GLP-1 receptor agonists, such as semaglutide and liraglutide, are increasingly prescribed for type 2 diabetes and weight management. However, if you have Crohn's disease, you may wonder whether these medications are safe and appropriate for you. Crohn's disease is a chronic inflammatory bowel condition that can cause abdominal pain, diarrhoea, and weight loss. GLP-1 medications commonly cause gastrointestinal side effects, which may overlap with or worsen Crohn's symptoms. This article explores the use of GLP-1 with Crohn's disease, examining current evidence, potential risks, and the importance of individualised clinical decision-making in collaboration with your healthcare team.
Summary: GLP-1 receptor agonists are not specifically contraindicated in Crohn's disease, but their use requires careful individualised assessment due to potential gastrointestinal side effects and disease-specific considerations.
- GLP-1 receptor agonists enhance insulin secretion, suppress glucagon, slow gastric emptying, and reduce appetite.
- Common gastrointestinal side effects include nausea, vomiting, diarrhoea, constipation, and abdominal pain, which may overlap with Crohn's symptoms.
- Caution is advised in active or severe gastrointestinal disease, strictures, malnutrition, or bowel obstruction risk.
- Clinical decisions should involve gastroenterology and diabetes specialists, with close monitoring of disease activity and nutritional status.
- Emerging research suggests GLP-1 use in stable IBD may not significantly increase disease activity, but robust evidence remains limited.
Table of Contents
What Are GLP-1 Medications and How Do They Work?
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications originally developed for managing type 2 diabetes. Some have also been approved for weight management in adults with obesity or overweight with weight-related comorbidities. These medicines include:
-
Semaglutide (Ozempic, Rybelsus – for diabetes; Wegovy – for weight management)
-
Liraglutide (Victoza – for diabetes; Saxenda – for weight management)
-
Dulaglutide (Trulicity – for diabetes only)
-
Tirzepatide (Mounjaro) – a dual glucose-dependent insulinotropic polypeptide (GIP) and GLP-1 receptor agonist, with distinct pharmacology from pure GLP-1 agonists
These medications work by mimicking the action of naturally occurring hormones that regulate blood glucose and appetite. The primary mechanisms of action include:
-
Enhancing insulin secretion from the pancreas in response to elevated blood glucose levels, which helps lower blood sugar
-
Suppressing glucagon release, a hormone that raises blood glucose
-
Slowing gastric emptying, which means food moves more slowly from the stomach into the small intestine
-
Reducing appetite through effects on brain centres that regulate hunger and satiety
These combined effects make GLP-1 receptor agonists effective for glycaemic control in type 2 diabetes and, for those specifically licensed for weight management, achieving significant weight loss. Most formulations are administered via subcutaneous injection, either daily or weekly, though oral semaglutide (Rybelsus) is also available for diabetes treatment.
The Medicines and Healthcare products Regulatory Agency (MHRA) has approved these medications for specific indications, and NICE provides guidance on their use within the NHS. Importantly, these medications are not generally recommended in patients with severe gastrointestinal disease, including severe gastroparesis, which may be relevant when considering their use in individuals with Crohn's disease.
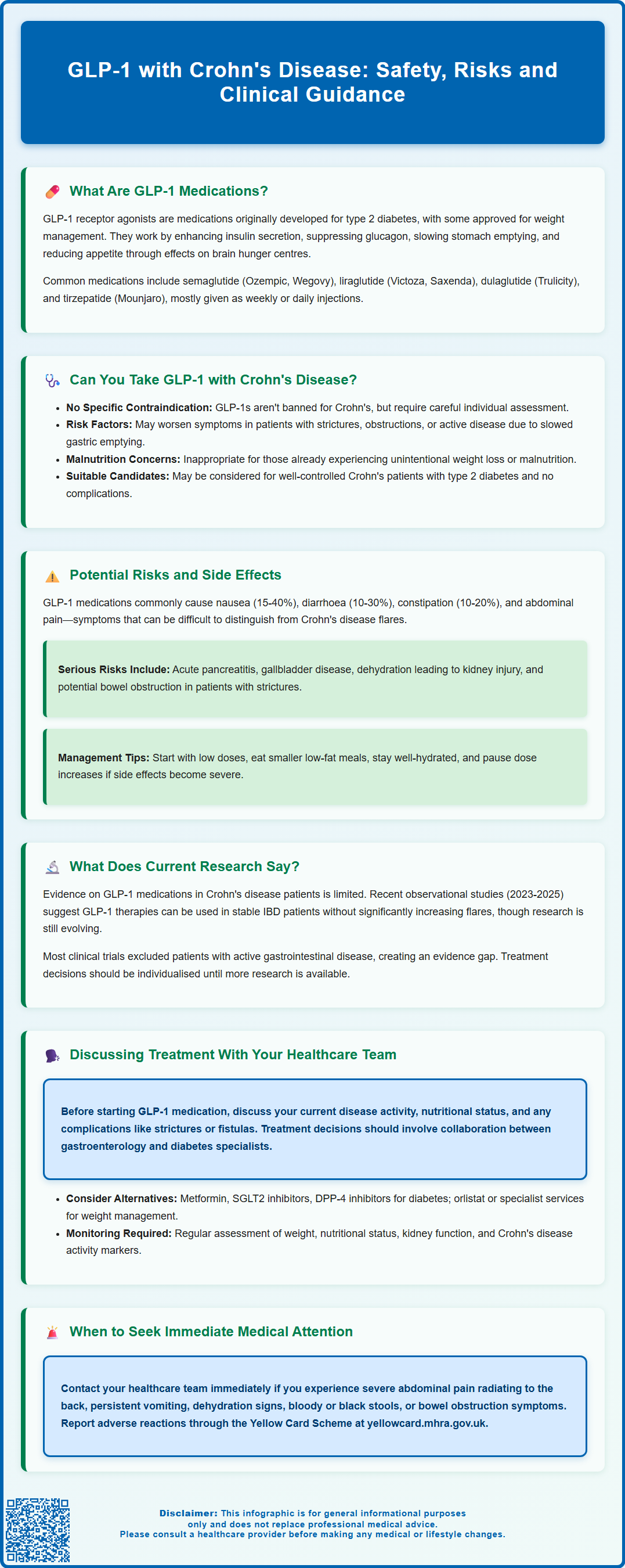
Can You Take GLP-1 Medications If You Have Crohn's Disease?
There is currently no specific contraindication to using GLP-1 receptor agonists in people with Crohn's disease, but this decision requires careful individualised assessment. Crohn's disease is a chronic inflammatory bowel disease (IBD) that can affect any part of the gastrointestinal tract, causing symptoms such as abdominal pain, diarrhoea, weight loss, and fatigue. The condition is characterised by periods of active inflammation (flares) and remission.
While the prescribing information for GLP-1 medications does not specifically list Crohn's disease as a contraindication, the Summary of Product Characteristics (SmPC) for these medicines does advise caution in patients with gastrointestinal disease and states they are not recommended in severe gastrointestinal disease. Several important considerations apply:
-
Individuals with active or severe gastrointestinal disease may experience worsening symptoms due to the gastrointestinal side effects of GLP-1 medications
-
The slowed gastric emptying caused by these drugs could theoretically exacerbate symptoms in people with strictures or obstructive complications of Crohn's disease
-
Weight loss associated with GLP-1 therapy may be inappropriate in patients with Crohn's disease who are already experiencing malnutrition or unintentional weight loss
-
The interaction between GLP-1 medications and the inflammatory processes in IBD is not fully understood
Clinical decision-making should involve a thorough assessment of disease activity, nutritional status, presence of complications (such as strictures or fistulas), and the primary indication for GLP-1 therapy. If the medication is being considered for type 2 diabetes management in someone with well-controlled Crohn's disease and no significant gastrointestinal complications, it may be appropriate. However, if considered for weight management in someone with active Crohn's disease or malnutrition, alternative approaches would typically be preferred.
It's also important to note that GLP-1 medications are not recommended during pregnancy or breastfeeding, and women of childbearing potential should follow product-specific advice regarding discontinuation before planned pregnancy. Close collaboration between gastroenterology and endocrinology or diabetes specialists is advisable.
Potential Risks and Gastrointestinal Side Effects
Gastrointestinal side effects are the most commonly reported adverse reactions with GLP-1 receptor agonists, occurring in a significant proportion of patients, particularly during treatment initiation and dose escalation. For individuals with Crohn's disease, these effects warrant particular attention as they may overlap with or exacerbate existing symptoms.
Common gastrointestinal side effects include:
-
Nausea and vomiting (affecting 15–40% of patients, depending on the specific medication and dose)
-
Diarrhoea (reported in 10–30% of patients)
-
Constipation (affecting 10–20% of patients)
-
Abdominal pain and discomfort
-
Reduced appetite and early satiety
-
Dyspepsia and gastro-oesophageal reflux symptoms
These effects are generally dose-dependent and tend to improve over time as the body adjusts to the medication. However, in people with Crohn's disease, distinguishing between medication side effects and disease flares can be challenging. Diarrhoea and abdominal pain, for instance, are cardinal symptoms of active Crohn's disease, and their worsening could indicate either a drug side effect or disease progression.
More serious concerns include:
-
Acute pancreatitis: If severe, persistent abdominal pain occurs, possibly radiating to the back, with or without vomiting, treatment should be discontinued immediately and urgent medical attention sought
-
Gallbladder disease: GLP-1 medications and weight loss can increase the risk of gallstones and cholecystitis. People with Crohn's disease, especially those with ileal involvement, may already have a higher baseline risk of gallstone formation
-
Dehydration and acute kidney injury: Persistent vomiting or diarrhoea can lead to dehydration, particularly in vulnerable patients
-
Bowel obstruction: For individuals with Crohn's disease, especially those with known strictures, the risk of obstruction may theoretically be increased due to the medication's effect on gastrointestinal motility
Practical strategies to minimise side effects include:
-
Starting with a low dose and gradually increasing as tolerated
-
Eating smaller, lower-fat meals and avoiding overeating
-
Maintaining adequate hydration
-
Temporarily pausing dose escalation if symptoms become intolerable
Patients should be advised to contact their GP or specialist immediately if they experience:
-
Severe, persistent abdominal pain (especially if radiating to the back)
-
Persistent vomiting preventing adequate fluid intake
-
Signs of dehydration
-
Blood in stools or black, tarry stools
-
Symptoms suggesting bowel obstruction (severe cramping, inability to pass stool or gas, abdominal distension)
Suspected adverse reactions should be reported via the Yellow Card Scheme (yellowcard.mhra.gov.uk or the Yellow Card app).
What Does Current Research Say About GLP-1 and IBD?
The evidence base regarding GLP-1 receptor agonists in patients with inflammatory bowel disease, including Crohn's disease, remains limited but is an area of growing research interest. While there is no established link between GLP-1 medications and worsening of Crohn's disease, the data to definitively confirm their safety in this population is still evolving.
Some emerging research has explored potential connections between GLP-1 signalling and intestinal inflammation. GLP-2, a related peptide from the same proglucagon precursor, has known intestinotrophic effects and has been studied for its potential to promote intestinal healing in short bowel syndrome. Some experimental studies have suggested that GLP-1 receptors are expressed in the gastrointestinal tract and may have anti-inflammatory properties, though this research is preliminary and has not been translated into clinical practice.
Recent observational studies examining GLP-1 use in patients with IBD have generally not shown a clear increase in IBD exacerbations or flares. Registry and cohort analyses from 2023-2025 suggest that GLP-1 therapies may be used in stable IBD without significantly increasing disease activity, though these studies have important limitations. It's worth noting that most clinical trials of GLP-1 medications excluded patients with significant active gastrointestinal disease, creating an evidence gap for those with severe or poorly controlled IBD.
Current NICE guidance on GLP-1 receptor agonists for diabetes and obesity does not specifically address their use in people with Crohn's disease or other forms of IBD. The absence of specific guidance reflects the lack of robust clinical trial data in this population.
Further research, including prospective studies and registry data, is needed to better understand the safety profile, potential benefits, and risks of GLP-1 therapy in individuals with Crohn's disease. Until more definitive evidence becomes available, clinical decisions must be made on an individual basis, weighing the potential benefits against theoretical and observed risks.
Discussing GLP-1 Treatment Options With Your Healthcare Team
If you have Crohn's disease and are considering GLP-1 medication—whether for type 2 diabetes management or weight loss—it is essential to have an open, detailed conversation with your healthcare team. This discussion should involve your GP, gastroenterologist, and potentially an endocrinologist or diabetes specialist, ensuring a coordinated approach to your care.
Key points to discuss with your healthcare team include:
-
Current disease activity: Is your Crohn's disease well-controlled or are you experiencing active symptoms? The presence of active inflammation, frequent flares, or recent changes in your condition may influence the decision
-
Nutritional status: Have you experienced unintentional weight loss? Are you at risk of malnutrition? GLP-1 medications typically cause weight loss, which may not be appropriate if you are already underweight or nutritionally compromised
-
Gastrointestinal complications: Do you have strictures, fistulas, or a history of bowel obstruction? These complications may increase the risk of adverse effects from medications that slow gastrointestinal motility
-
Primary indication: Is the GLP-1 medication being considered for diabetes control or weight management? The risk-benefit balance may differ depending on the indication and availability of alternative treatments
-
Monitoring plan: What symptoms should you watch for? How will your team distinguish between medication side effects and Crohn's disease activity? What is the plan for follow-up?
Your healthcare team should also consider alternative treatment options. For type 2 diabetes, other medication classes such as metformin, SGLT2 inhibitors, or DPP-4 inhibitors may be appropriate alternatives. For weight management, NICE provides guidance on eligibility for specialist weight management services, which may include other pharmacological options such as orlistat (though this can also cause gastrointestinal side effects that may be problematic in IBD).
If GLP-1 therapy is initiated, a structured monitoring plan should include:
-
Regular assessment of weight, BMI and nutritional status
-
Monitoring of hydration and renal function, particularly if experiencing significant gastrointestinal symptoms
-
For diabetes patients, appropriate retinopathy surveillance if glycaemic control improves rapidly (especially with semaglutide)
-
Regular review of Crohn's disease activity using clinical and biochemical markers
Remember that you are an active participant in your healthcare decisions, and your concerns and experiences should guide the treatment plan. If you experience any concerning symptoms, contact your healthcare team promptly rather than waiting for your next scheduled appointment.
Frequently Asked Questions
Are GLP-1 medications contraindicated in Crohn's disease?
No, GLP-1 receptor agonists are not specifically contraindicated in Crohn's disease, but caution is advised in patients with active or severe gastrointestinal disease. Individualised assessment by gastroenterology and diabetes specialists is essential.
What gastrointestinal side effects should Crohn's patients watch for with GLP-1 medications?
Common side effects include nausea, vomiting, diarrhoea, constipation, and abdominal pain. Patients should seek urgent medical attention for severe persistent abdominal pain, persistent vomiting, dehydration, blood in stools, or signs of bowel obstruction.
Should I discuss my Crohn's disease with my doctor before starting GLP-1 therapy?
Yes, it is essential to discuss your Crohn's disease activity, nutritional status, gastrointestinal complications, and treatment goals with your GP, gastroenterologist, and diabetes specialist before starting GLP-1 therapy to ensure a coordinated, safe approach.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












