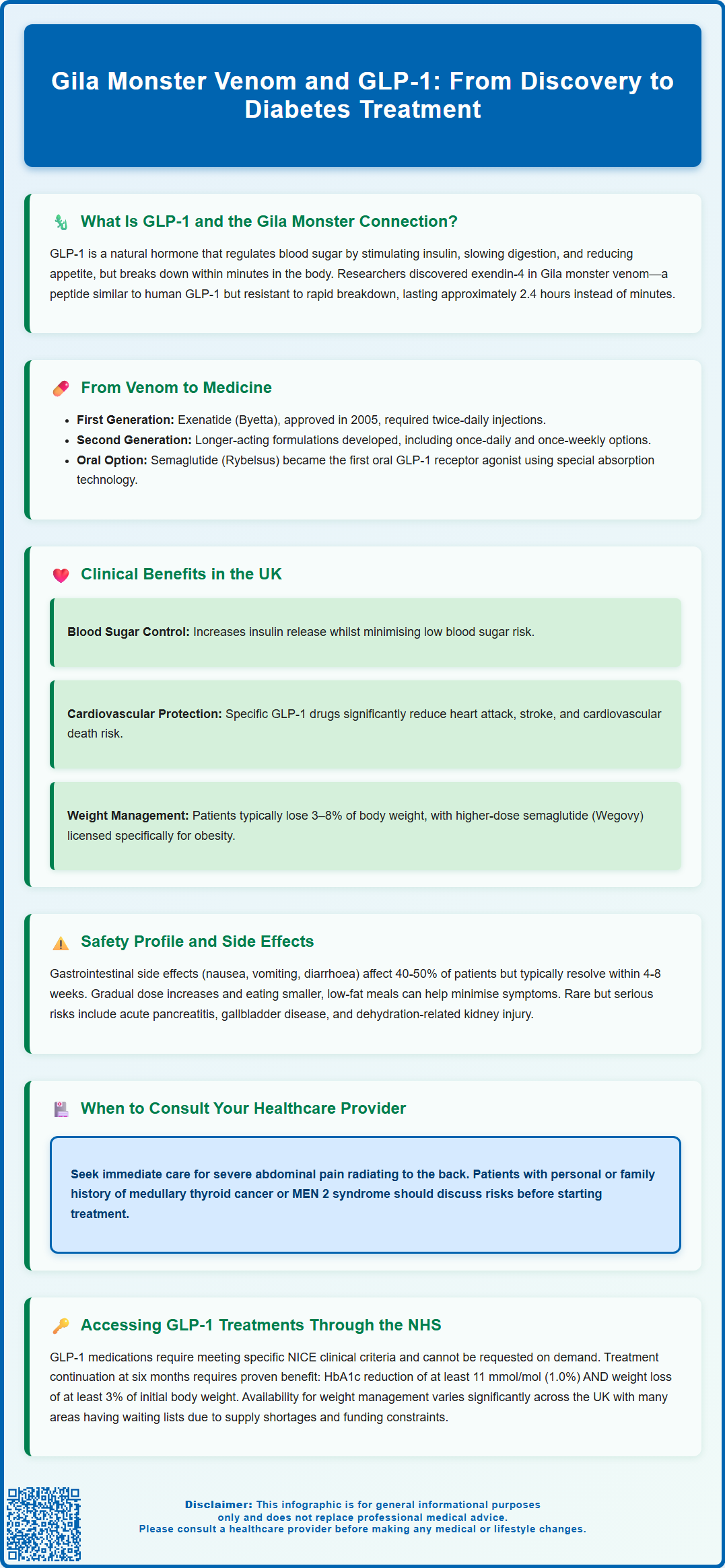
Gila monster venom and GLP-1 share a remarkable connection that revolutionised diabetes treatment. In the 1990s, researchers discovered exendin-4, a peptide in Gila monster venom structurally similar to human glucagon-like peptide-1 (GLP-1), a hormone that regulates blood glucose. Unlike natural GLP-1, which breaks down within minutes, exendin-4 resists enzymatic degradation, offering prolonged glucose-lowering effects. This discovery led to the development of exenatide, the first GLP-1 receptor agonist approved for type 2 diabetes in 2005. Today, GLP-1 medications derived from this venom peptide are cornerstone therapies in UK diabetes care, prescribed according to NICE guidance for glycaemic control, cardiovascular protection, and weight management.
Summary: Gila monster venom contains exendin-4, a peptide that mimics human GLP-1 but resists rapid breakdown, leading to the development of long-acting GLP-1 receptor agonists now used to treat type 2 diabetes.
- Exendin-4 from Gila monster venom shares structural similarities with human GLP-1 but has a significantly longer duration of action due to resistance to DPP-4 enzyme breakdown.
- The first GLP-1 receptor agonist, exenatide, was approved in 2005 and has since led to multiple formulations including once-weekly injectables and oral semaglutide.
- NICE recommends GLP-1 receptor agonists for type 2 diabetes when triple oral therapy fails or in specific BMI and comorbidity contexts, with six-month review required.
- Certain GLP-1 agents reduce major cardiovascular events including myocardial infarction and stroke in patients with established cardiovascular disease.
- Common side effects include gastrointestinal symptoms (nausea, vomiting, diarrhoea); rare serious risks include acute pancreatitis and gallbladder disease requiring clinical monitoring.
- NHS access requires meeting NICE eligibility criteria, specialist or enhanced GP assessment, and demonstration of metabolic response (HbA1c reduction ≥11 mmol/mol and ≥3% weight loss) at six months.
Table of Contents
What Is GLP-1 and How Was It Discovered in Gila Monster Venom?
Glucagon-like peptide-1 (GLP-1) is a naturally occurring hormone produced in the human intestine that plays a crucial role in regulating blood glucose levels. When we eat, GLP-1 is released and stimulates insulin secretion from the pancreas, slows gastric emptying, and reduces appetite. However, natural human GLP-1 has a very short half-life—it is rapidly broken down by an enzyme called dipeptidyl peptidase-4 (DPP-4), lasting only a few minutes in the bloodstream.
The remarkable connection between Gila monster venom and modern diabetes treatment began in the 1990s when researchers at the Veterans Affairs Medical Centre in New York were studying the venom of the Gila monster (Heloderma suspectum), a venomous lizard native to the southwestern United States and Mexico. Dr John Eng and his colleagues discovered a peptide in the venom called exendin-4, which shared structural similarities with human GLP-1 but possessed a crucial advantage: it was resistant to breakdown by DPP-4.
Exendin-4 demonstrated the ability to bind to the same receptors as human GLP-1, producing similar glucose-lowering effects, but with a significantly longer duration of action. When developed into the synthetic medication exenatide, it showed a human half-life of approximately 2.4 hours compared to the minutes-long activity of native GLP-1. This discovery was groundbreaking because it suggested that a modified version of this venom peptide could potentially be developed into a therapeutic agent for type 2 diabetes. The Gila monster, which feeds infrequently and can survive for months without food, may use similar metabolic mechanisms, though the precise role of exendin-4 in the lizard's own physiology continues to be studied.
How Gila Monster Venom Led to Modern Diabetes Medications
The translation of Gila monster venom research into clinical medicine represents one of the most successful examples of biomimicry in pharmaceutical development. Following the discovery of exendin-4, pharmaceutical companies recognised the therapeutic potential and began developing synthetic versions of this peptide for human use.
In 2005, the first GLP-1 receptor agonist, exenatide (marketed as Byetta), was approved by the US Food and Drug Administration and subsequently received European authorisation through the European Medicines Agency (EMA). The Medicines and Healthcare products Regulatory Agency (MHRA) now maintains the UK licence for this medication. Exenatide required twice-daily injections and represented a novel approach to treating type 2 diabetes by harnessing the body's natural glucose regulation mechanisms.
The success of exenatide paved the way for the development of second-generation GLP-1 receptor agonists with improved pharmacological properties. Researchers modified the original peptide structure to create longer-acting formulations with various strategies: liraglutide (once daily) uses fatty acid albumin-binding, dulaglutide (once weekly) employs an Fc-fusion approach, exenatide extended-release (Bydureon, once weekly) utilises microsphere technology, and semaglutide (once weekly) incorporates fatty acid modifications. Other agents in this class include lixisenatide (once daily).
More recently, oral formulations of GLP-1 receptor agonists have been developed, with oral semaglutide (Rybelsus) becoming the first in this class to receive regulatory approval. This represents a significant advancement, as it provides an oral option for some patients, potentially improving treatment acceptance. Oral semaglutide uses a novel absorption enhancer (SNAC) to facilitate gastrointestinal absorption. The evolution from Gila monster venom to these diverse medication options demonstrates the remarkable journey of pharmaceutical innovation, transforming a natural toxin into a cornerstone of modern diabetes therapy.
Clinical Benefits and Uses of GLP-1 Medications in the UK
GLP-1 receptor agonists have become an integral component of type 2 diabetes management in the UK, with prescribing guided by NICE (National Institute for Health and Care Excellence) recommendations. These medications work through multiple complementary mechanisms: they enhance glucose-dependent insulin secretion, suppress inappropriate glucagon release, slow gastric emptying, and reduce appetite—collectively improving glycaemic control whilst minimising the risk of hypoglycaemia.
NICE guidance (NG28) recommends GLP-1 receptor agonists as a treatment option for adults with type 2 diabetes when:
-
Triple therapy with metformin and two other oral drugs is not effective, not tolerated or contraindicated
-
The person has a BMI of 35 kg/m² or higher (adjust accordingly for people from particular ethnic groups) and specific psychological or other medical problems associated with obesity
-
The person has a BMI lower than 35 kg/m² and insulin would have significant occupational implications, or weight loss would benefit other significant obesity-related comorbidities
-
GLP-1 receptor agonists may also be considered in combination with insulin therapy in specialist care settings
Beyond glycaemic control, specific GLP-1 receptor agonists offer significant cardiovascular benefits. Large-scale cardiovascular outcome trials have demonstrated that certain agents in this class—particularly liraglutide (LEADER trial), semaglutide (SUSTAIN-6 trial), and dulaglutide (REWIND trial)—reduce the risk of major adverse cardiovascular events, including myocardial infarction, stroke, and cardiovascular death. This makes these specific agents particularly valuable for patients with established cardiovascular disease or multiple risk factors.
Weight reduction is another clinically important benefit, with patients typically losing 3–8% of their body weight, depending on the specific agent and dose. Higher doses of semaglutide (2.4 mg weekly, Wegovy) have been specifically licensed for weight management in individuals with obesity, reflecting the medication's potent effects on appetite regulation. The NHS has begun implementing NICE guidance (TA875) for these medications for weight management in specialist services, though availability remains limited and subject to strict eligibility criteria. Treatment targets and drug choices should be individualised according to patient needs, aligned with NICE guidance and local formularies.
Safety Profile and Side Effects of GLP-1 Drugs
Whilst GLP-1 receptor agonists are generally well-tolerated, healthcare professionals and patients must be aware of their safety profile to ensure appropriate use and monitoring. The most common adverse effects are gastrointestinal in nature, affecting up to 40–50% of patients, particularly during treatment initiation or dose escalation. These include:
-
Nausea (most frequent, often transient)
-
Vomiting and diarrhoea
-
Constipation
-
Abdominal discomfort or bloating
These symptoms typically diminish over 4–8 weeks as tolerance develops. Gradual dose titration, as recommended in the Summary of Product Characteristics (SmPC), significantly reduces the severity of gastrointestinal side effects. Patients should be advised to eat smaller, more frequent meals and avoid high-fat foods during the initial treatment period.
Serious but rare adverse effects require clinical vigilance. Acute pancreatitis has been reported with GLP-1 receptor agonists, though a definitive causal relationship remains debated in the literature. Patients should be counselled to seek immediate medical attention if they experience severe, persistent abdominal pain radiating to the back. Treatment should be discontinued if pancreatitis is suspected, and alternative diabetes therapies should be considered.
Gallbladder disease (including cholelithiasis and cholecystitis) has been reported, particularly with substantial weight loss. Dehydration leading to acute kidney injury can occur with severe gastrointestinal side effects. Semaglutide carries a specific warning about potential worsening of diabetic retinopathy in patients with pre-existing retinopathy, particularly with rapid improvement in glucose control.
Animal studies have shown thyroid C-cell tumours with GLP-1 receptor agonists. While no conclusive human risk has been established, UK and EU SmPCs include this as a precaution rather than a contraindication. Patients with personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2 (MEN 2) should discuss this risk with their healthcare provider.
Hypoglycaemia risk is low when GLP-1 receptor agonists are used as monotherapy or with metformin, as their glucose-lowering effect is glucose-dependent. However, when combined with sulfonylureas or insulin, dose adjustments of these concomitant medications may be necessary to prevent hypoglycaemic episodes.
GLP-1 receptor agonists are not recommended during pregnancy or breastfeeding and are not indicated for type 1 diabetes. Some agents have specific renal impairment restrictions (e.g., exenatide is not recommended in severe renal impairment). Patients should report suspected side effects to their healthcare professional or via the MHRA Yellow Card scheme.
Accessing GLP-1 Treatments Through the NHS
Access to GLP-1 receptor agonists through the NHS follows a structured pathway, with prescribing typically initiated by specialist diabetes services or, in some areas, by GPs with appropriate expertise and support. Patients cannot simply request these medications; they must meet specific clinical eligibility criteria as outlined in NICE guidance and local formularies.
The typical pathway begins with a comprehensive diabetes review by your GP or practice nurse. If your current treatment regimen is not achieving target HbA1c levels (usually <58 mmol/mol, though individualised targets apply), and you meet the criteria outlined in NICE guidance, your GP may refer you to a specialist diabetes service. In some integrated care systems, GPs with enhanced diabetes training may initiate GLP-1 therapy directly, supported by local prescribing protocols.
Specialist diabetes services will conduct a thorough assessment, including:
-
Review of your diabetes history and current medications
-
Assessment of cardiovascular risk factors
-
Evaluation of potential contraindications and precautions
-
Discussion of treatment goals, including weight management
-
Education on injection technique (for injectable formulations)
-
Monitoring plan for efficacy and tolerability
NICE recommends that GLP-1 therapy should be reviewed at six months. Treatment should only be continued if there has been a beneficial metabolic response, defined as a reduction in HbA1c of at least 11 mmol/mol (1.0%) and weight loss of at least 3% of initial body weight. This "trial and review" approach ensures that NHS resources are directed towards patients who derive meaningful clinical benefit.
For weight management indications, access follows NICE guidance (TA875). Specialist weight management services may prescribe higher-dose semaglutide (Wegovy) for adults with a BMI ≥35 kg/m² (or ≥30 kg/m² in exceptional cases) and at least one weight-related comorbidity. For people of South Asian, Chinese, other Asian, Middle Eastern, Black African, or African-Caribbean family background, the BMI thresholds are reduced by 2.5 kg/m². However, availability varies significantly across the UK, with many areas maintaining waiting lists due to supply constraints and funding limitations. Patients should discuss their eligibility and local access arrangements with their GP, who can provide information about referral pathways and expected waiting times for specialist assessment.
Frequently Asked Questions
How did Gila monster venom lead to diabetes medication?
Researchers discovered exendin-4 in Gila monster venom, a peptide similar to human GLP-1 but resistant to rapid breakdown. This led to the development of exenatide and subsequent GLP-1 receptor agonists, which are now widely used to treat type 2 diabetes by enhancing insulin secretion, slowing gastric emptying, and reducing appetite.
What are the main side effects of GLP-1 medications?
The most common side effects are gastrointestinal, including nausea, vomiting, diarrhoea, and constipation, affecting up to 40–50% of patients initially. Rare but serious risks include acute pancreatitis, gallbladder disease, and dehydration leading to acute kidney injury, requiring clinical monitoring and patient education.
Can I get GLP-1 medications on the NHS?
Yes, if you meet NICE eligibility criteria, typically when triple oral therapy for type 2 diabetes is inadequate and specific BMI or comorbidity thresholds apply. Access requires GP referral to specialist diabetes services or assessment by GPs with enhanced training, with treatment reviewed at six months to confirm metabolic benefit.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript