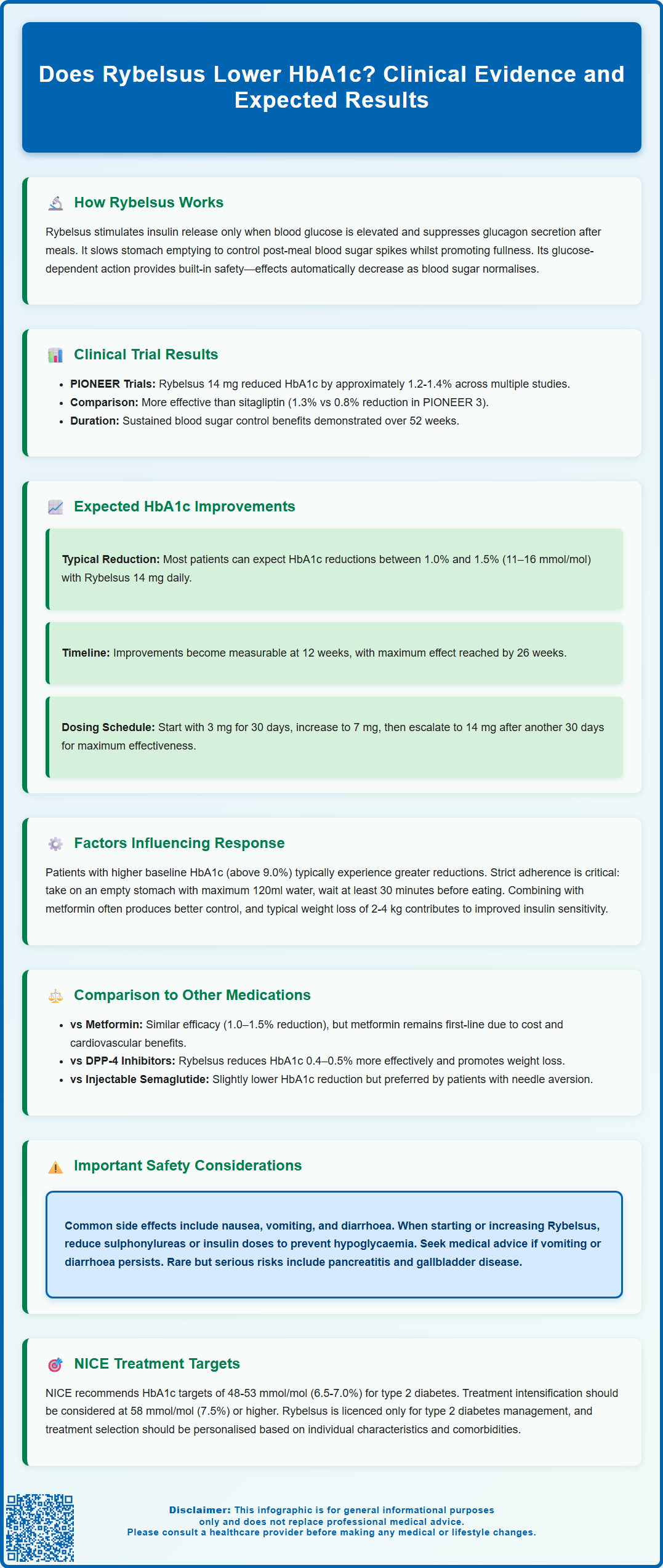
Rybelsus (semaglutide) is an oral glucagon-like peptide-1 receptor agonist (GLP-1 RA) licensed in the UK for treating type 2 diabetes mellitus. Clinical evidence demonstrates that Rybelsus effectively lowers HbA1c levels through multiple mechanisms, including glucose-dependent insulin secretion, glucagon suppression, and delayed gastric emptying. The PIONEER clinical trial programme has established robust efficacy data, with the 14 mg maintenance dose typically reducing HbA1c by 1.0–1.5% (11–16 mmol/mol). Understanding how Rybelsus influences glycaemic control helps clinicians and patients make informed treatment decisions aligned with NICE guidance for individualised diabetes management.
Summary: Rybelsus (oral semaglutide) lowers HbA1c by approximately 1.0–1.5% (11–16 mmol/mol) at the 14 mg maintenance dose in adults with type 2 diabetes.
- Rybelsus is an oral GLP-1 receptor agonist that stimulates insulin secretion and suppresses glucagon in a glucose-dependent manner, reducing hypoglycaemia risk.
- The PIONEER clinical trial programme demonstrated HbA1c reductions of 1.2–1.4% with the 14 mg dose across diverse patient populations.
- Treatment begins at 3 mg daily for tolerability, escalates to 7 mg after 30 days, then to 14 mg for maximal glycaemic effect.
- Maximal HbA1c reduction typically occurs by 26 weeks, with NICE recommending HbA1c monitoring every 3–6 months until stable.
- Common side effects include gastrointestinal symptoms; caution is needed when combining with sulphonylureas or insulin due to increased hypoglycaemia risk.
- Rybelsus is licensed for type 2 diabetes management only and requires specific dosing on an empty stomach with restricted food and fluid intake for 30 minutes.
Table of Contents
How Rybelsus Works to Lower HbA1c Levels
Rybelsus (semaglutide) is an oral glucagon-like peptide-1 receptor agonist (GLP-1 RA) licensed in the UK for the treatment of type 2 diabetes mellitus only. It works through multiple complementary mechanisms to improve glycaemic control and reduce HbA1c levels.
The primary mechanism involves stimulating insulin secretion from pancreatic beta cells in a glucose-dependent manner. This means Rybelsus enhances insulin release only when blood glucose levels are elevated, which significantly reduces the risk of hypoglycaemia compared to some other glucose-lowering agents. However, this risk increases when Rybelsus is combined with sulphonylureas or insulin, and dose adjustments of these medications may be needed. Simultaneously, semaglutide suppresses glucagon secretion from pancreatic alpha cells, particularly after meals when glucagon levels would otherwise inappropriately rise and stimulate hepatic glucose production.
Beyond its direct pancreatic effects, Rybelsus slows gastric emptying, which moderates the rate at which glucose enters the bloodstream following food intake. This contributes to reduced postprandial glucose excursions—a key component of overall glycaemic control. Additionally, GLP-1 receptor agonists act on appetite centres in the hypothalamus, promoting satiety and often leading to modest weight reduction, which itself improves insulin sensitivity.
The glucose-dependent nature of Rybelsus is particularly important from a safety perspective. Unlike sulphonylureas or exogenous insulin, the medication's effect diminishes as blood glucose normalises, providing a built-in safety mechanism. Common side effects include gastrointestinal symptoms (nausea, vomiting, diarrhoea), and there are rare but serious risks including pancreatitis and gallbladder disease. Caution is needed in patients with diabetic retinopathy, particularly when achieving rapid improvements in glycaemic control.
Clinical Evidence: Rybelsus HbA1c Reduction Results
The efficacy of Rybelsus in reducing HbA1c has been extensively evaluated through the PIONEER clinical trial programme, a series of phase 3 studies that formed the basis for regulatory approval by the MHRA and EMA. These trials enrolled diverse populations with type 2 diabetes across different treatment backgrounds and disease durations.
In the PIONEER 1 trial, which assessed Rybelsus as monotherapy in treatment-naïve patients, both the 7 mg and 14 mg doses demonstrated statistically significant HbA1c reductions compared to placebo. The 14 mg dose achieved mean HbA1c reductions of approximately 1.4% from baseline at 26 weeks. PIONEER 3, which compared Rybelsus directly against sitagliptin (a DPP-4 inhibitor), showed superior glycaemic control with Rybelsus 14 mg, achieving HbA1c reductions of around 1.3% versus 0.8% with sitagliptin.
Perhaps most notably, PIONEER 4 evaluated Rybelsus as add-on therapy to metformin with or without an SGLT2 inhibitor. Results demonstrated HbA1c reductions of approximately 1.2% with the 14 mg dose. The PIONEER 7 trial provided a flexible dose-adjustment design more reflective of real-world practice, confirming sustained glycaemic benefits over 52 weeks.
Across the PIONEER programme, a substantial proportion of participants achieved therapeutic HbA1c targets. NICE recommends individualised HbA1c targets for people with type 2 diabetes, typically between 48-53 mmol/mol (6.5-7.0%) depending on the person's circumstances and treatments used. Treatment intensification is generally considered when HbA1c rises to 58 mmol/mol (7.5%) or higher. These robust clinical data support Rybelsus as an evidence-based option for meaningful HbA1c reduction in accordance with contemporary diabetes management guidelines.
Expected HbA1c Improvements with Rybelsus Treatment
When initiating Rybelsus therapy, patients and healthcare professionals should have realistic expectations regarding the magnitude and timeline of HbA1c improvements. Based on clinical trial data and real-world evidence, most patients can expect HbA1c reductions between 1.0% and 1.5% (11–16 mmol/mol) when taking the maintenance dose of 14 mg daily.
The dose-escalation schedule is important for both tolerability and efficacy. Treatment typically begins with 3 mg once daily for 30 days, which is an initiation dose primarily to improve gastrointestinal tolerability rather than for glycaemic effect. After this initial period, the dose increases to 7 mg daily, where modest HbA1c reductions begin to emerge. For patients requiring further glycaemic improvement, escalation to the 14 mg maintenance dose after an additional 30 days provides maximal HbA1c-lowering efficacy.
The time course of HbA1c reduction reflects both the pharmacological action of semaglutide and the biological nature of HbA1c measurement. Whilst improvements in fasting and postprandial glucose occur within days to weeks, HbA1c—representing average glycaemia over approximately three months—typically shows measurable reduction at 12 weeks, with maximal effect evident by 26 weeks of treatment.
Individual response varies considerably based on baseline HbA1c, diabetes duration, beta-cell function, and adherence to therapy. Patients with higher baseline HbA1c levels often experience greater absolute reductions, though percentage reductions remain relatively consistent. It is important to note that whilst clinical trials demonstrate average responses, individual patients may experience greater or lesser benefit. NICE recommends measuring HbA1c every 3-6 months until stable, then every 6 months to assess treatment response and guide ongoing management decisions, including potential dose adjustment or addition of complementary therapies.
When adding or up-titrating Rybelsus, consider reviewing and potentially reducing doses of sulphonylureas or insulin to minimise hypoglycaemia risk.
Factors That Influence HbA1c Response to Rybelsus
Multiple patient-specific and treatment-related factors influence the magnitude of HbA1c reduction achieved with Rybelsus therapy. Understanding these variables helps clinicians set appropriate expectations and optimise treatment outcomes.
Baseline HbA1c is among the most significant predictors of absolute reduction. Patients starting treatment with higher HbA1c levels (e.g., >9.0% or 75 mmol/mol) typically experience greater absolute reductions than those with near-target baseline values, though the latter may still achieve important clinical benefits. Duration of diabetes also matters—individuals with shorter disease duration and preserved beta-cell function generally respond more robustly to GLP-1 receptor agonists than those with longstanding diabetes and significant beta-cell exhaustion.
Adherence to the dosing regimen critically affects outcomes. Rybelsus must be taken on an empty stomach with no more than 120 ml of water, and patients must wait at least 30 minutes before eating, drinking, or taking other medications. The tablet must be swallowed whole and not split, crushed or chewed. Suboptimal adherence to these specific instructions can significantly impair absorption and reduce efficacy.
Concomitant medications and lifestyle factors further modulate response. Patients taking metformin alongside Rybelsus often achieve better glycaemic control than with either agent alone, reflecting complementary mechanisms of action. Some medications may affect Rybelsus absorption or response; for example, levothyroxine exposure may increase, requiring thyroid function monitoring. Body weight changes associated with Rybelsus treatment—typically 2–4 kg reduction—contribute to improved insulin sensitivity and HbA1c lowering. Finally, gastrointestinal tolerability influences persistence; nausea and other GI adverse effects, whilst usually transient, may lead to treatment discontinuation in some patients, thereby limiting long-term glycaemic benefits. It's important to maintain adequate hydration during episodes of gastrointestinal side effects and seek medical advice if experiencing persistent vomiting or diarrhoea.
Comparing Rybelsus HbA1c Reduction to Other Diabetes Medications
When selecting glucose-lowering therapy, clinicians must consider comparative efficacy alongside safety, tolerability, and patient preferences. Rybelsus occupies a distinctive position within the type 2 diabetes treatment landscape as the first oral GLP-1 receptor agonist, combining the efficacy of this drug class with oral administration.
Compared to metformin—the recommended first-line agent per NICE guidance—Rybelsus demonstrates similar or slightly superior HbA1c-lowering efficacy (1.0–1.5% versus 1.0–1.5%), though metformin remains preferred initially due to extensive safety data, low cost, and cardiovascular benefits. When metformin alone provides insufficient control, NICE NG28 recommends considering additional agents based on individual patient factors including cardiovascular disease, heart failure, and chronic kidney disease.
Against DPP-4 inhibitors (sitagliptin, linagliptin), Rybelsus shows superior HbA1c reduction—approximately 0.4–0.5% greater lowering in head-to-head trials. Both drug classes have low hypoglycaemia risk, but Rybelsus additionally promotes weight loss whilst DPP-4 inhibitors are weight-neutral. SGLT2 inhibitors (dapagliflozin, empagliflozin) typically provide HbA1c reductions of approximately 0.5–1.0% and offer proven cardiovascular and renal benefits, making them preferred add-on therapy for patients with established cardiovascular disease, heart failure or CKD per current NICE guidance.
Compared to injectable GLP-1 receptor agonists, Rybelsus (oral semaglutide 14 mg) demonstrates slightly lower HbA1c reduction than once-weekly subcutaneous semaglutide but similar efficacy to other injectable GLP-1 RAs such as dulaglutide or liraglutide. The oral formulation may be preferred by patients with needle aversion, though the specific dosing requirements may affect adherence. Sulphonylureas achieve similar HbA1c reductions but carry significant hypoglycaemia risk and promote weight gain, making them less favourable options in contemporary practice.
It is important to note that Rybelsus is licensed for type 2 diabetes management, not for weight loss. Ultimately, treatment selection should follow a personalised approach, considering individual patient characteristics, comorbidities, and preferences alongside glycaemic efficacy.
Frequently Asked Questions
How much does Rybelsus lower HbA1c levels?
Clinical trials show that Rybelsus 14 mg typically reduces HbA1c by 1.0–1.5% (11–16 mmol/mol) from baseline. Individual response varies based on baseline HbA1c, diabetes duration, and adherence to the specific dosing requirements.
How long does it take for Rybelsus to lower HbA1c?
Measurable HbA1c reduction typically occurs at 12 weeks of treatment, with maximal effect evident by 26 weeks. NICE recommends monitoring HbA1c every 3–6 months to assess treatment response.
Is Rybelsus more effective than other diabetes medications for lowering HbA1c?
Rybelsus demonstrates superior HbA1c reduction compared to DPP-4 inhibitors (approximately 0.4–0.5% greater lowering) and similar efficacy to metformin. It shows slightly lower HbA1c reduction than injectable semaglutide but offers the convenience of oral administration for patients with needle aversion.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript