Emerging research has sparked interest in whether GLP-1 receptor agonists—medications primarily used for type 2 diabetes and weight management—might influence alcohol consumption. Whilst preliminary studies suggest these medications may reduce drinking in some individuals, the evidence remains limited and inconclusive. GLP-1 medications are not approved for treating alcohol use disorder, and any effects on drinking behaviour are incidental rather than therapeutic. This article examines the current evidence, explores potential mechanisms, and outlines important safety considerations for patients taking these medications who consume alcohol.
Summary: GLP-1 receptor agonists may reduce alcohol consumption in some individuals, but they are not approved for treating alcohol use disorder and evidence remains preliminary.
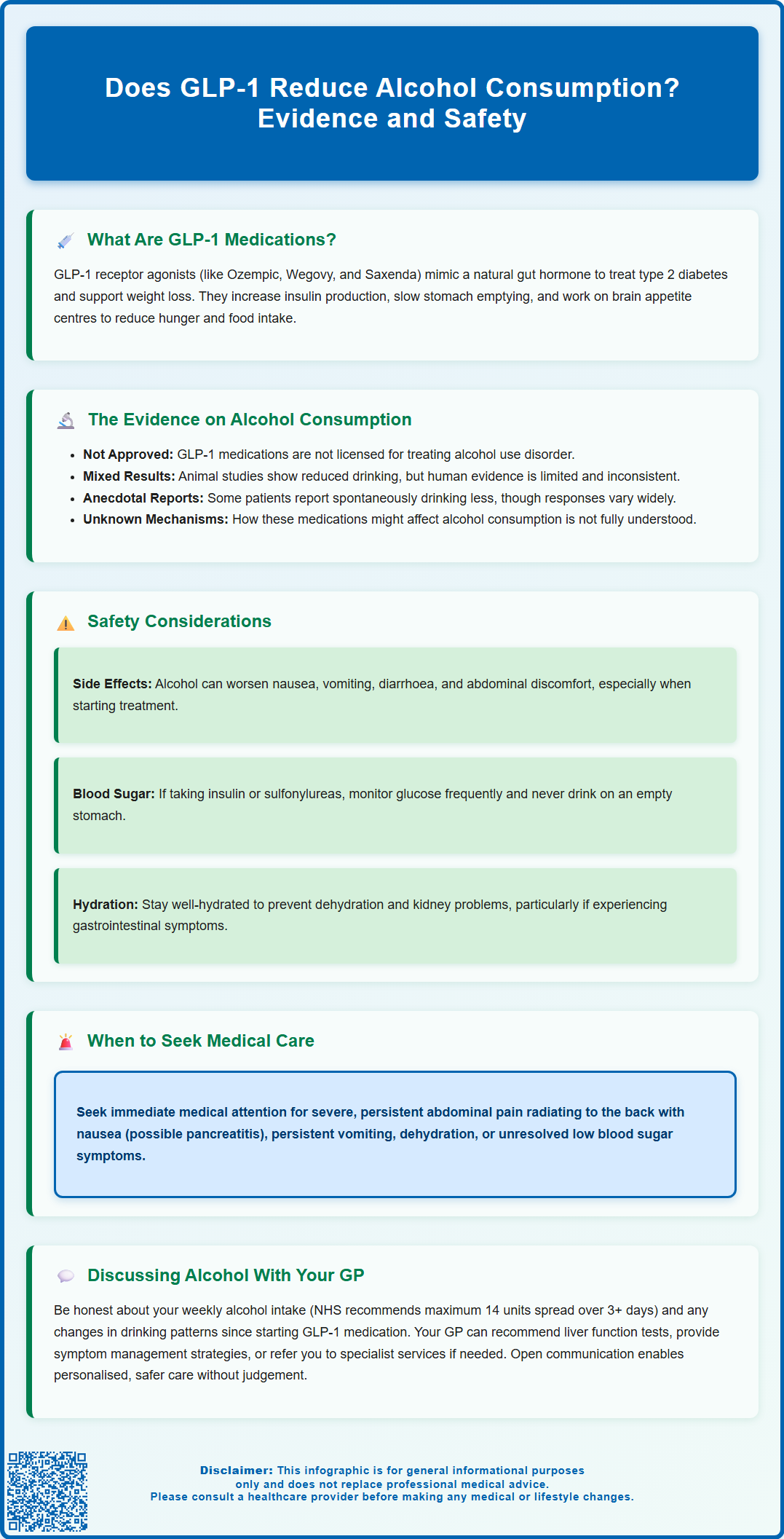
- GLP-1 medications mimic a natural hormone that regulates blood glucose, slows gastric emptying, and acts on brain appetite centres.
- Animal studies show reduced alcohol intake with GLP-1 medications, but human evidence is limited and mixed.
- These medications are not licensed by the MHRA for alcohol use disorder and should not replace specialist addiction services.
- Alcohol may worsen common GLP-1 side effects including nausea, vomiting, and gastrointestinal discomfort.
- Patients with diabetes taking GLP-1 medications should monitor blood glucose carefully when consuming alcohol due to hypoglycaemia risk.
- Severe abdominal pain whilst taking GLP-1 medications requires urgent medical assessment to exclude pancreatitis.
Table of Contents
What Are GLP-1 Medications and How Do They Work?
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications primarily prescribed for the management of type 2 diabetes mellitus and, more recently, for weight management in adults with obesity or overweight with weight-related comorbidities. Common examples available in the UK include semaglutide (injectable as Ozempic, Wegovy; oral as Rybelsus), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda).
These medications work by mimicking the action of naturally occurring GLP-1, a hormone released by the intestine in response to food intake. The primary mechanisms of action include:
-
Enhancing insulin secretion from pancreatic beta cells in a glucose-dependent manner, which helps lower blood glucose levels without causing hypoglycaemia when used alone
-
Suppressing glucagon release from pancreatic alpha cells, reducing hepatic glucose production
-
Slowing gastric emptying, which prolongs the feeling of fullness after meals
-
Acting on appetite centres in the brain, particularly the hypothalamus, to reduce hunger and food intake
GLP-1 receptor agonists are typically administered via subcutaneous injection, with dosing frequencies ranging from once daily to once weekly depending on the specific medication, though oral semaglutide (Rybelsus) is also available. According to NICE guidance (NG28), these medications have demonstrated significant benefits in glycaemic control, with some specific agents (semaglutide, liraglutide, dulaglutide) also showing cardiovascular risk reduction in clinical trials. The appetite-suppressing effects occur through complex interactions with the central nervous system, which has led researchers to hypothesise that these medications might influence other reward-driven behaviours, including alcohol consumption. This emerging area of research has generated considerable interest among clinicians and patients alike.
Does GLP-1 Reduce Alcohol Consumption? Current Evidence
Emerging research suggests that GLP-1 receptor agonists may influence alcohol consumption patterns, though there is no official indication for these medications in treating alcohol use disorder, and the evidence base remains preliminary. The interest in this potential effect stems from the understanding that GLP-1 receptors are present in brain regions associated with reward processing and addictive behaviours.
Preclinical and clinical evidence includes several noteworthy findings. Animal studies have consistently demonstrated that GLP-1 receptor agonists reduce alcohol intake in rodent models of alcohol consumption. In human studies, the evidence is mixed. A randomised controlled trial of exenatide once-weekly in alcohol use disorder showed mixed results overall, with possible effects in certain subgroups. Additionally, some individuals taking these medications for diabetes or weight management have reported spontaneously reduced alcohol intake in observational studies.
However, significant limitations exist in the current evidence:
-
Most human data comes from small studies, with limited randomised controlled trials specifically designed to assess alcohol consumption
-
The mechanisms by which GLP-1 medications might reduce alcohol intake are not fully understood
-
Individual responses vary considerably, and not all patients experience changes in drinking behaviour
-
Long-term effects and safety of using these medications specifically for alcohol reduction remain unknown
The MHRA has not approved GLP-1 receptor agonists for alcohol use disorder, and these medications should not be considered a treatment for problematic drinking. Patients concerned about alcohol consumption should be referred to appropriate addiction services. Whilst the preliminary findings are intriguing and warrant further investigation through properly designed clinical trials, clinicians should counsel patients that any effects on alcohol intake are incidental rather than therapeutic indications.
Safety Considerations: GLP-1 Medications and Alcohol Use
Understanding the safety profile of GLP-1 receptor agonists in the context of alcohol consumption is essential for both patients and healthcare professionals. Whilst there is no absolute contraindication to consuming alcohol whilst taking GLP-1 medications, several important considerations warrant careful attention.
Gastrointestinal effects represent the most common concern. GLP-1 receptor agonists frequently cause nausea, vomiting, diarrhoea, and abdominal discomfort, particularly during dose titration. Alcohol consumption can exacerbate these gastrointestinal side effects, potentially leading to increased discomfort, dehydration, and poor medication tolerance. The delayed gastric emptying caused by these medications may also alter alcohol absorption patterns, though the clinical significance of this interaction remains unclear.
Hypoglycaemia risk requires consideration, particularly in patients with type 2 diabetes taking GLP-1 medications alongside insulin or sulfonylureas. Alcohol consumption can impair hepatic gluconeogenesis and mask hypoglycaemic symptoms. Patients should be advised to:
-
Monitor blood glucose levels more frequently if consuming alcohol
-
Avoid drinking on an empty stomach
-
Be aware of delayed hypoglycaemia, which can occur several hours after drinking
-
Ensure companions recognise signs of hypoglycaemia
Pancreatitis is a rare but serious adverse effect associated with GLP-1 receptor agonists. Excessive alcohol consumption is itself a risk factor for acute pancreatitis. If pancreatitis is suspected (severe, persistent abdominal pain, particularly if radiating to the back, accompanied by nausea and vomiting), the GLP-1 medication should be discontinued immediately and urgent medical assessment sought. The combination of a GLP-1 medication and heavy alcohol use may theoretically increase pancreatitis risk, though definitive evidence for this interaction is lacking.
Gallbladder disease risk may be increased with GLP-1 receptor agonists, particularly with substantial weight loss. Alcohol can exacerbate gallbladder symptoms, and patients should seek medical attention for right upper quadrant pain or other biliary symptoms.
Patients should maintain adequate hydration, especially if experiencing gastrointestinal side effects, to reduce the risk of acute kidney injury. Any suspected side effects should be reported via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
What to Discuss With Your GP About GLP-1 and Alcohol
Open communication with your GP about alcohol consumption is crucial when considering or taking GLP-1 medications. Honest disclosure of drinking patterns enables your healthcare provider to assess potential risks, optimise treatment, and provide appropriate monitoring and support.
Key topics to raise during your consultation include:
-
Your current alcohol intake: Be specific about the number of units consumed weekly. The NHS recommends not regularly drinking more than 14 units per week, spread over three or more days. Your GP can help you calculate your consumption accurately and may use screening tools like AUDIT-C to assess your drinking patterns.
-
Any history of alcohol-related health problems, including liver disease, pancreatitis, gastritis, or previous attempts to reduce drinking
-
Changes in drinking patterns since starting GLP-1 medication, whether increased or decreased consumption, or altered tolerance to alcohol
-
Gastrointestinal symptoms and whether alcohol worsens nausea, vomiting, or other side effects
-
Concerns about alcohol use disorder: If you're finding it difficult to control your drinking, your GP can arrange referral to specialist NHS alcohol services
Your GP should provide personalised advice based on your individual circumstances, including other medications, comorbidities, and treatment goals. They may recommend:
-
Liver function tests based on clinical judgement and your overall risk profile
-
Strategies to minimise gastrointestinal side effects
-
Referral to diabetes specialist nurses for education on hypoglycaemia prevention
-
Signposting to alcohol support services if appropriate
When to contact your GP urgently: Seek medical advice promptly if you experience severe abdominal pain (stop your GLP-1 medication if pancreatitis is suspected), persistent vomiting preventing medication or fluid intake, signs of dehydration, or symptoms of hypoglycaemia that don't resolve with usual measures. If you're concerned about your alcohol consumption or experiencing withdrawal symptoms, contact your GP practice or NHS 111 for guidance. Remember that your healthcare team is there to support you without judgement, and honest conversations lead to safer, more effective care.
Frequently Asked Questions
Can I drink alcohol whilst taking GLP-1 medications?
There is no absolute contraindication to consuming alcohol whilst taking GLP-1 medications, but alcohol may worsen gastrointestinal side effects such as nausea and vomiting. Patients with diabetes should monitor blood glucose carefully, as alcohol can increase hypoglycaemia risk, particularly when combined with insulin or sulfonylureas.
Are GLP-1 medications approved for treating alcohol use disorder?
No, GLP-1 receptor agonists are not approved by the MHRA for treating alcohol use disorder. Whilst emerging research suggests they may influence drinking patterns in some individuals, these medications should not be considered a treatment for problematic alcohol consumption, and patients should be referred to appropriate addiction services.
What should I do if I experience severe abdominal pain whilst taking GLP-1 medication and drinking alcohol?
Stop your GLP-1 medication immediately and seek urgent medical assessment, as severe abdominal pain may indicate pancreatitis, a rare but serious side effect. Both GLP-1 medications and excessive alcohol consumption are risk factors for pancreatitis, and the combination may theoretically increase this risk.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












