Ozempic (semaglutide) is a widely prescribed GLP-1 receptor agonist for type 2 diabetes management in the UK. Whilst gastrointestinal side effects such as nausea and diarrhoea are well documented, some patients report experiencing hot flushes during treatment. Hot flushes are not officially listed as a recognised adverse effect in the Summary of Product Characteristics or MHRA-approved patient information. This article examines whether Ozempic causes hot flushes, explores potential indirect mechanisms including weight loss and hormonal changes, and provides guidance on managing vasomotor symptoms whilst continuing diabetes therapy.
Summary: Hot flushes are not officially recognised as a direct side effect of Ozempic in UK regulatory documentation, though some patients report experiencing them during treatment.
- Ozempic (semaglutide) is a GLP-1 receptor agonist licensed for type 2 diabetes, administered as a once-weekly subcutaneous injection.
- The most common side effects are gastrointestinal, including nausea, vomiting, diarrhoea, and decreased appetite.
- Hot flushes may occur indirectly through weight loss-related hormonal changes, metabolic shifts, or glycaemic fluctuations rather than direct pharmacological action.
- Patients experiencing troublesome hot flushes should seek medical review to exclude alternative causes such as thyroid dysfunction or menopausal status.
- Management includes lifestyle modifications, trigger avoidance, and medical assessment; do not discontinue Ozempic without consulting your healthcare provider.
Table of Contents
Understanding Ozempic and Its Common Side Effects
Ozempic (semaglutide) is a glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for the treatment of type 2 diabetes mellitus. Administered as a once-weekly subcutaneous injection, it works by mimicking the action of the naturally occurring hormone GLP-1, which stimulates insulin secretion in response to elevated blood glucose levels, suppresses glucagon release, and slows gastric emptying. These mechanisms collectively improve glycaemic control and often result in weight loss as a secondary benefit.
The most frequently reported adverse effects of Ozempic are gastrointestinal in nature, particularly during dose titration. According to the Summary of Product Characteristics (SmPC), these include:
-
Nausea (very common)
-
Vomiting (common)
-
Diarrhoea (very common)
-
Constipation (common)
-
Abdominal pain or discomfort (common)
-
Decreased appetite (very common)
These symptoms typically diminish over time as the body adjusts to the medication. Other recognised side effects include injection site reactions, fatigue, dizziness, and headache. More serious but less common adverse effects include pancreatitis, gallbladder disease, and potential thyroid C-cell tumours (observed in animal studies, though the clinical relevance in humans remains uncertain).
Patients initiating Ozempic are generally advised to start at a low dose (0.25 mg weekly) with gradual titration every 4 weeks to therapeutic doses (0.5 mg, 1 mg, or 2 mg weekly) to minimise gastrointestinal side effects. There is an increased risk of hypoglycaemia when Ozempic is used in combination with insulin or sulfonylureas, and dose adjustments of these medications may be necessary.
The MHRA and prescribing information provide comprehensive guidance on adverse effect profiles, though hot flushes are not listed among the established side effects in the official product literature. Understanding the documented side effect profile is essential when evaluating any new or unexpected symptoms during treatment. Patients who suspect they are experiencing side effects not listed in the patient information leaflet should report them through the MHRA Yellow Card Scheme.
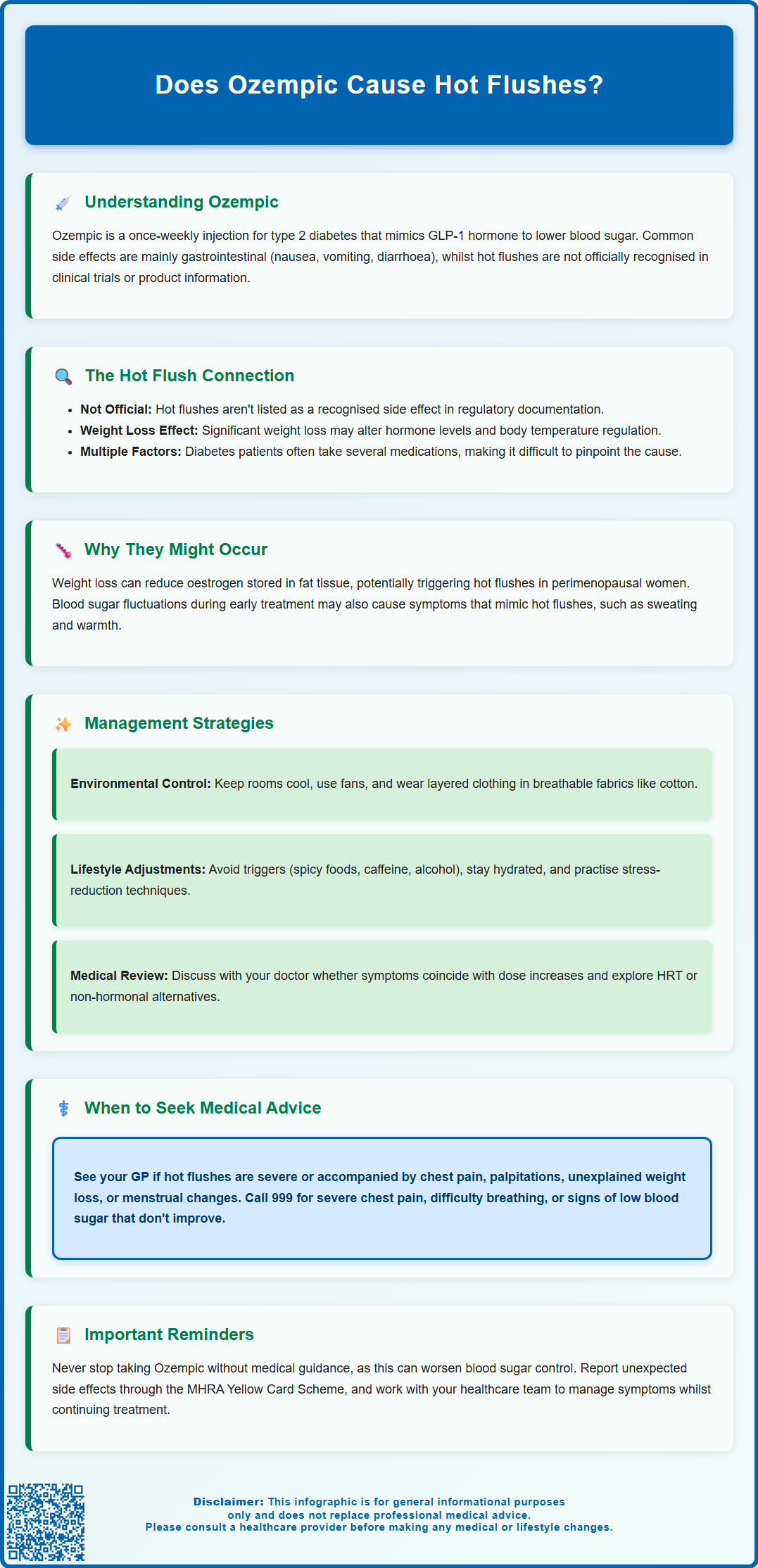
The Connection Between Ozempic and Hot Flushes
Hot flushes (also called hot flashes)—sudden sensations of intense warmth, typically affecting the face, neck, and chest, often accompanied by sweating and flushing—are not officially recognised as a direct side effect of Ozempic in the Summary of Product Characteristics (SmPC) or patient information leaflets approved by the MHRA. However, some patients have anecdotally reported experiencing hot flushes or similar vasomotor symptoms whilst taking semaglutide, prompting questions about a potential connection.
It is important to distinguish between established causation and anecdotal association. The absence of hot flushes from official adverse effect listings suggests that clinical trials did not identify a statistically significant link between Ozempic and this symptom. Nevertheless, patient reports indicate that some individuals do experience these sensations during treatment, warranting careful consideration of possible mechanisms.
Several factors may explain why patients report hot flushes whilst taking Ozempic:
-
Metabolic changes: Significant weight loss and alterations in body composition can affect thermoregulation
-
Hormonal fluctuations: Weight loss may influence sex hormone levels, particularly oestrogen
-
Blood glucose variations: Rapid changes in glycaemic control may trigger autonomic responses
-
Concurrent medications or conditions: Many patients with type 2 diabetes take multiple medications that could contribute to vasomotor symptoms
There is no official link established between Ozempic and hot flushes based on current evidence from randomised controlled trials. However, the complexity of metabolic and hormonal regulation means that indirect effects cannot be entirely excluded. Patients experiencing hot flushes should not automatically attribute them to Ozempic without considering alternative explanations, including menopausal status, thyroid dysfunction, or other medical conditions.
Why Hot Flushes May Occur During Ozempic Treatment
Whilst hot flushes are not a documented pharmacological effect of semaglutide, several hypothetical indirect mechanisms may explain why some patients experience vasomotor symptoms during Ozempic treatment. Understanding these potential pathways helps clinicians and patients evaluate the symptom in context.
Weight loss and hormonal changes represent the most plausible explanation. Adipose tissue functions as an endocrine organ, producing and storing sex hormones, particularly oestrogen. Significant weight reduction—a common outcome of Ozempic therapy—can alter the balance of circulating hormones. In women approaching or experiencing menopause, this metabolic shift may precipitate or exacerbate hot flushes. Similarly, changes in body composition can affect the conversion of androgens to oestrogens in peripheral tissues, potentially triggering vasomotor instability.
Autonomic nervous system effects may theoretically play a role. GLP-1 receptors are present in various tissues beyond the pancreas, including the central nervous system and cardiovascular system. Whilst semaglutide's primary actions target glucose regulation through enhanced insulin secretion, reduced glucagon, and slowed gastric emptying, changes in autonomic function could theoretically affect thermoregulation and vascular tone, though this remains speculative.
Glycaemic fluctuations during the initial treatment period may trigger symptoms resembling hot flushes. As Ozempic lowers blood glucose levels, some patients experience transient autonomic responses, including sweating, warmth, and palpitations. These symptoms may sometimes represent hypoglycaemia, particularly when Ozempic is combined with insulin or sulfonylureas. This risk should be carefully monitored, and medication doses may need adjustment.
Additionally, concurrent medical conditions must be considered. Patients with type 2 diabetes often have comorbidities such as thyroid disorders, which can cause hot flushes independently. Medications including certain antidepressants, antihypertensives, and other diabetes treatments may also contribute to vasomotor symptoms. A thorough medication review is essential when evaluating new symptoms during Ozempic therapy.
Managing Hot Flushes While Taking Ozempic
For patients experiencing hot flushes during Ozempic treatment, several practical strategies can help manage symptoms whilst continuing therapy. These approaches focus on lifestyle modifications, symptomatic relief, and addressing potential underlying causes.
Lifestyle and environmental adjustments often provide significant relief:
-
Temperature control: Maintain cooler ambient temperatures, use fans, and dress in layers that can be easily removed
-
Breathable fabrics: Choose natural fibres such as cotton and linen that allow better air circulation
-
Trigger avoidance: Identify and minimise exposure to common triggers including spicy foods, caffeine, alcohol, and hot beverages
-
Stress management: Practise relaxation techniques such as deep breathing exercises, meditation, or yoga, as stress can exacerbate vasomotor symptoms
-
Regular exercise: Moderate physical activity may help regulate body temperature and improve overall wellbeing, though intense exercise immediately before bed should be avoided
Dietary considerations may also prove beneficial. Maintaining stable blood glucose levels through regular, balanced meals can reduce autonomic fluctuations. Adequate hydration is essential, as dehydration may worsen hot flushes. Some patients find that reducing intake of known vasodilators (alcohol, spicy foods) decreases symptom frequency.
Medical review is important if hot flushes are troublesome. Your GP or diabetes specialist should:
-
Evaluate whether symptoms coincide with dose escalation (suggesting a possible connection to treatment)
-
Review all concurrent medications for potential contributors
-
Assess for alternative causes, particularly thyroid function and menopausal status in women
-
Consider whether glycaemic control has changed significantly
-
Review insulin or sulfonylurea doses if hypoglycaemia is suspected
For women experiencing menopausal hot flushes, hormone replacement therapy (HRT) is generally considered first-line treatment where appropriate, in line with NICE guidance. Non-hormonal alternatives (such as certain SSRIs/SNRIs, gabapentin, or clonidine) may be suitable where HRT is contraindicated. Any such treatment should be discussed with a healthcare professional who can assess suitability in the context of diabetes management. Continuing Ozempic whilst addressing hot flushes through alternative means is often possible and appropriate.
When to Seek Medical Advice About Hot Flushes
Whilst hot flushes are generally not a serious medical concern, certain circumstances warrant prompt medical evaluation to exclude underlying conditions or complications that require intervention.
Contact your GP or diabetes care team if:
-
Hot flushes are severe, persistent, or significantly impacting quality of life, affecting sleep, work, or daily activities
-
Symptoms are accompanied by chest pain, palpitations, or shortness of breath, which could indicate cardiovascular issues
-
You experience unexplained weight loss beyond what is expected with Ozempic, or other constitutional symptoms such as night sweats
-
Hot flushes occur alongside tremor, anxiety, or heat intolerance, which may suggest thyroid dysfunction (hyperthyroidism)
-
There are changes in menstrual patterns or other hormonal symptoms in premenopausal women
-
You develop new or worsening symptoms after starting Ozempic or increasing the dose
Call 999 or seek urgent medical attention if hot flushes are accompanied by:
-
Severe chest pain, difficulty breathing, or symptoms of anaphylaxis
-
Signs of hypoglycaemia (confusion, excessive sweating, trembling, rapid heartbeat) that do not resolve with glucose intake
-
Symptoms of pancreatitis (severe, persistent abdominal pain radiating to the back, nausea, vomiting)
-
Severe dehydration from concurrent vomiting or diarrhoea
For urgent concerns that are not life-threatening, contact NHS 111 for advice.
Your healthcare provider can conduct appropriate investigations, which may include thyroid function tests, hormone levels, cardiovascular assessment, or review of glycaemic control through HbA1c and glucose monitoring. If you are taking insulin or sulfonylureas alongside Ozempic, your doctor may need to adjust these medications to reduce hypoglycaemia risk.
Do not discontinue Ozempic without medical advice, as abrupt cessation may result in deterioration of glycaemic control. If hot flushes are intolerable, your clinician can discuss alternative diabetes management strategies or symptomatic treatments that allow continuation of effective therapy. Open communication with your healthcare team ensures that both diabetes control and quality of life are optimised during treatment.
If you suspect you are experiencing a side effect from Ozempic that is not listed in the patient information leaflet, report it to the MHRA through the Yellow Card Scheme.
Frequently Asked Questions
Are hot flushes a recognised side effect of Ozempic?
No, hot flushes are not listed as an established side effect in the Summary of Product Characteristics or MHRA-approved patient information for Ozempic. However, some patients report experiencing them during treatment, possibly due to indirect mechanisms such as weight loss and hormonal changes.
Why might I experience hot flushes whilst taking Ozempic?
Hot flushes during Ozempic treatment may result from significant weight loss affecting hormone levels, metabolic changes influencing thermoregulation, or glycaemic fluctuations. Alternative causes such as menopausal status, thyroid dysfunction, or concurrent medications should also be considered.
When should I contact my doctor about hot flushes on Ozempic?
Seek medical advice if hot flushes are severe, persistent, or accompanied by chest pain, palpitations, unexplained weight loss, or symptoms suggesting thyroid dysfunction. Do not discontinue Ozempic without consulting your healthcare provider, as abrupt cessation may worsen glycaemic control.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript










