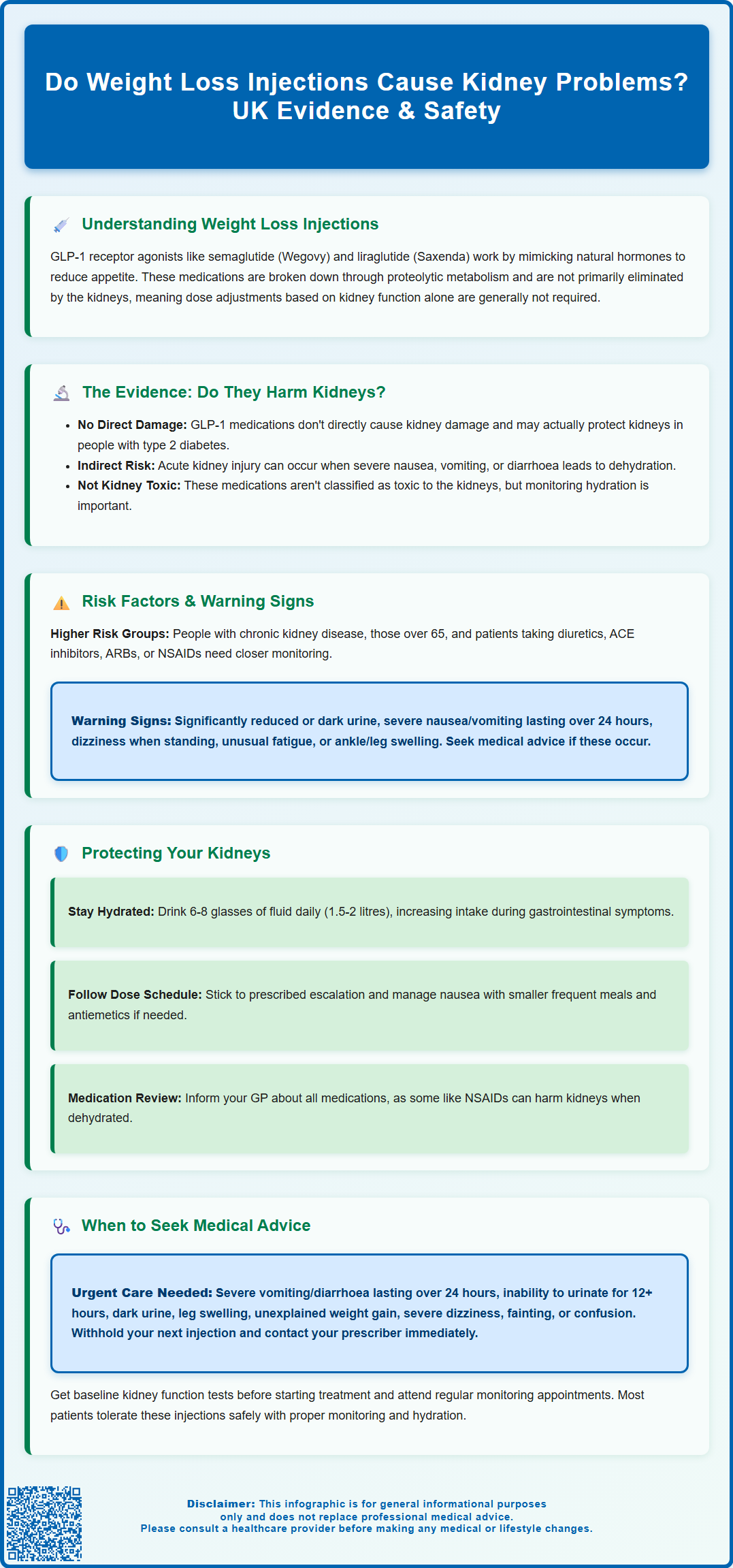
Weight loss injections, particularly GLP-1 receptor agonists like semaglutide (Wegovy) and liraglutide (Saxenda), are increasingly prescribed in the UK for obesity management. Many patients wonder: do weight loss injections cause kidney problems? Understanding the relationship between these medications and kidney function is essential for safe treatment. Current evidence suggests these injections do not directly damage kidneys in most patients. However, severe gastrointestinal side effects—such as persistent vomiting or diarrhoea—can lead to dehydration, which may indirectly affect kidney function. This article examines the evidence, identifies risk factors, and provides practical guidance on protecting kidney health during weight loss injection treatment.
Summary: Weight loss injections do not directly cause kidney problems in most patients, though severe dehydration from gastrointestinal side effects may indirectly affect kidney function.
- GLP-1 receptor agonists like semaglutide and liraglutide are not primarily cleared by the kidneys and do not directly damage renal tissue.
- Acute kidney injury may occur as a secondary consequence of severe dehydration from persistent vomiting or diarrhoea, not from direct drug toxicity.
- Clinical trials have demonstrated potential renoprotective effects in patients with type 2 diabetes, including reduced albuminuria and slowed progression of diabetic kidney disease.
- Patients with pre-existing chronic kidney disease, advanced age, or concurrent use of medications affecting kidney function require enhanced monitoring during treatment.
- Maintaining adequate hydration, managing gastrointestinal side effects, and attending scheduled monitoring appointments are essential for kidney safety during treatment.
Table of Contents
Understanding Weight Loss Injections and Kidney Function
Weight loss injections, particularly glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), have become increasingly prescribed in the UK for weight management in adults with obesity or overweight with weight-related comorbidities. These medications work by mimicking natural hormones that regulate appetite and blood glucose levels, leading to reduced food intake and subsequent weight loss. Unlike many medications, GLP-1 receptor agonists used for weight management undergo proteolytic metabolism similar to endogenous peptides, with minimal unchanged renal excretion.
The kidneys play an important role in overall drug metabolism and elimination, though semaglutide and liraglutide are not primarily cleared by the kidneys. Healthy kidney function is typically defined by an estimated glomerular filtration rate (eGFR) above 90 mL/min/1.73m² without evidence of kidney damage, whilst chronic kidney disease (CKD) is classified into stages based on declining eGFR values and the presence of albuminuria, as outlined in NICE guideline NG203. When kidney function is impaired, the body's ability to process and eliminate some medications may be affected, though dose adjustments for weight loss injections are generally not required based on renal function alone.
For individuals considering weight loss injections, assessment of kidney function may be considered, particularly in those with risk factors for kidney disease or who develop significant gastrointestinal symptoms during treatment. In the UK, NICE technology appraisals TA875 (semaglutide) and TA664 (liraglutide) outline specific eligibility criteria, including BMI thresholds and the requirement for specialist weight management services. The Summary of Product Characteristics (SmPC) for these medications provides guidance on their use in various patient populations, emphasising individualised risk assessment before initiating treatment. Understanding the relationship between weight loss injections and kidney function enables informed decision-making and appropriate clinical vigilance throughout the treatment journey.
Do Weight Loss Injections Cause Kidney Problems?
The relationship between weight loss injections and kidney problems is complex and requires careful examination of available evidence. Current research suggests that GLP-1 receptor agonists do not directly cause kidney damage in most patients. In fact, several large-scale clinical trials have demonstrated potential renoprotective effects, particularly in individuals with type 2 diabetes. Studies such as LEADER (liraglutide), SUSTAIN-6 (semaglutide), and REWIND (dulaglutide) have shown that these medications may slow the progression of diabetic kidney disease and reduce albuminuria (protein in the urine), which is a marker of kidney damage. However, it's important to note that these renoprotective effects are primarily observed in diabetes populations and are not licensed renal indications.
While there is no evidence that weight loss injections directly cause kidney problems in individuals with normal baseline renal function, the SmPCs for both Wegovy and Saxenda do list acute kidney injury (AKI) and renal impairment among reported adverse reactions. These events are typically associated with severe gastrointestinal side effects. GLP-1 receptor agonists commonly cause nausea, vomiting, and diarrhoea, particularly during the initial weeks of treatment or following dose escalation. When these symptoms are severe and prolonged, they can lead to dehydration and volume depletion, which may precipitate acute kidney injury as a secondary consequence rather than a direct drug effect on renal tissue.
The MHRA has received post-marketing reports of renal impairment and acute renal failure in patients taking GLP-1 receptor agonists, but these cases have typically occurred in the context of significant dehydration, pre-existing kidney disease, or concurrent use of other medications affecting kidney function. It is important to distinguish between direct nephrotoxicity (kidney damage caused by the drug itself) and indirect effects mediated through dehydration or other mechanisms. Current evidence does not support the classification of weight loss injections as nephrotoxic agents, though vigilance regarding hydration status and kidney function monitoring remains clinically prudent throughout treatment, particularly if severe gastrointestinal symptoms occur.
Risk Factors and Warning Signs to Monitor
Certain individuals face elevated risks when using weight loss injections, necessitating enhanced monitoring and clinical awareness. Pre-existing chronic kidney disease represents a significant risk factor, as reduced renal function may increase susceptibility to volume depletion. According to the SmPCs, there is limited experience with semaglutide and liraglutide in severe renal impairment, with liraglutide not recommended in end-stage renal disease and semaglutide to be used with caution in severe impairment. Additional risk factors include advanced age (over 65 years), concurrent use of diuretics or medications affecting kidney function (such as ACE inhibitors, ARBs, or NSAIDs), diabetes with diabetic nephropathy, and cardiovascular disease. Individuals taking multiple medications that affect fluid balance or kidney perfusion require particularly careful assessment and monitoring.
Recognising warning signs of potential kidney problems is essential for patient safety. Symptoms suggesting dehydration or acute kidney injury include significantly reduced urine output or dark-coloured urine, persistent severe nausea or vomiting lasting more than 24 hours, inability to maintain adequate fluid intake, dizziness or lightheadedness when standing, unusual fatigue or weakness, and swelling of the ankles or legs. It is important to note that early kidney problems may be asymptomatic, which is why monitoring is important, particularly in high-risk individuals.
The frequency of kidney function monitoring should be individualised based on risk factors and follow established guidelines such as NICE NG203 for those with known CKD. For patients with normal baseline kidney function and no risk factors, routine monitoring may be sufficient. However, those with pre-existing kidney disease, multiple risk factors, or experiencing significant gastrointestinal side effects should undergo more frequent assessment as clinically indicated. Following 'sick day rules' is advisable – temporarily withholding the injection and contacting a healthcare professional if unable to maintain adequate hydration due to vomiting or diarrhoea. Importantly, patients should not stop other medications such as ACE inhibitors, ARBs or diuretics without clinical advice, even during illness, as this requires individualised assessment.
Protecting Your Kidneys While Using Weight Loss Injections
Maintaining optimal kidney health whilst using weight loss injections requires a proactive approach centred on adequate hydration and symptom management. Ensuring sufficient fluid intake is important, particularly during the initial treatment phase when gastrointestinal side effects are most pronounced. The NHS recommends adults aim for about 6-8 glasses of fluid daily (approximately 1.5-2 litres), though individual requirements vary based on body size, activity level, and climate. Those with heart failure or advanced kidney disease should follow their clinician's specific fluid intake advice. During episodes of nausea, vomiting, or diarrhoea, fluid intake should be increased to compensate for losses. Small, frequent sips of water, oral rehydration solutions, or clear fluids may be better tolerated than large volumes consumed at once.
Managing gastrointestinal side effects effectively reduces the risk of dehydration-related kidney complications. Following the dose escalation schedule outlined in the SmPC is important for minimising side effects. Strategies include eating smaller, more frequent meals, avoiding high-fat and spicy foods that may exacerbate nausea, and taking the injection at a time of day when side effects are most manageable. If nausea or vomiting becomes severe, antiemetic medications prescribed by a GP can provide relief and enable adequate fluid intake. If experiencing severe gastrointestinal symptoms with signs of dehydration, it may be appropriate to withhold the next dose and seek medical advice.
Regular medication review with healthcare professionals helps identify and manage potential drug interactions that could affect kidney function. Patients should inform their GP and pharmacist about all medications, including over-the-counter products and supplements. Particular caution is warranted with NSAIDs (such as ibuprofen), which can affect kidney function, especially when combined with dehydration – seek pharmacist or GP advice before using these medications if you're experiencing gastrointestinal symptoms. Maintaining a healthy lifestyle supports kidney function: following a balanced diet with appropriate protein intake, limiting salt consumption, avoiding excessive alcohol, not smoking, and engaging in regular physical activity all contribute to renal health. Attending scheduled monitoring appointments enables early detection of any kidney function changes, allowing for timely intervention if needed.
When to Seek Medical Advice About Kidney Health
Understanding when to contact healthcare services is crucial for preventing serious kidney complications during weight loss injection treatment. Urgent medical attention is required if you experience severe, persistent vomiting or diarrhoea lasting more than 24 hours that prevents adequate fluid intake, as this can rapidly lead to dehydration and acute kidney injury. Similarly, a marked decrease in urine output (especially if unable to pass urine for 12+ hours), dark-coloured urine, swelling of the legs or ankles, significant unexplained weight gain, severe dizziness, fainting, or confusion warrants prompt medical assessment. These symptoms may indicate fluid retention, declining kidney function, or severe dehydration requiring immediate evaluation. Contact your GP, NHS 111, or emergency services as appropriate if you develop these symptoms.
Routine medical review is equally important for ongoing kidney health monitoring. Patients should schedule appointments with their GP or prescribing clinician before starting weight loss injections to establish baseline kidney function if indicated, and subsequently as recommended based on individual risk factors. Any new symptoms, even if seemingly minor, should be discussed at these appointments rather than dismissed. According to NICE guideline NG203, nephrology referral should be considered for patients with eGFR <30 mL/min/1.73m², albumin:creatinine ratio ≥70 mg/mmol, sustained decline in eGFR, persistent haematuria with elevated albumin:creatinine ratio, or resistant hypertension. If you have pre-existing kidney disease, diabetes, or cardiovascular conditions, monitoring should follow established clinical guidelines.
It is important to maintain open communication with healthcare professionals throughout treatment. If you experience severe gastrointestinal symptoms or dehydration, it may be appropriate to withhold your next dose and contact your prescriber for advice, rather than continuing treatment while severely unwell. If kidney function tests show declining eGFR or rising creatinine levels, your clinician will discuss whether treatment modification, temporary suspension, or discontinuation is appropriate. The decision-making process considers the overall benefit-risk balance, including the metabolic benefits of weight loss against any potential kidney concerns. Remember that most patients tolerate weight loss injections well without kidney complications when appropriate monitoring and precautions are in place. Your healthcare team is your partner in ensuring safe, effective treatment, and seeking timely advice when concerns arise is always the right approach.
Scientific References
- Saxenda 6 mg/mL solution for injection in pre-filled pen - Summary of Product Characteristics.
- Wegovy 0.25 mg, FlexTouch solution for injection in pre-filled pen - Summary of Product Characteristics.
- Chronic kidney disease: assessment and management. NICE guideline NG203.
- Liraglutide and Renal Outcomes in Type 2 Diabetes (LEADER trial).
- Semaglutide and Cardiovascular Outcomes in Patients with Type 2 Diabetes (SUSTAIN-6 trial).
- Dulaglutide and Kidney Function-Related Outcomes in Type 2 Diabetes: A REWIND Post Hoc Analysis.
- Wegovy - European Public Assessment Report.
- Obesity - Treatment.
Frequently Asked Questions
Can weight loss injections like Wegovy damage your kidneys?
Weight loss injections do not directly damage kidneys in most patients. However, severe gastrointestinal side effects such as persistent vomiting or diarrhoea can cause dehydration, which may indirectly lead to acute kidney injury if not managed promptly.
Who is at higher risk of kidney problems when using weight loss injections?
Individuals with pre-existing chronic kidney disease, advanced age (over 65), diabetes with diabetic nephropathy, or those taking medications affecting kidney function (such as ACE inhibitors, ARBs, diuretics, or NSAIDs) face elevated risks and require enhanced monitoring during treatment.
What warning signs suggest kidney problems during weight loss injection treatment?
Warning signs include significantly reduced or dark-coloured urine, persistent severe nausea or vomiting lasting more than 24 hours, inability to maintain adequate fluid intake, dizziness when standing, unusual fatigue, and swelling of the ankles or legs. Seek medical advice promptly if these symptoms develop.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












