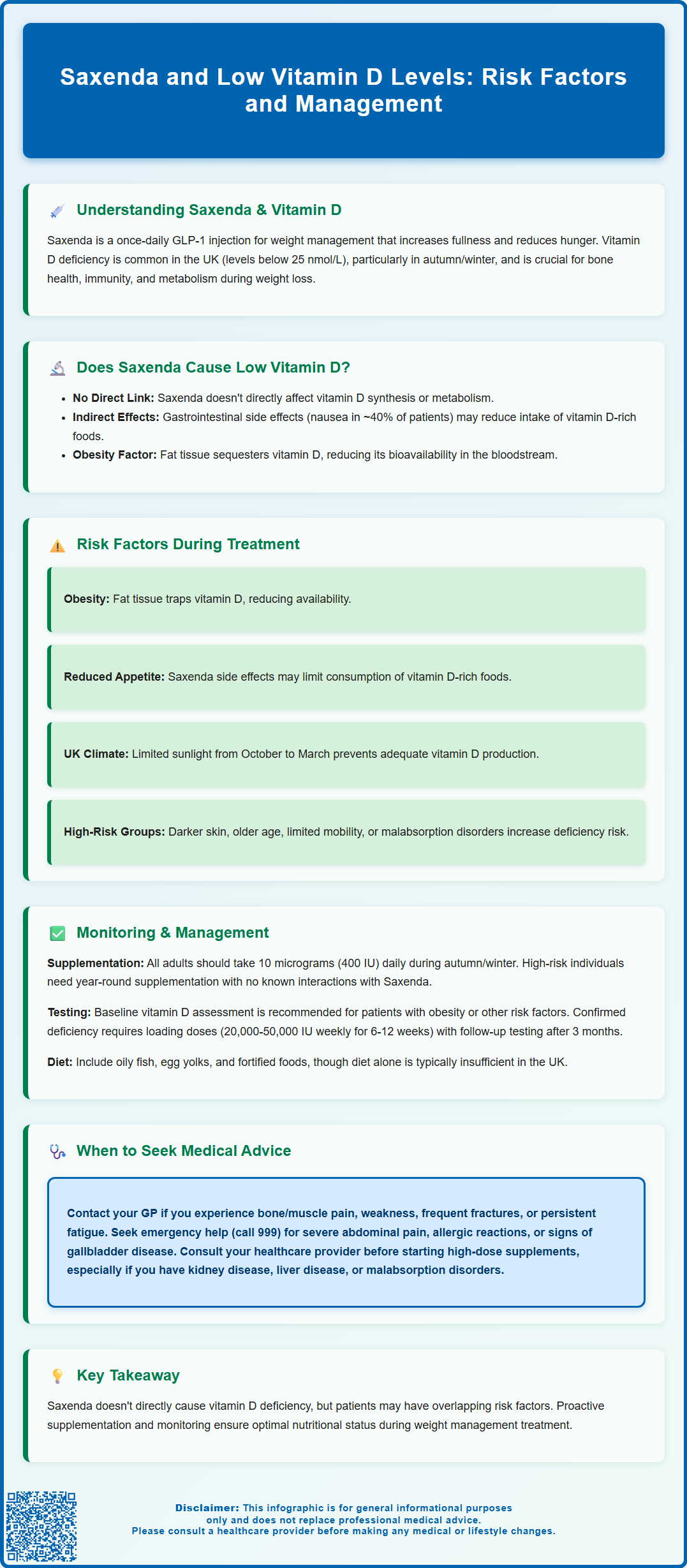
Saxenda (liraglutide 3.0 mg) is a GLP-1 receptor agonist prescribed for weight management in adults and adolescents with obesity or overweight with comorbidities. Whilst Saxenda and low vitamin D levels may occur together in some patients, there is no established evidence that Saxenda directly causes vitamin D deficiency. However, factors associated with obesity and weight management treatment—including reduced dietary intake due to gastrointestinal side effects, pre-existing vitamin D sequestration in adipose tissue, and limited sun exposure—may contribute to low vitamin D status. Understanding this relationship helps patients and healthcare professionals optimise nutritional health during Saxenda therapy.
Summary: Saxenda does not directly cause low vitamin D levels, but patients may have multiple risk factors for deficiency related to obesity, gastrointestinal side effects, and reduced dietary intake.
- Saxenda (liraglutide) is a GLP-1 receptor agonist licensed for weight management in adults and adolescents with obesity or overweight with comorbidities.
- No established mechanism exists by which Saxenda causes vitamin D deficiency, and it is not listed as a known side effect in the Summary of Product Characteristics.
- Obesity itself is associated with lower circulating vitamin D due to sequestration in adipose tissue, reducing bioavailability.
- Gastrointestinal side effects such as nausea and vomiting may reduce dietary intake of vitamin D-rich foods during Saxenda treatment.
- NHS guidance recommends all UK adults consider taking 10 micrograms (400 IU) vitamin D daily during autumn and winter, with year-round supplementation for at-risk groups.
- Patients with multiple risk factors for deficiency should discuss vitamin D monitoring and supplementation with their healthcare provider before or during Saxenda treatment.
Table of Contents
Understanding Saxenda and Vitamin D Deficiency
Saxenda (liraglutide 3.0 mg) is a prescription-only glucagon-like peptide-1 (GLP-1) receptor agonist licensed in the UK for weight management. It is indicated for adults with a body mass index (BMI) of 30 kg/m² or greater, or 27 kg/m² or greater with weight-related comorbidities, and for adolescents aged 12-17 years with obesity. Administered as a once-daily subcutaneous injection, Saxenda must be used as part of a structured weight management programme including a reduced-calorie diet and increased physical activity. It works by mimicking the action of the naturally occurring hormone GLP-1, which regulates appetite and food intake. By activating GLP-1 receptors in the brain, Saxenda increases feelings of fullness, reduces hunger, and slows gastric emptying, thereby supporting calorie reduction and weight loss.
Vitamin D is a fat-soluble vitamin essential for calcium absorption, bone health, immune function, and numerous metabolic processes. In the UK, vitamin D deficiency is common, particularly during autumn and winter months when sunlight exposure is limited. According to the Scientific Advisory Committee on Nutrition (SACN), deficiency is defined by serum 25-hydroxyvitamin D (25(OH)D) concentrations below 25 nmol/L, with insufficiency typically considered at levels between 25–50 nmol/L. Risk factors include limited sun exposure, darker skin pigmentation, obesity, older age, and certain dietary patterns.
Patients considering or currently using Saxenda may have concerns about potential interactions between the medication and their vitamin D status. Understanding whether Saxenda directly affects vitamin D levels, or whether other factors associated with weight management treatment contribute to deficiency, is important for maintaining overall health during weight loss therapy. This article examines the relationship between Saxenda treatment and vitamin D levels, providing evidence-based guidance for patients and healthcare professionals.
Can Saxenda Cause Low Vitamin D Levels?
Currently, there is no established evidence or mechanism by which Saxenda (liraglutide) causes vitamin D deficiency. The drug's primary action on GLP-1 receptors does not appear to interfere with vitamin D synthesis in the skin, absorption in the gastrointestinal tract, or metabolism in the liver and kidneys. The Saxenda Summary of Product Characteristics (SmPC) does not list vitamin D deficiency among known side effects.
However, several indirect factors associated with Saxenda treatment may influence vitamin D levels. The medication commonly causes gastrointestinal adverse effects, including nausea (reported in approximately 40% of patients according to the SmPC), vomiting, diarrhoea, and constipation, particularly during dose escalation. These symptoms may lead to reduced dietary intake or altered eating patterns, potentially decreasing consumption of vitamin D-rich foods such as oily fish, eggs, and fortified products like some breakfast cereals and spreads. Additionally, if gastrointestinal symptoms are severe, they could theoretically affect the absorption of fat-soluble vitamins, including vitamin D, though this has not been specifically documented in clinical trials.
It is important to note that obesity itself is associated with lower circulating vitamin D levels. Vitamin D is sequestered in adipose tissue, and individuals with higher body fat percentages often demonstrate reduced bioavailability of vitamin D. Some research suggests that as patients lose weight, vitamin D stored in fat tissue may be released, potentially affecting vitamin D status, though the clinical significance of this remains uncertain.
Risk Factors for Vitamin D Deficiency During Saxenda Treatment
While Saxenda itself does not directly cause vitamin D deficiency, patients using this medication may have multiple overlapping risk factors that predispose them to low vitamin D levels. Understanding these factors helps identify individuals who may benefit from monitoring or supplementation.
Obesity-related factors are particularly relevant, as patients prescribed Saxenda typically have a BMI of 30 kg/m² or above. Excess adipose tissue sequesters vitamin D, reducing its bioavailability in the circulation. Furthermore, individuals with obesity may have reduced outdoor physical activity and sun exposure, limiting cutaneous vitamin D synthesis. Dietary patterns associated with weight gain often include lower consumption of vitamin D-rich foods.
Gastrointestinal symptoms induced by Saxenda may contribute to inadequate nutritional intake. Persistent nausea, early satiety, or food aversions can lead to a restricted diet that may not provide sufficient vitamin D. Patients who experience prolonged gastrointestinal disturbances should be particularly mindful of maintaining adequate nutrition, including vitamin D intake through diet or supplementation.
Seasonal and geographical factors significantly affect vitamin D status in the UK. Between October and March, sunlight intensity is insufficient for adequate vitamin D synthesis, and the NHS recommends that all adults consider taking a daily supplement containing 10 micrograms (400 IU) of vitamin D during these months. Certain groups should take 10 micrograms year-round, including pregnant and breastfeeding women, care home residents, and those with minimal sun exposure. Patients with darker skin require longer sun exposure to produce equivalent amounts of vitamin D and are at higher risk of deficiency year-round.
Additional risk factors include advanced age (reduced skin synthesis capacity), limited mobility, cultural or religious practices involving covering skin, malabsorption disorders, chronic kidney disease, and certain medications. Patients on Saxenda with multiple risk factors warrant closer attention to vitamin D status.
Monitoring and Managing Vitamin D Levels on Saxenda
Routine monitoring of vitamin D levels is not universally required for all patients starting Saxenda. However, healthcare professionals should consider baseline assessment of serum 25-hydroxyvitamin D in patients with multiple risk factors for deficiency, particularly those with obesity, limited sun exposure, darker skin, or relevant comorbidities. NICE guidance does not mandate routine vitamin D testing in the general population but supports targeted testing in at-risk groups.
For patients found to have vitamin D deficiency (serum 25(OH)D <25 nmol/L), treatment typically involves loading doses of colecalciferol. According to NICE Clinical Knowledge Summaries, various regimens exist, but commonly include a total dose of approximately 300,000 IU given as weekly or daily doses over 6-12 weeks. For example, 20,000 IU weekly for 7 weeks (total 140,000 IU) or 50,000 IU weekly for 6 weeks (total 300,000 IU). Corrected calcium should be checked before starting high-dose therapy and approximately one month after completion. For insufficiency (25–50 nmol/L), maintenance supplementation of 800–2,000 IU daily is often appropriate. Vitamin D levels should be rechecked approximately 3 months after treatment.
Dietary optimisation should be encouraged alongside Saxenda treatment. Patients should be counselled to include vitamin D-rich foods such as oily fish (salmon, mackerel, sardines), egg yolks, and fortified products (some breakfast cereals, spreads, and plant-based milks). However, dietary sources alone are often insufficient to maintain adequate levels, particularly in the UK climate.
Supplementation advice aligns with NHS recommendations: all adults should consider taking a daily supplement containing 10 micrograms (400 IU) of vitamin D during autumn and winter. Those at higher risk of deficiency should take this dose year-round. The safe upper limit for long-term supplementation without medical supervision is 100 micrograms (4,000 IU) daily. There are no known clinically relevant interactions between Saxenda and vitamin D supplements.
Follow-up monitoring may be appropriate 3–6 months after initiating treatment in deficient patients to ensure adequate repletion. Patients experiencing persistent gastrointestinal symptoms or those losing significant weight should be reviewed to ensure nutritional adequacy across all micronutrients, not just vitamin D.
When to Seek Medical Advice
Patients taking Saxenda should contact their GP or healthcare provider if they experience symptoms potentially related to vitamin D deficiency. These include persistent bone or muscle pain, muscle weakness, frequent fractures, fatigue, or mood changes. Whilst these symptoms are non-specific and can have multiple causes, they warrant medical assessment, particularly in patients with known risk factors for deficiency.
Urgent medical attention is required for certain symptoms while taking Saxenda:
-
Severe, persistent upper abdominal pain, possibly radiating to the back, with or without vomiting (potential signs of pancreatitis): stop Saxenda immediately and seek urgent medical help or call 999
-
Symptoms of gallbladder disease (pain in upper right abdomen, fever, yellowing of skin/eyes): seek urgent medical review
-
Signs of severe dehydration (extreme thirst, dizziness, reduced urination): seek urgent medical advice
-
Signs of allergic reaction (rash, swelling, breathing difficulties): stop Saxenda and seek emergency help
Severe gastrointestinal symptoms that persist beyond the initial dose-escalation period or that significantly impair nutritional intake require medical review. If nausea, vomiting, or diarrhoea prevent adequate food and fluid intake, or if unintentional weight loss exceeds expected therapeutic weight loss, patients should seek advice promptly. Healthcare professionals may need to adjust the Saxenda dose, provide antiemetic medication, or refer to a dietitian for nutritional support.
Patients should also seek guidance if they have pre-existing conditions that affect vitamin D metabolism, such as chronic kidney disease (particularly stages 4-5), liver disease, malabsorption disorders (coeliac disease, Crohn's disease), or if they are taking medications known to interact with vitamin D metabolism. These individuals may require specialist input to optimise vitamin D management alongside Saxenda treatment.
Before starting supplementation, particularly at doses above standard recommendations, patients should consult their healthcare provider. Whilst vitamin D toxicity is rare, excessive supplementation can lead to hypercalcaemia. Patients with certain medical conditions, including sarcoidosis, hyperparathyroidism, or kidney stones, require specialist advice before taking vitamin D supplements.
Finally, patients should attend scheduled follow-up appointments for weight management monitoring. These consultations provide opportunities to discuss nutritional concerns, review overall health status, and ensure that weight loss is occurring safely and sustainably. Healthcare professionals can assess whether additional investigations, including vitamin D testing, are warranted based on individual circumstances and risk factors.
Patients are encouraged to report any suspected side effects from Saxenda via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Frequently Asked Questions
Does Saxenda cause vitamin D deficiency?
No, there is no established evidence that Saxenda directly causes vitamin D deficiency. However, factors associated with obesity and gastrointestinal side effects may contribute to low vitamin D levels in some patients.
Should I take vitamin D supplements whilst on Saxenda?
The NHS recommends all adults consider taking 10 micrograms (400 IU) of vitamin D daily during autumn and winter. Those at higher risk of deficiency, including people with obesity or darker skin, should take this dose year-round and discuss their individual needs with a healthcare professional.
Do I need a blood test to check my vitamin D levels before starting Saxenda?
Routine vitamin D testing is not required for all patients starting Saxenda. However, healthcare professionals may recommend baseline testing for those with multiple risk factors, including obesity, limited sun exposure, darker skin, or relevant comorbidities.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript