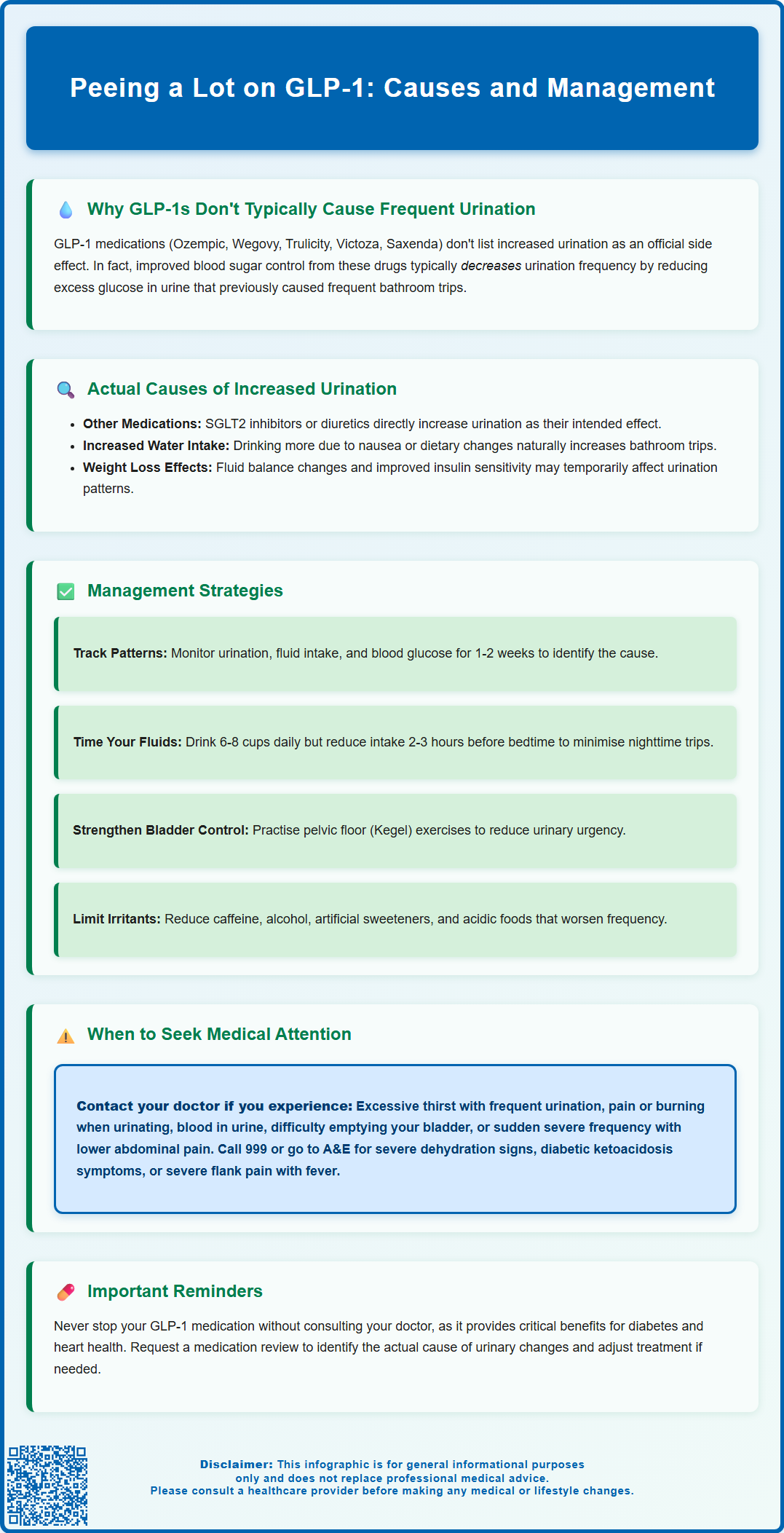
Many patients taking GLP-1 receptor agonists such as semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), or liraglutide (Victoza, Saxenda) report changes in urination patterns. However, peeing a lot on GLP-1 medications is not a recognised side effect in official MHRA guidance. When increased urination occurs, it typically reflects indirect factors such as improved blood glucose control, dietary changes, increased fluid intake, or co-prescribed medications like SGLT2 inhibitors or diuretics. Understanding the mechanisms behind GLP-1 therapy and identifying contributing factors can help you manage symptoms effectively whilst maintaining the important therapeutic benefits these medications provide for type 2 diabetes and weight management.
Summary: Increased urination is not a recognised side effect of GLP-1 medications; when it occurs, it typically results from improved glucose control, increased fluid intake, or co-prescribed medications rather than the GLP-1 drug itself.
- GLP-1 receptor agonists (semaglutide, dulaglutide, liraglutide) work by enhancing insulin secretion, suppressing glucagon, slowing gastric emptying, and reducing appetite.
- Improved blood glucose control from GLP-1 therapy typically reduces urination by eliminating osmotic diuresis caused by excess glucose in urine.
- Co-prescribed SGLT2 inhibitors or diuretics are more likely causes of increased urination than GLP-1 medications themselves.
- Seek medical attention for excessive thirst with frequent urination, pain during urination, blood in urine, or signs of dehydration or infection.
- Do not discontinue GLP-1 medication without medical advice; discuss persistent symptoms with your GP or diabetes specialist for appropriate assessment and management.
Table of Contents
- Why GLP-1 Medications May Cause Increased Urination
- Common Urinary Side Effects of GLP-1 Receptor Agonists
- When Frequent Urination on GLP-1 Treatment Needs Medical Attention
- Managing Increased Urination While Taking GLP-1 Medications
- Other Factors That May Affect Urination During GLP-1 Therapy
- Frequently Asked Questions
Why GLP-1 Medications May Cause Increased Urination
GLP-1 receptor agonists, including semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda), are increasingly prescribed for type 2 diabetes management and weight loss. It's important to note that increased urination is not listed as a recognised side effect in the official MHRA/EMC Summaries of Product Characteristics (SmPCs) for these medications.
If you experience changes in urination patterns while taking GLP-1 medications, this is likely indirect rather than a primary drug action. GLP-1 medications work by mimicking the incretin hormone glucagon-like peptide-1, which enhances insulin secretion in response to food, suppresses glucagon release, slows gastric emptying, and reduces appetite. These effects lead to improved glycaemic control and significant weight loss in many patients.
Paradoxically, improved blood glucose control often reduces urination frequency. In poorly controlled diabetes, excess glucose in the blood is filtered into urine (glycosuria), drawing water with it through osmotic diuresis—a process that causes frequent urination. As GLP-1 therapy improves glucose control, this osmotic effect typically diminishes, potentially normalising previously excessive urination patterns.
Weight loss during GLP-1 therapy may temporarily affect fluid balance in the body, which could influence urination patterns. Additionally, other factors such as increased fluid intake or co-prescribed medications (particularly SGLT2 inhibitors or diuretics) are more likely explanations for increased urination than the GLP-1 medication itself.
Common Urinary Side Effects of GLP-1 Receptor Agonists
According to the MHRA-approved Summaries of Product Characteristics (SmPCs) for GLP-1 receptor agonists, urinary symptoms are not among the recognised adverse effects of these medications. The predominant side effects include:
-
Gastrointestinal symptoms: nausea, vomiting, diarrhoea, constipation, and abdominal pain (affecting 10-50% of patients depending on the specific product and dose, particularly during dose escalation)
-
Injection site reactions: redness, itching, or discomfort at the subcutaneous injection site
-
Hypoglycaemia: particularly when combined with insulin or sulphonylureas
-
Decreased appetite: an intended therapeutic effect that contributes to weight loss
However, some patients do report changes in urinary frequency or patterns. These reports may reflect:
Improved diabetes control: Better glycaemic management reduces osmotic diuresis (excessive urination due to glucose in urine), which might paradoxically make patients more aware of normal urination patterns if they were previously experiencing polyuria due to uncontrolled hyperglycaemia.
Increased fluid intake: Patients experiencing nausea or following dietary advice may increase water consumption, naturally leading to more frequent urination.
Co-prescribed medications: SGLT2 inhibitors (such as dapagliflozin, empagliflozin) commonly cause increased urination as their primary mechanism of action. Diuretics also directly increase urine output. If you're taking these alongside GLP-1 therapy, they may be responsible for urinary changes.
Urinary tract symptoms: Whilst uncommon, some patients report urinary tract infections or bladder discomfort, though these are not established as direct drug effects of GLP-1 medications.
Clinical trials have not identified increased urination as a significant adverse event requiring specific monitoring for GLP-1 receptor agonists. If you experience marked changes in urinary habits, this warrants discussion with your healthcare provider to rule out other causes.
When Frequent Urination on GLP-1 Treatment Needs Medical Attention
Whilst mild changes in urination patterns may be a temporary adjustment to GLP-1 therapy, certain symptoms require prompt medical evaluation. Contact your GP or diabetes specialist nurse if you experience:
-
Excessive thirst combined with frequent urination: This may indicate worsening glycaemic control or inadequate diabetes management, requiring blood glucose monitoring and potential treatment adjustment.
-
Pain or burning during urination: These symptoms suggest a possible urinary tract infection (UTI), which requires antibiotic treatment.
-
Blood in the urine (haematuria): This always warrants investigation. According to NICE guidance (NG12), visible blood in urine requires urgent referral (within 2 weeks) for people aged 45 and over to exclude urological cancer. Non-visible haematuria with other symptoms also needs assessment.
-
Inability to empty the bladder completely: Urinary retention or difficulty passing urine requires urgent assessment.
-
Sudden onset of severe urinary frequency with lower abdominal pain: This may indicate acute cystitis or other bladder pathology.
Seek immediate medical attention (call 999 or attend A&E) if you develop:
-
Signs of severe dehydration: dizziness, confusion, reduced urine output despite drinking fluids, rapid heartbeat
-
Symptoms of diabetic ketoacidosis: excessive thirst, frequent urination, nausea, vomiting, abdominal pain, fruity-smelling breath, confusion (Note: GLP-1 medications do not cause DKA, but it can occur in type 1 diabetes or ketosis-prone type 2 diabetes, especially during illness)
-
Severe flank pain with fever: may indicate pyelonephritis (kidney infection)
If you experience persistent vomiting or diarrhoea from GLP-1 therapy and cannot maintain adequate fluid intake, seek urgent medical advice as there is a risk of dehydration and acute kidney injury.
According to NICE guidance on diabetes management (NG28), any significant change in symptoms whilst on diabetes medication should be reviewed to ensure treatment remains appropriate and effective.
Managing Increased Urination While Taking GLP-1 Medications
If you are experiencing increased urination whilst taking GLP-1 medication, several practical strategies can help manage this symptom whilst ensuring your treatment remains effective:
Monitor your fluid intake: Maintain adequate hydration (NHS recommends 6-8 cups or glasses of fluid per day for most adults) but avoid excessive fluid consumption unless medically advised. Drinking appropriate amounts helps prevent dehydration without unnecessarily increasing urinary frequency.
Time your fluid intake strategically: If nighttime urination (nocturia) is problematic, reduce fluid intake in the 2–3 hours before bedtime whilst ensuring adequate hydration throughout the day.
Keep a symptom diary: Record your urination frequency, fluid intake, and blood glucose readings for 1–2 weeks. This information helps your healthcare team identify patterns and determine whether symptoms relate to medication, diabetes control, or other factors.
Review your blood glucose control: Check your HbA1c and daily glucose readings with your diabetes team. If glucose levels have improved significantly, your body may be adjusting to better metabolic control, and urinary symptoms may be temporary.
Pelvic floor exercises: If urinary urgency is problematic, pelvic floor muscle training (Kegel exercises) can improve bladder control. The NHS provides guidance on these exercises, and your GP can refer you to a physiotherapist specialising in continence if needed.
Avoid bladder irritants: Caffeine, alcohol, artificial sweeteners, and acidic foods can increase urinary frequency. Moderating these may help reduce symptoms.
Review other medications: If you're also taking SGLT2 inhibitors or diuretics, discuss with your healthcare provider whether these might be contributing to increased urination and if adjustments are appropriate.
Do not discontinue medication without medical advice: GLP-1 receptor agonists provide important therapeutic benefits for diabetes control and cardiovascular risk reduction. If side effects are troublesome, discuss alternatives with your prescriber rather than stopping treatment independently.
Other Factors That May Affect Urination During GLP-1 Therapy
Several concurrent factors may influence urinary patterns in patients taking GLP-1 medications, and it is important to consider these when evaluating symptoms:
Concomitant medications: Many patients on GLP-1 therapy take other medications that affect urination. Diuretics (commonly prescribed for hypertension or heart failure) directly increase urine production. SGLT2 inhibitors (such as dapagliflozin or empagliflozin), often co-prescribed with GLP-1 agonists for diabetes management, work by increasing glucose excretion in urine, which increases urinary frequency as an expected and common pharmacological effect. If you have recently started or adjusted doses of these medications, they may be the primary cause of increased urination.
Dietary changes: Patients starting GLP-1 therapy often make significant dietary modifications, including increased vegetable and fruit consumption (which have high water content) and reduced processed food intake. These healthy changes naturally increase fluid intake and may affect urination patterns.
Weight loss and metabolic changes: Substantial weight reduction alters body composition and fluid balance. Additionally, improved insulin sensitivity may affect renal sodium handling and fluid balance.
Age-related factors: Many patients prescribed GLP-1 medications are middle-aged or older, demographics where benign prostatic hyperplasia (in men) and overactive bladder syndrome (in both sexes) become more prevalent. These conditions may coincidentally develop or worsen during GLP-1 treatment without being causally related.
Underlying kidney function: Some GLP-1 receptor agonists have shown benefits for renal outcomes in clinical trials, though this varies by specific medication. NICE recommends monitoring renal function in patients with diabetes, particularly when initiating or adjusting glucose-lowering therapies.
Sick day management: If you experience significant gastrointestinal side effects from GLP-1 therapy, follow sick day rules to prevent dehydration. Contact your healthcare provider if you cannot maintain adequate fluid intake, as this may increase the risk of acute kidney injury.
If you believe you're experiencing side effects from your medication, you can report them through the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
If increased urination persists or concerns you, request a comprehensive medication review with your GP or pharmacist to identify potential contributing factors and optimise your treatment regimen accordingly.
Frequently Asked Questions
Do GLP-1 medications like Ozempic cause increased urination?
No, increased urination is not a recognised side effect of GLP-1 receptor agonists according to MHRA guidance. When it occurs, it typically results from improved glucose control, increased fluid intake, or co-prescribed medications such as SGLT2 inhibitors or diuretics rather than the GLP-1 medication itself.
When should I see a doctor about frequent urination on GLP-1 treatment?
Contact your GP if you experience excessive thirst with frequent urination, pain or burning during urination, blood in urine, or inability to empty your bladder completely. Seek immediate medical attention for signs of severe dehydration, diabetic ketoacidosis, or severe flank pain with fever.
How can I manage increased urination whilst taking GLP-1 medications?
Maintain adequate hydration (6–8 glasses daily), time fluid intake to reduce nighttime urination, keep a symptom diary, review blood glucose control with your healthcare team, and consider pelvic floor exercises if urgency is problematic. Always discuss persistent symptoms with your GP rather than stopping medication independently.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript