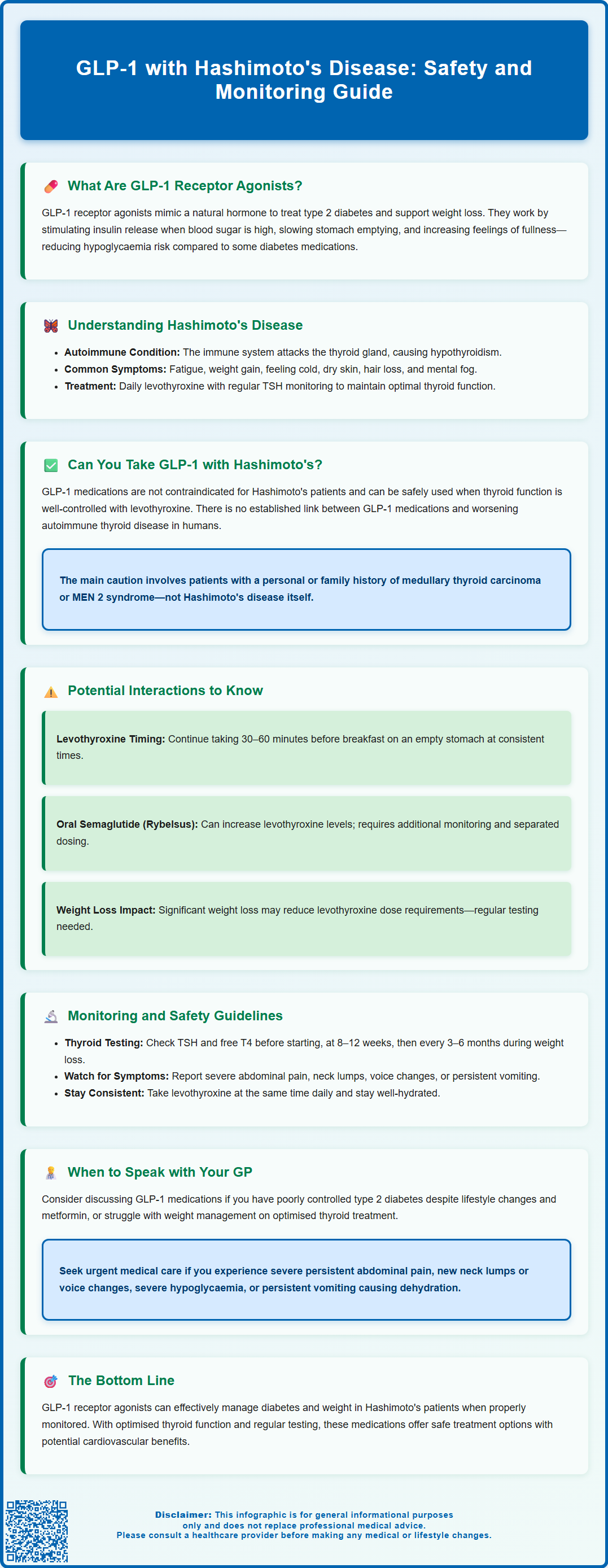
GLP-1 receptor agonists, such as semaglutide and liraglutide, are increasingly prescribed for type 2 diabetes and weight management in the UK. For patients with Hashimoto's disease—the most common cause of hypothyroidism—questions often arise about the safety and appropriateness of combining these treatments. Whilst there is no absolute contraindication to using GLP-1 medications alongside thyroid hormone replacement, several important considerations regarding monitoring, potential interactions, and thyroid safety require careful attention. This article examines the evidence and practical guidance for patients with Hashimoto's thyroiditis considering or currently taking GLP-1 receptor agonists.
Summary: GLP-1 receptor agonists can generally be used safely in patients with Hashimoto's disease when thyroid function is well-controlled with levothyroxine and appropriate monitoring is in place.
- GLP-1 receptor agonists are medications that enhance insulin secretion, suppress glucagon, and promote weight loss, primarily used for type 2 diabetes and obesity management.
- There is no absolute contraindication to combining GLP-1 medications with Hashimoto's disease, provided hypothyroidism is adequately managed with levothyroxine replacement.
- Oral semaglutide (Rybelsus) can increase levothyroxine exposure and requires additional thyroid function monitoring and dose separation.
- Significant weight loss from GLP-1 therapy may reduce levothyroxine requirements, necessitating regular thyroid function testing every 3–6 months during active weight loss.
- UK product information contains warnings about thyroid C-cell tumours based on animal studies, though clinical relevance to humans remains uncertain and Hashimoto's disease itself is not a contraindication.
- Patients should report new neck swelling, voice changes, or symptoms of thyroid dysfunction to their GP whilst taking GLP-1 medications.
Table of Contents
- What Are GLP-1 Receptor Agonists and How Do They Work?
- Understanding Hashimoto's Disease and Thyroid Function
- Can You Take GLP-1 Medications with Hashimoto's Disease?
- Potential Interactions Between GLP-1 Drugs and Thyroid Conditions
- Monitoring and Safety Considerations for Hashimoto's Patients
- When to Speak with Your GP About GLP-1 Treatment
- Frequently Asked Questions
What Are GLP-1 Receptor Agonists and How Do They Work?
GLP-1 receptor agonists are a class of medications that mimic the action of glucagon-like peptide-1, a naturally occurring hormone in the body. These drugs are primarily prescribed for the management of type 2 diabetes mellitus and, more recently, for weight management in adults with obesity or overweight with weight-related comorbidities. Common examples available in the UK include semaglutide (Ozempic, Wegovy, Rybelsus), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda).
The mechanism of action centres on several key physiological effects. GLP-1 receptor agonists enhance glucose-dependent insulin secretion from pancreatic beta cells, meaning they stimulate insulin release only when blood glucose levels are elevated. This reduces the risk of hypoglycaemia compared with some other diabetes medications. Additionally, they suppress glucagon secretion, slow gastric emptying, and promote satiety through central nervous system pathways, which collectively improve glycaemic control and facilitate weight loss.
These medications are administered via subcutaneous injection, with dosing frequencies ranging from once daily to once weekly depending on the specific agent. Oral semaglutide (Rybelsus) is also available as a tablet. In the UK, NICE recommends GLP-1 receptor agonists for type 2 diabetes under specific circumstances, typically when metformin and other treatments have not achieved glycaemic targets, or in people with specific cardiovascular risk factors. For weight management, NICE restricts their use to specialist weight management services with specific BMI thresholds and stopping rules.
Common adverse effects include gastrointestinal symptoms such as nausea, vomiting, diarrhoea, and constipation, which typically diminish over time. More serious but rare complications include pancreatitis and, in animal studies, thyroid C-cell tumours, though the clinical relevance to humans remains under investigation. GLP-1 receptor agonists are not indicated for type 1 diabetes. Understanding how these medications work is essential when considering their use alongside other chronic conditions such as Hashimoto's disease.
Understanding Hashimoto's Disease and Thyroid Function
Hashimoto's thyroiditis, also known as chronic lymphocytic thyroiditis, is the most common cause of hypothyroidism in the UK and other iodine-sufficient regions. This autoimmune condition occurs when the body's immune system mistakenly attacks the thyroid gland, leading to chronic inflammation and progressive destruction of thyroid tissue. Over time, this results in reduced production of thyroid hormones—primarily thyroxine (T4) and triiodothyronine (T3)—which are essential for regulating metabolism, energy production, and numerous bodily functions.
The condition predominantly affects women, with a female-to-male ratio of approximately 10:1, and typically presents in middle age, though it can occur at any age. Patients with Hashimoto's disease often have detectable thyroid autoantibodies in their blood, particularly anti-thyroid peroxidase (anti-TPO) antibodies and, less commonly, anti-thyroglobulin antibodies. These markers help confirm the autoimmune nature of the condition.
Clinical manifestations of hypothyroidism secondary to Hashimoto's disease include:
-
Fatigue and lethargy
-
Weight gain despite normal appetite
-
Cold intolerance
-
Dry skin and hair loss
-
Constipation
-
Depression and cognitive impairment
-
Bradycardia and elevated cholesterol
Diagnosis is established through thyroid function tests showing elevated thyroid-stimulating hormone (TSH) with low free T4 (overt hypothyroidism) or normal free T4 (subclinical hypothyroidism), alongside positive thyroid antibodies. The mainstay of treatment is levothyroxine replacement therapy, which aims to restore normal thyroid hormone levels. Regular monitoring of TSH levels is essential to ensure optimal dosing, with annual review typically recommended once stable. Many patients with Hashimoto's disease also experience other autoimmune conditions, metabolic syndrome, or weight management challenges, which may prompt consideration of additional therapies such as GLP-1 receptor agonists.
Can You Take GLP-1 Medications with Hashimoto's Disease?
There is no absolute contraindication to using GLP-1 receptor agonists in patients with Hashimoto's disease or established hypothyroidism. Many individuals with Hashimoto's thyroiditis also have type 2 diabetes or obesity—conditions for which GLP-1 medications are indicated—and can safely receive these treatments under appropriate medical supervision. As good clinical practice, ensuring that thyroid function is adequately controlled with levothyroxine before initiating additional therapies is advisable.
Patients with well-managed hypothyroidism on stable levothyroxine replacement can generally proceed with GLP-1 therapy if clinically indicated. The primary concern relates not to direct drug interactions between most injectable GLP-1 agonists and levothyroxine, but rather to the potential impact on thyroid monitoring and the theoretical risk associated with thyroid C-cell tumours observed in animal studies. It is important to note that there is no established link between GLP-1 receptor agonists and worsening of autoimmune thyroid disease in humans.
UK product information for GLP-1 receptor agonists contains special warnings and precautions regarding thyroid C-cell tumours (medullary thyroid carcinoma) based on rodent studies. Whilst this has not been conclusively demonstrated in humans, caution is advised in patients with a personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2 (MEN 2). Hashimoto's disease itself does not fall into these categories, but patients should be counselled about this theoretical risk.
For women of childbearing potential, it's important to note that GLP-1 receptor agonists are generally not recommended during pregnancy. For weight management medications like Wegovy, discontinuation at least two months before a planned pregnancy is advised.
Before starting GLP-1 therapy, your healthcare provider will:
-
Review your complete medical history, including thyroid disease status
-
Ensure thyroid function is optimised
-
Assess for any contraindications
-
Discuss the benefits and risks specific to your situation
With appropriate patient selection and monitoring, GLP-1 receptor agonists can be safely prescribed to individuals with Hashimoto's disease when the clinical benefits outweigh potential risks.
Potential Interactions Between GLP-1 Drugs and Thyroid Conditions
Understanding potential interactions between GLP-1 receptor agonists and thyroid conditions requires consideration of both pharmacological mechanisms and clinical monitoring implications. While injectable GLP-1 medications generally have no direct pharmacokinetic interaction with levothyroxine, there are important considerations regarding oral semaglutide and indirect effects that warrant attention.
Gastric emptying and levothyroxine absorption: GLP-1 receptor agonists significantly slow gastric emptying, which is part of their therapeutic mechanism. Levothyroxine is optimally absorbed in the small intestine on an empty stomach. Delayed gastric emptying could affect the timing and extent of levothyroxine absorption. To minimise any potential effect, patients should continue taking levothyroxine as directed—typically 30–60 minutes before breakfast on an empty stomach—and maintain consistent timing.
Oral semaglutide (Rybelsus) interaction: Unlike injectable GLP-1 agonists, oral semaglutide has a documented interaction with levothyroxine. The Rybelsus Summary of Product Characteristics notes that it can increase levothyroxine exposure. If you take both medications, your healthcare provider may recommend additional thyroid function monitoring and separation of dosing times.
Weight loss and thyroid hormone requirements: Substantial weight loss achieved through GLP-1 therapy may alter thyroid hormone requirements. As body weight decreases, the dose of levothyroxine needed to maintain euthyroidism may also decrease. This necessitates regular monitoring of thyroid function during active weight loss phases to avoid overtreatment, which can cause symptoms of hyperthyroidism including palpitations, anxiety, and bone loss.
Thyroid C-cell concerns: UK product information contains special warnings and precautions regarding thyroid C-cell tumours. Animal studies demonstrated dose-dependent and treatment-duration-dependent increases in thyroid C-cell tumours in rodents treated with GLP-1 receptor agonists. The relevance to humans remains uncertain, as human thyroid C-cells express far fewer GLP-1 receptors than rodent C-cells. Clinical vigilance is advised, particularly for symptoms such as a neck mass, dysphagia, or persistent hoarseness.
Autoimmune considerations: There is no evidence that GLP-1 receptor agonists worsen autoimmune thyroid disease or trigger new-onset Hashimoto's thyroiditis. The autoimmune process in Hashimoto's disease is distinct from the mechanisms affected by GLP-1 therapy, and no causal relationship has been established in clinical studies or post-marketing surveillance.
Monitoring and Safety Considerations for Hashimoto's Patients
Patients with Hashimoto's disease who are prescribed GLP-1 receptor agonists require a structured monitoring approach to ensure both conditions are optimally managed and to detect any potential complications early. This collaborative care typically involves both your GP and, where appropriate, endocrinology services.
Thyroid function monitoring should be intensified during the initial phases of GLP-1 treatment and during periods of significant weight loss. Standard practice includes:
-
Baseline thyroid function tests (TSH and free T4) before initiating GLP-1 therapy
-
Repeat testing at 8–12 weeks after starting treatment or after dose escalation
-
Regular monitoring every 3–6 months during active weight loss
-
Return to annual monitoring once weight is stable and thyroid function remains consistent
Adjustments to levothyroxine dosing may be necessary as weight changes. Your healthcare provider will interpret TSH levels in the context of your symptoms and weight trajectory, aiming to maintain TSH within your local laboratory's reference range.
Safety monitoring for GLP-1 therapy itself includes:
-
Assessment for gastrointestinal adverse effects, which are common but usually transient
-
Monitoring for signs of pancreatitis (severe, persistent abdominal pain)
-
Vigilance for symptoms suggesting thyroid masses (neck lump, difficulty swallowing, persistent hoarseness)
-
Regular review of glycaemic control in diabetic patients
-
Blood pressure and cardiovascular risk factor assessment
-
Monitoring for gallbladder disease (right upper abdominal pain, fever, jaundice)
-
Eye examinations for people with diabetes, particularly those with pre-existing diabetic retinopathy
-
Renal function checks, especially if experiencing severe gastrointestinal symptoms that could lead to dehydration
If you have diabetes and take insulin or sulfonylureas, your doctor may reduce these doses when starting GLP-1 therapy to prevent hypoglycaemia.
Patient self-monitoring is equally important. You should be advised to:
-
Report any new neck swelling or changes in voice
-
Monitor for symptoms of thyroid dysfunction (either hypo- or hyperthyroidism)
-
Maintain consistent timing of levothyroxine administration
-
Keep a record of weight changes
-
Report severe or persistent gastrointestinal symptoms
-
Stay well-hydrated, especially if experiencing nausea, vomiting or diarrhoea
Medication adherence to both levothyroxine and GLP-1 therapy is essential for optimal outcomes. Some patients find the injection-based administration of GLP-1 medications challenging initially, but most adapt well with proper education and support. Your healthcare team can provide training and address any concerns about injection technique or side effect management.
If you experience any suspected side effects, you can report them through the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
When to Speak with Your GP About GLP-1 Treatment
Knowing when to initiate a conversation with your GP about GLP-1 receptor agonists is important for patients with Hashimoto's disease who may benefit from these medications. Several clinical scenarios warrant discussion:
You should consider speaking with your GP if:
-
You have type 2 diabetes that is inadequately controlled despite lifestyle modifications and metformin therapy, and your HbA1c remains above target
-
You are struggling with weight management despite optimised thyroid hormone replacement, and you might meet NICE criteria for medical weight management (typically requiring referral to specialist weight management services)
-
You have cardiovascular disease alongside type 2 diabetes, as some GLP-1 agonists (semaglutide, liraglutide, dulaglutide) have demonstrated cardiovascular benefits
-
Your current diabetes medications are causing problematic side effects or hypoglycaemia
Before your appointment, it is helpful to:
-
Ensure your thyroid function has been checked recently (within the past 6 months)
-
Compile a list of all current medications, including levothyroxine dose and timing
-
Document your weight history and any previous weight management attempts
-
Note any family history of thyroid cancer or endocrine conditions
-
Prepare questions about potential benefits, risks, and alternatives
Your GP will assess your suitability for GLP-1 therapy by reviewing your medical history, current thyroid status, diabetes control (if applicable), and overall health. For weight management, be aware that in the UK, GLP-1 medications like Wegovy (semaglutide) and Saxenda (liraglutide) are typically only available through specialist weight management services (tier 3 or 4), with specific BMI thresholds and time-limited treatment courses as per NICE guidance.
Seek urgent medical advice if you are already taking a GLP-1 medication and experience:
-
Severe, persistent abdominal pain (possible pancreatitis)
-
A new lump in your neck or changes in your voice
-
Symptoms of severe hypoglycaemia (if taking other diabetes medications)
-
Signs of thyroid dysfunction despite stable levothyroxine therapy
-
Persistent vomiting leading to dehydration or inability to take oral medications
-
Severe right upper abdominal pain, fever or jaundice (possible gallbladder disease)
Open communication with your healthcare team ensures that treatment decisions are individualised, evidence-based, and aligned with your health priorities. GLP-1 receptor agonists can be valuable tools for managing diabetes and weight in patients with Hashimoto's disease when used appropriately and with proper monitoring.
Frequently Asked Questions
Can I take GLP-1 medications if I have Hashimoto's disease?
Yes, there is no absolute contraindication to using GLP-1 receptor agonists with Hashimoto's disease. Provided your hypothyroidism is well-controlled with levothyroxine and you receive appropriate monitoring, GLP-1 medications can be safely prescribed when clinically indicated for type 2 diabetes or weight management.
Do GLP-1 medications interact with levothyroxine?
Injectable GLP-1 medications generally have no direct interaction with levothyroxine, though delayed gastric emptying may affect absorption timing. Oral semaglutide (Rybelsus) can increase levothyroxine exposure and requires additional thyroid monitoring and dose separation.
How often should thyroid function be monitored when taking GLP-1 medications?
Thyroid function tests should be performed at baseline, repeated at 8–12 weeks after starting GLP-1 therapy, then every 3–6 months during active weight loss. Once weight stabilises and thyroid function remains consistent, monitoring can return to annual reviews.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript