Many people starting GLP-1 medications for type 2 diabetes or weight management wonder why they aren't seeing the expected results. GLP-1 receptor agonists like semaglutide, liraglutide, and dulaglutide work by mimicking natural hormones that regulate blood glucose and appetite, but individual responses vary considerably. Several factors—from dosing schedules and biological differences to lifestyle habits and concurrent medications—can influence how well these treatments work. Understanding why GLP-1 therapy may not be effective for you is the first step towards finding the right solution, whether that involves optimising your current treatment, switching medications, or exploring alternative approaches tailored to your individual circumstances.
Summary: GLP-1 medications may not work due to insufficient dosing, individual biological variation in receptor function, advanced beta cell dysfunction, lifestyle factors, or unrealistic expectations about treatment timelines and outcomes.
- GLP-1 receptor agonists stimulate insulin secretion, suppress glucagon, slow gastric emptying, and reduce appetite through action on pancreatic cells and brain centres.
- Gradual dose escalation over weeks to months is essential; premature discontinuation or suboptimal dosing prevents full therapeutic benefit.
- Genetic differences in GLP-1 receptor sensitivity and remaining beta cell function significantly affect individual treatment response.
- Dietary habits, physical activity levels, concurrent medications, and undiagnosed conditions like hypothyroidism can impair GLP-1 effectiveness.
- If treatment fails after optimisation, alternatives include SGLT2 inhibitors, insulin therapy, other weight management medications, or bariatric surgery referral.
- Severe abdominal pain whilst taking GLP-1 medications requires urgent medical attention due to potential pancreatitis or gallbladder complications.
Table of Contents
How GLP-1 Medications Work in the Body
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications primarily used to manage type 2 diabetes and, more recently, obesity. These drugs mimic the action of naturally occurring GLP-1, a hormone produced in the intestines in response to food intake. Understanding their mechanism of action helps explain why they may not work uniformly for everyone.
GLP-1 medications work through several complementary pathways. They stimulate insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning insulin is only released when blood glucose levels are elevated. This reduces the risk of hypoglycaemia when used alone, though this risk increases significantly when combined with insulin or sulfonylureas. Simultaneously, they suppress glucagon release from pancreatic alpha cells, which normally raises blood glucose by promoting hepatic glucose production. This dual action helps maintain more stable blood glucose levels throughout the day.
Beyond glycaemic control, GLP-1 receptor agonists slow gastric emptying, which prolongs the feeling of fullness after meals and reduces appetite. This effect may diminish over time with continued use. They also act on appetite centres in the brain, particularly the hypothalamus, to reduce hunger signals and food cravings. This combination of effects explains why these medications are effective for weight management as well as diabetes control.
Commonly prescribed GLP-1 medications in the UK include semaglutide (Ozempic, Wegovy, Rybelsus), dulaglutide (Trulicity), liraglutide (Victoza, Saxenda), and exenatide products. These vary in dosing frequency—from daily to once weekly—and in their specific receptor binding profiles, which may influence individual response rates and tolerability. Some agents, like semaglutide and dulaglutide, have also demonstrated cardiovascular and renal benefits in clinical trials.
Importantly, GLP-1 receptor agonists are not indicated for type 1 diabetes or diabetic ketoacidosis.
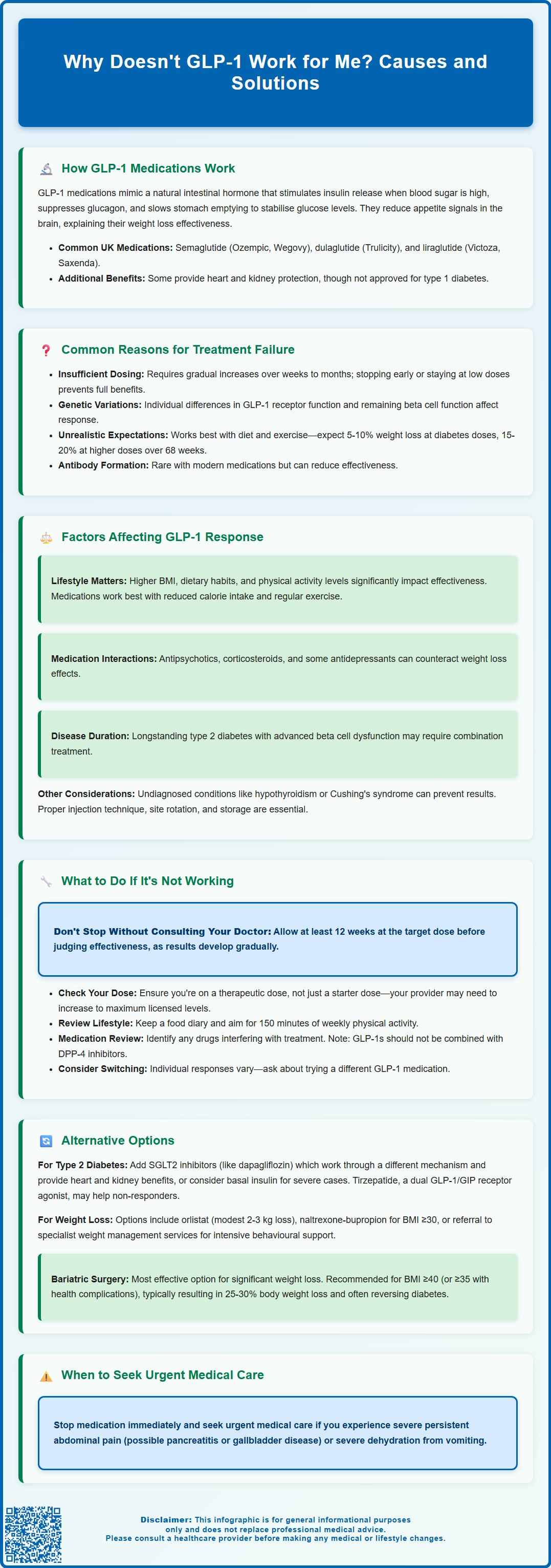
Common Reasons Why GLP-1 Treatment May Not Work
Several factors can explain why GLP-1 medications may not produce the expected results for some individuals. Insufficient dosing is perhaps the most common issue. GLP-1 medications typically require gradual dose escalation over several weeks to months to reach therapeutic levels whilst minimising gastrointestinal side effects. If treatment is discontinued prematurely due to side effects, or if the dose remains suboptimal, the full therapeutic benefit may never be achieved.
Individual biological variation plays a significant role in treatment response. Genetic differences in GLP-1 receptor expression and function can affect how well these medications work. Some people naturally have variations in receptor sensitivity or downstream signalling pathways that reduce drug effectiveness. Additionally, the degree of beta cell function remaining in people with type 2 diabetes varies considerably; those with more advanced beta cell dysfunction may experience less benefit from GLP-1 therapy, as the medication relies on functional beta cells to stimulate insulin secretion.
Poor response to GLP-1 therapy with continued weight loss and hyperglycaemia may occasionally indicate misdiagnosed diabetes type. Some patients may have latent autoimmune diabetes in adults (LADA) or other forms of diabetes requiring insulin therapy.
Antibody formation against GLP-1 medications can occasionally occur, though this is more common with exenatide than with human GLP-1 analogues like liraglutide or semaglutide. Modern GLP-1 analogues are designed to minimise immunogenicity, and neutralising antibodies rarely drive complete non-response.
It's also important to recognise that unrealistic expectations can lead to perceived treatment failure. GLP-1 medications are not miracle cures; they work best as part of a comprehensive approach including dietary modification and physical activity. Weight loss varies by drug and dose—typically 5-10% with diabetes doses and potentially 15-20% with higher weight management doses over 68 weeks. Glycaemic improvements may take weeks to become apparent.
If you experience severe, persistent abdominal pain while taking GLP-1 medications, stop taking the medication and seek urgent medical attention, as this could indicate pancreatitis or gallbladder disease. Similarly, seek medical help if you become dehydrated from vomiting. Report any suspected side effects via the MHRA Yellow Card scheme.
Factors That Affect GLP-1 Response and Effectiveness
Multiple patient-specific and lifestyle factors can significantly influence how well GLP-1 medications work. Body mass index (BMI) and baseline weight appear to correlate with response patterns; individuals with higher BMI may experience different response patterns compared to those with lower BMI values, though all patients follow the same fixed dose titration schedules as outlined in the medication's prescribing information.
Dietary habits profoundly impact GLP-1 effectiveness. These medications work synergistically with reduced calorie intake; if dietary patterns remain unchanged, weight loss and glycaemic benefits will be limited. High-fat, high-calorie diets can overwhelm the appetite-suppressing effects of GLP-1 therapy. Similarly, physical activity levels influence outcomes—sedentary individuals typically experience less benefit than those who incorporate regular exercise into their routine.
Concurrent medications may interfere with GLP-1 action or counteract their effects. Medications that promote weight gain, such as certain antipsychotics, corticosteroids, or some antidepressants, can blunt weight loss effects. Additionally, GLP-1 medications can affect the absorption of some oral medicines by slowing gastric emptying. This requires particular attention with narrow therapeutic index drugs, where your doctor may need to adjust timing or dosing.
Duration of diabetes and underlying pathophysiology matter considerably. People with longstanding type 2 diabetes often have more advanced beta cell dysfunction and may respond less robustly to GLP-1 therapy. Those with significant insulin resistance may require combination therapy rather than GLP-1 monotherapy. Furthermore, undiagnosed conditions such as hypothyroidism or Cushing's syndrome can impair weight loss and glycaemic control regardless of GLP-1 treatment. Your doctor may consider testing for these conditions based on clinical features rather than as routine screening.
Adherence and injection technique also affect outcomes. Missing doses, incorrect injection sites, or improper storage of medication can all reduce effectiveness. Rotate injection sites to avoid injection-site reactions or nodules, which can occur particularly with some formulations. GLP-1 medications are generally not recommended for people with severe gastrointestinal disease, such as severe gastroparesis.
What to Do If Your GLP-1 Medication Isn't Working
If you feel your GLP-1 medication isn't working as expected, do not stop treatment abruptly without consulting your healthcare provider. There are several systematic steps to take before concluding that the medication has failed.
First, assess your expectations and timeline. Discuss with your GP or diabetes specialist what constitutes realistic treatment goals. For diabetes management, HbA1c reductions typically range from 5-15 mmol/mol (0.5-1.5%) depending on the specific medication and dose, though targets should be individualised based on your circumstances as per NICE guidance. Weight loss usually occurs gradually over 3-6 months. If you've been on treatment for less than 12 weeks at the target dose, it may simply be too early to judge effectiveness.
Review your current dose with your healthcare provider. Many people remain on starter doses that are intended only for tolerability, not therapeutic effect. Your clinician may recommend increasing to the maximum licensed dose if you're tolerating the current dose well. For example, semaglutide can be increased up to 2 mg weekly for diabetes (Ozempic), or up to 2.4 mg weekly for weight management (Wegovy). Note that specific stopping rules apply to some medications—for example, Saxenda (liraglutide 3 mg) should be discontinued if a 5% weight reduction is not achieved after 12 weeks at the full dose.
Evaluate lifestyle factors honestly. Keep a food diary for a week to identify areas where dietary improvements could be made. Consider whether you're meeting physical activity recommendations (at least 150 minutes of moderate-intensity activity weekly). Your GP may refer you to a dietitian or weight management service for additional support.
Request a medication review to identify any drugs that might be interfering with GLP-1 effectiveness. Your healthcare provider can assess whether alternative medications might be more suitable for concurrent conditions. Remember that GLP-1 receptor agonists should not be combined with DPP-4 inhibitors, as both work on the incretin system.
Consider switching GLP-1 medications. Individual responses can vary between different GLP-1 receptor agonists. Some people respond better to semaglutide than liraglutide, or vice versa. Your specialist may suggest trying an alternative agent before abandoning the class entirely.
If you're planning pregnancy, discuss this with your doctor. GLP-1 medications are not recommended during pregnancy or breastfeeding, and some (like semaglutide) should be discontinued at least 2 months before a planned pregnancy.
Alternative Options When GLP-1 Treatment Fails
When GLP-1 medications prove ineffective despite optimisation, several alternative therapeutic strategies exist, depending on whether the primary goal is diabetes management or weight loss.
For type 2 diabetes management, NICE guidelines (NG28) recommend a stepwise approach. If GLP-1 therapy fails to achieve individualised HbA1c targets, combination therapy is often the next step. This might include:
-
Adding SGLT2 inhibitors (such as dapagliflozin or empagliflozin), which work through a different mechanism by increasing urinary glucose excretion and offer cardiovascular and renal benefits. Eligibility depends on eGFR and cardiovascular risk status.
-
Combining with DPP-4 inhibitors is generally not recommended, as both drug classes work on the incretin system
-
Adding basal insulin for those with more significant hyperglycaemia, which can be used alongside GLP-1 medications (with careful monitoring for hypoglycaemia)
-
Switching to insulin therapy entirely may be necessary for those with advanced beta cell failure
For weight management, when GLP-1 medications don't produce adequate weight loss, alternatives include:
-
Orlistat, a lipase inhibitor that reduces fat absorption, though weight loss is typically modest (2-3 kg on average)
-
Naltrexone-bupropion (Mysimba), which works on appetite centres through different pathways. NICE (TA733) recommends this for adults with a BMI of at least 30 kg/m² (or 27 kg/m² with weight-related comorbidities) in specific circumstances, though local availability may vary.
-
Referral to specialist weight management services for intensive behavioural interventions, very-low-calorie diets, or consideration for bariatric surgery
Bariatric surgery remains the most effective intervention for significant, sustained weight loss. NICE recommends considering surgical options for people with BMI ≥40 kg/m² (or ≥35 kg/m² with comorbidities). Lower thresholds apply for people with recent-onset type 2 diabetes (BMI ≥30 kg/m²) and for people of Asian family origin (typically 2.5 kg/m² lower). Procedures such as gastric bypass or sleeve gastrectomy typically result in 25-30% total body weight loss and often lead to diabetes remission.
Emerging therapies show promise for those who don't respond to current GLP-1 medications. Tirzepatide, a dual GLP-1/GIP receptor agonist, has been approved by NICE for type 2 diabetes management. Its status for weight management depends on licensing and NHS commissioning decisions. Your specialist can discuss whether newer medications might be appropriate for your situation.
Ultimately, personalised medicine approaches recognise that no single treatment works for everyone. Working closely with your diabetes team or weight management specialist to find the right combination of medications, lifestyle interventions, and support services offers the best chance of achieving your health goals.
Scientific References
- Ozempic 0.5 mg solution for injection in pre-filled pen - Summary of Product Characteristics.
- GLP-1 medicines for weight loss and diabetes: what you need to know.
- Guidance for Prescribing Glucagon-like peptide 1 (GLP 1) agonists.
- Mounjaro (tirzepatide) EPAR.
- Bone Health After Exercise Alone, GLP-1 Receptor Agonist.
Frequently Asked Questions
How long does it take for GLP-1 medications to work?
GLP-1 medications typically require 12 weeks at the target therapeutic dose to assess effectiveness. Weight loss occurs gradually over 3-6 months, whilst glycaemic improvements may become apparent within weeks of reaching optimal dosing.
Can I switch to a different GLP-1 medication if one doesn't work?
Yes, individual responses vary between different GLP-1 receptor agonists. Your healthcare provider may suggest switching from one agent (such as liraglutide) to another (such as semaglutide) before concluding that the entire medication class is ineffective for you.
What should I do if my GLP-1 medication stops working over time?
Consult your healthcare provider to review your current dose, assess lifestyle factors, and consider combination therapy with other diabetes or weight management medications. Do not stop treatment abruptly without medical guidance, as alternative strategies or dose adjustments may restore effectiveness.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript