilst maintaining comfort and quality of life. This guide provides practical, clinically informed approaches to managing bloating effectively.
Summary: Bloating on GLP-1 medications can be reduced through dietary modifications (smaller meals, lean proteins, cooked vegetables, avoiding high-fat foods and gas-producing vegetables), lifestyle changes (gentle post-meal walking, eating slowly, adequate hydration), and medical guidance for dose adjustments if symptoms persist.
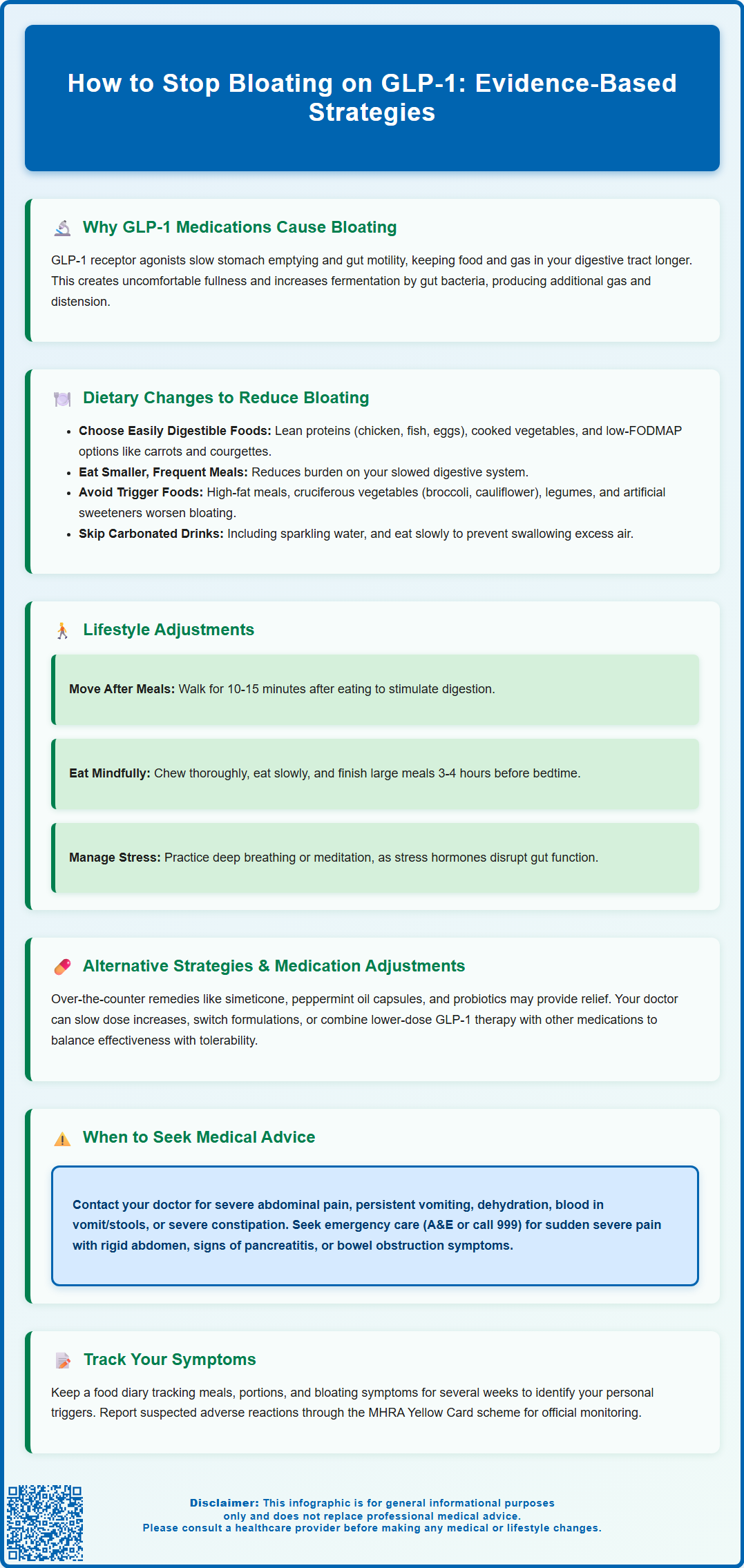
- GLP-1 receptor agonists cause bloating by slowing gastric emptying, which prolongs food transit through the digestive system and increases gas production.
- Prioritise easily digestible foods such as lean proteins, cooked vegetables, and low-FODMAP options whilst avoiding high-fat meals, cruciferous vegetables, legumes, and carbonated drinks.
- Gentle physical activity after meals, eating slowly, staying hydrated with still water, and managing stress can improve gut motility and reduce symptoms.
- Seek medical advice for severe or persistent abdominal pain, vomiting, dehydration, blood in stools, or symptoms suggesting pancreatitis or gallbladder disease.
- Dose titration adjustments, alternative GLP-1 formulations, or over-the-counter remedies like simeticone may help when dietary and lifestyle changes prove insufficient.
Table of Contents
Why GLP-1 Medications Cause Bloating
Glucagon-like peptide-1 (GLP-1) receptor agonists — including semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and liraglutide (Saxenda, Victoza) — are increasingly prescribed for type 2 diabetes management and weight loss. These medications work by mimicking the action of naturally occurring GLP-1, a hormone released from the gut after eating. By binding to GLP-1 receptors in the pancreas, brain, and gastrointestinal tract, they enhance insulin secretion, suppress glucagon release, and promote satiety.
A key mechanism underlying their effectiveness is delayed gastric emptying. GLP-1 receptor agonists slow the rate at which food moves from the stomach into the small intestine, prolonging feelings of fullness and helping to reduce overall calorie intake. However, this same action can lead to gastrointestinal side effects, with abdominal distension (bloating) being a commonly reported complaint. When the stomach empties more slowly, food and gas remain in the digestive tract for longer periods, creating sensations of fullness and discomfort.
Additionally, GLP-1 medications can affect gut motility throughout the entire digestive system, not just the stomach. Slower transit times may contribute to increased fermentation of food by gut bacteria, producing additional gas. The severity of bloating often varies between individuals and may be dose-dependent, typically being more pronounced during the initial weeks of treatment or following dose escalations. Understanding this pharmacological basis helps patients recognise that bloating, whilst uncomfortable, is a predictable consequence of how these medications work rather than an indication of treatment failure. However, persistent or severe symptoms should always be assessed to exclude other causes such as pancreatitis or gallbladder disease.
Dietary Changes to Reduce Bloating on GLP-1
Modifying your dietary habits represents one of the most effective strategies for managing bloating whilst taking GLP-1 medications. Because these drugs slow gastric emptying, choosing foods that are easier to digest can significantly reduce abdominal discomfort.
Foods to prioritise include:
-
Lean proteins such as chicken, turkey, white fish, and eggs, which are generally well-tolerated and less likely to cause gas
-
Cooked vegetables rather than raw ones, as cooking breaks down fibres that can be harder to digest
-
Low-FODMAP options including carrots, courgettes, spinach, and potatoes, which produce less fermentation (note: low-FODMAP diets should be trialled short-term and ideally supervised by a registered dietitian)
-
Smaller, more frequent meals rather than three large meals, reducing the burden on your slowed digestive system (if you also use insulin or sulfonylureas, monitor for hypoglycaemia when changing meal patterns and seek advice from your diabetes team)
-
Adequate hydration with still water throughout the day, avoiding carbonated beverages that introduce additional gas
Foods and habits to limit or avoid:
-
High-fat meals, which take considerably longer to digest and can exacerbate feelings of fullness
-
Cruciferous vegetables (broccoli, cauliflower, Brussels sprouts, cabbage) and legumes (beans, lentils), which are notorious gas producers
-
Artificial sweeteners such as sorbitol and xylitol, commonly found in sugar-free products, which can cause bloating and diarrhoea
-
Carbonated drinks, including sparkling water, which directly introduce gas into the digestive system
-
Eating too quickly, which causes you to swallow excess air
Keeping a food diary for several weeks can help identify specific triggers unique to your digestive system. Note what you eat, portion sizes, and any subsequent bloating symptoms. This personalised approach, ideally reviewed with a dietitian, allows you to make informed adjustments whilst maintaining adequate nutrition during your weight loss or diabetes management journey.
Lifestyle Adjustments to Manage GLP-1 Side Effects
Beyond dietary modifications, several lifestyle strategies can help minimise bloating and improve overall tolerance of GLP-1 medications.
Physical activity plays a crucial role in promoting gut motility. Gentle exercise such as walking for 10-15 minutes after meals can help stimulate digestion and reduce feelings of fullness. Regular physical activity throughout the week — aiming for at least 150 minutes of moderate-intensity exercise as recommended by NHS guidelines — supports overall gastrointestinal function. Yoga poses that involve gentle twisting or forward bends may provide comfort for some people, though these have limited evidence specifically for gas relief. Avoid vigorous exercise immediately after eating.
Eating habits and meal timing deserve careful attention. Chew food thoroughly, taking time to eat slowly and mindfully. This reduces the amount of air swallowed and allows your brain to register satiety signals more effectively. Try to finish your last substantial meal at least 3-4 hours before bedtime, as lying down with a full stomach can worsen bloating and may contribute to acid reflux. Elevating the head of your bed slightly can also help if nighttime symptoms are problematic.
Stress management should not be overlooked, as psychological stress can significantly impact gut function through the gut-brain axis. The digestive system is highly sensitive to stress hormones, which can alter motility patterns and increase visceral sensitivity. Consider incorporating relaxation techniques such as deep breathing exercises, meditation, or progressive muscle relaxation into your daily routine.
Medication timing should follow the specific guidance in your medicine's patient information leaflet. For once-weekly GLP-1 medications, changing the time of day may not materially affect gastrointestinal symptoms. For daily medications, some patients find that administering their injection at different times affects the timing of symptoms. However, never alter your dosing schedule without medical guidance, as consistency is important for glycaemic control and weight management outcomes.
When to Seek Medical Advice About Bloating
Whilst bloating is a common and generally benign side effect of GLP-1 therapy, certain symptoms warrant prompt medical evaluation to rule out more serious complications or conditions requiring intervention.
Contact your GP or diabetes specialist nurse if you experience:
-
Severe or worsening abdominal pain that is persistent, sharp, or different in character from typical bloating discomfort
-
Persistent vomiting or inability to keep down food and fluids, which may indicate gastroparesis (severe delayed gastric emptying) or bowel obstruction
-
Signs of dehydration including dark urine, dizziness, reduced urination, or extreme thirst
-
Unintentional weight loss beyond your treatment goals, or inability to maintain adequate nutrition
-
Blood in vomit or stools, which could indicate gastrointestinal bleeding
-
Severe constipation lasting more than a few days despite usual remedies
-
Symptoms that significantly impair your quality of life or prevent you from carrying out normal daily activities
-
Sudden or persistent right upper abdominal pain (may radiate to the shoulder/back), fever, jaundice, pale stools, or dark urine, which could indicate gallbladder disease
Seek urgent medical attention (A&E or call 999) if you develop:
-
Sudden, severe abdominal pain with a rigid, board-like abdomen
-
Persistent vomiting with inability to keep down any fluids
-
Signs of pancreatitis: severe upper abdominal pain radiating to the back, often with nausea and vomiting
-
Symptoms of bowel obstruction: absolute constipation (no passage of stool or gas), severe cramping, and progressive abdominal distension
For urgent but non-life-threatening concerns, contact NHS 111 for advice.
Your healthcare provider may need to adjust your dose, slow the titration schedule, or consider alternative medications if side effects remain intolerable despite conservative management. Bloating alone is usually not serious, but persistent or severe symptoms should be assessed. Regular follow-up appointments allow monitoring of both therapeutic benefits and adverse effects, ensuring your treatment remains safe and appropriate for your individual circumstances.
If you suspect an adverse reaction to your medication, you can report it via the MHRA Yellow Card scheme at yellowcard.mhra.gov.uk or through the Yellow Card app.
Alternative Strategies and Medication Adjustments
When dietary and lifestyle modifications prove insufficient, additional therapeutic options may help manage bloating whilst continuing GLP-1 therapy.
Over-the-counter remedies can provide symptomatic relief for some patients. Simeticone (such as Wind-Eze or WindSetlers) works by breaking up gas bubbles in the digestive tract, making them easier to pass. Peppermint oil capsules have antispasmodic properties that may reduce bloating and abdominal discomfort, though evidence for their effectiveness specifically in GLP-1-related bloating is limited. They should be used cautiously in patients with gastro-oesophageal reflux disease. Probiotics may help optimise gut microbiome balance, though evidence for their effectiveness specifically in GLP-1-related bloating remains limited. Always speak with your pharmacist about all medications you're taking to check for potential interactions.
Dose titration strategies represent an important consideration. GLP-1 medications are typically started at low doses and gradually increased to minimise gastrointestinal side effects. If bloating is severe, your prescriber might slow this titration schedule, allowing your digestive system more time to adapt at each dose level. Some patients find that remaining at a lower maintenance dose, whilst potentially sacrificing some glycaemic or weight loss benefits, provides an acceptable balance between efficacy and tolerability.
Alternative GLP-1 formulations may be worth discussing. Different GLP-1 receptor agonists have varying pharmacokinetic profiles and receptor binding characteristics. For some patients, switching from a once-weekly to a once-daily formulation (or vice versa) might alter the side effect profile. Newer dual agonists, such as tirzepatide (which targets both GLP-1 and GIP receptors), may have different tolerability profiles, though they can also cause similar gastrointestinal effects. Note that tirzepatide can reduce exposure to oral contraceptives; check the patient information leaflet and consider additional contraception during dose changes.
Combination with other agents might allow dose reduction of the GLP-1 component. In type 2 diabetes management, combining a lower dose of GLP-1 therapy with other glucose-lowering medications (such as metformin or SGLT2 inhibitors) may achieve glycaemic targets whilst reducing side effects. This approach requires careful consideration of your overall treatment goals, other medical conditions, and NICE guidance for your specific situation. Your diabetes care team can help determine whether medication adjustment is appropriate based on your HbA1c levels, weight loss progress, and quality of life considerations.
Frequently Asked Questions
Why do GLP-1 medications like Ozempic cause bloating?
GLP-1 receptor agonists slow gastric emptying, meaning food remains in the stomach and digestive tract for longer periods. This delayed transit increases gas production through bacterial fermentation and creates sensations of fullness and abdominal distension.
What foods should I avoid to reduce bloating on GLP-1 medications?
Avoid high-fat meals, cruciferous vegetables (broccoli, cauliflower, cabbage), legumes (beans, lentils), artificial sweeteners (sorbitol, xylitol), and carbonated drinks, as these are harder to digest or produce excess gas when gastric emptying is slowed.
When should I contact my doctor about bloating on GLP-1 therapy?
Seek medical advice if you experience severe or worsening abdominal pain, persistent vomiting, signs of dehydration, blood in vomit or stools, severe constipation, or symptoms suggesting pancreatitis (severe upper abdominal pain radiating to the back). Seek urgent care (A&E or 999) for sudden severe pain with a rigid abdomen or signs of bowel obstruction.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript










