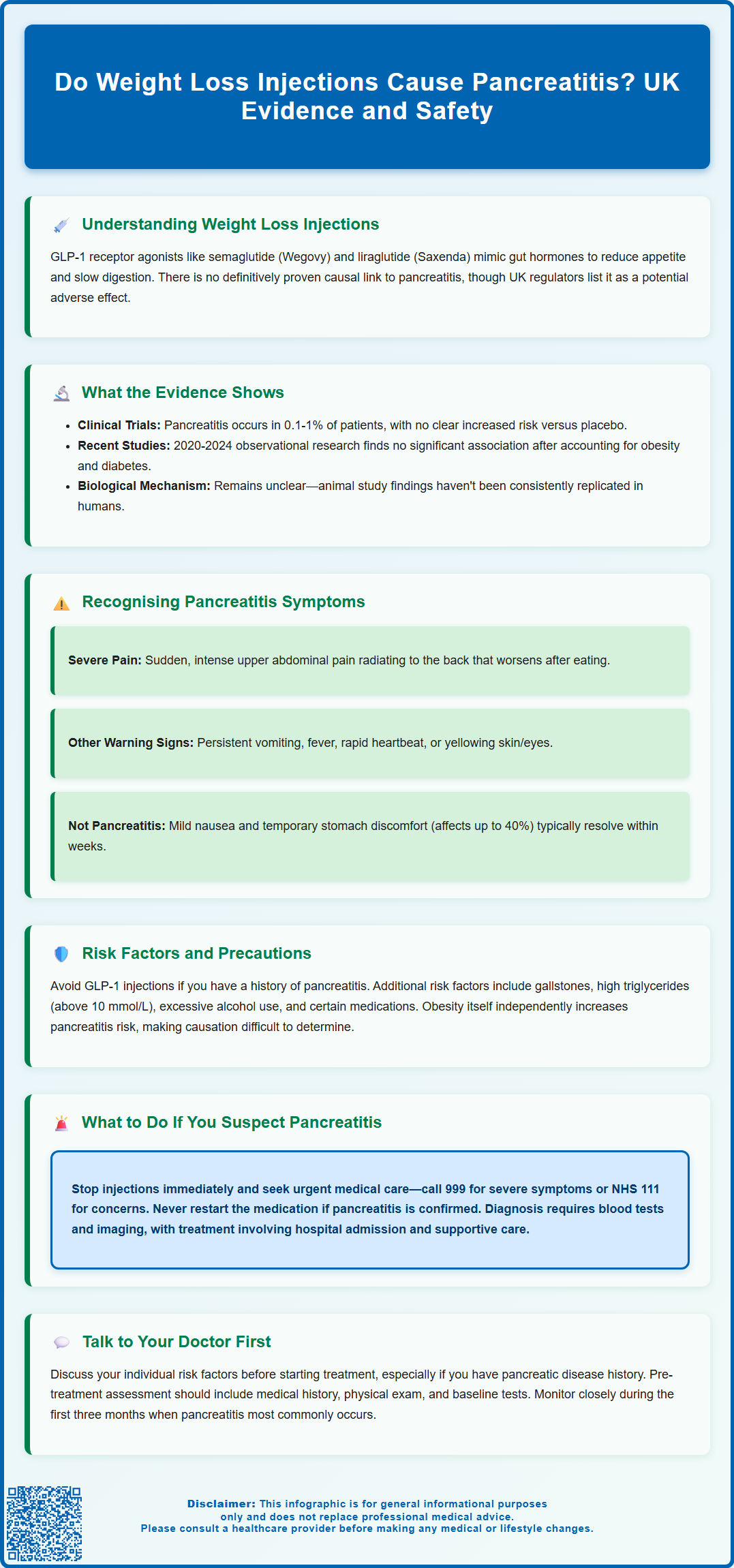
Weight loss injections, particularly GLP-1 receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), have transformed obesity management in the UK. Whilst these medications offer significant benefits when combined with lifestyle changes, questions persist about potential adverse effects, including pancreatitis. Current evidence does not establish a definitive causal link between GLP-1 receptor agonists and pancreatitis, though UK regulatory guidance lists it as a possible risk. Obesity itself increases pancreatitis risk, making causality difficult to determine. This article examines the evidence, symptoms to recognise, risk factors, and appropriate precautions for patients considering or using weight loss injections.
Summary: Current evidence does not establish a definitive causal relationship between weight loss injections (GLP-1 receptor agonists) and pancreatitis, though UK regulatory guidance lists pancreatitis as a potential adverse effect requiring monitoring.
- GLP-1 receptor agonists such as semaglutide and liraglutide are licensed in the UK for obesity management and work by mimicking gut hormones that regulate appetite and blood glucose.
- Large-scale trials report pancreatitis as uncommon (0.1–1% of patients) with no clear increased risk versus placebo, though obesity itself is an independent pancreatitis risk factor.
- UK guidance advises stopping treatment immediately if pancreatitis is suspected and not restarting if confirmed; patients should be informed about characteristic symptoms including severe upper abdominal pain.
- Pre-treatment assessment should identify risk factors including previous pancreatitis, gallstone disease, hypertriglyceridaemia, and excessive alcohol consumption to guide appropriate patient selection.
Table of Contents
Understanding Weight Loss Injections and Pancreatitis Risk
Weight loss injections, primarily glucagon-like peptide-1 (GLP-1) receptor agonists, have become increasingly prescribed for obesity management in the UK. Medications such as semaglutide (Wegovy) and liraglutide (Saxenda) are licensed for weight management, while other GLP-1 receptor agonists like dulaglutide (Trulicity) are licensed only for type 2 diabetes in the UK. These agents work by mimicking natural gut hormones that regulate appetite and blood glucose levels, slowing gastric emptying, enhancing satiety, and promoting weight reduction when combined with lifestyle modifications.
Pancreatitis—inflammation of the pancreas—is a serious condition that can present acutely or develop into a chronic disorder. The pancreas produces digestive enzymes and hormones including insulin, making its health critical for metabolic function. Acute pancreatitis typically causes severe abdominal pain, nausea, and vomiting, whilst chronic pancreatitis may lead to persistent digestive problems and diabetes.
The question of whether weight loss injections cause pancreatitis has been subject to ongoing pharmacovigilance and clinical investigation. There is no definitively established causal relationship, but UK and European regulatory bodies have noted pancreatitis as a potential adverse effect in the Summaries of Product Characteristics (SmPCs) for GLP-1 receptor agonists. The SmPCs advise informing patients about symptoms of pancreatitis, stopping treatment if pancreatitis is suspected, and not restarting if pancreatitis is confirmed.
It is important to contextualise this risk: obesity itself is an independent risk factor for pancreatitis, as are conditions commonly associated with excess weight such as gallstones, hypertriglyceridaemia, and type 2 diabetes. Distinguishing whether pancreatitis cases result from the medication, underlying metabolic conditions, or other factors remains challenging. Patients considering these treatments should discuss their individual risk profile with their prescribing clinician, particularly if they have a history of pancreatic disease.
Evidence Linking GLP-1 Receptor Agonists to Pancreatitis
The evidence base examining pancreatitis risk with GLP-1 receptor agonists presents a complex picture. Large-scale randomised controlled trials such as the STEP programme (semaglutide) and SCALE trials (liraglutide) reported pancreatitis as an uncommon adverse event (occurring in 0.1-1% of patients), with no clear signal for increased risk compared to placebo. However, these trials were not specifically powered to detect rare pancreatic events, limiting definitive conclusions.
Recent observational studies and meta-analyses (2020-2024) have generally not confirmed an increased risk of pancreatitis with GLP-1 receptor agonists. While earlier studies suggested a possible modest increase in risk, more recent comprehensive analyses have found no significant association after adjusting for confounding factors such as obesity, diabetes duration, and concurrent medications.
The mechanism by which GLP-1 receptor agonists might theoretically contribute to pancreatitis is not fully elucidated. Animal studies suggested potential pancreatic ductal proliferation and inflammation, but these findings have not been consistently replicated in human tissue studies. GLP-1 receptors are present on pancreatic tissue, and the drugs' effects on pancreatic enzyme secretion and ductal pressure remain areas of active research.
Regulatory guidance from UK and European authorities advises caution in patients with a history of pancreatitis. The SmPCs recommend that patients should be informed about characteristic symptoms of acute pancreatitis, treatment should be discontinued if pancreatitis is suspected, and should not be restarted if pancreatitis is confirmed. The European Medicines Agency conducted a comprehensive review in 2013 and concluded that available data did not confirm increased pancreatic cancer or pancreatitis risk, but recommended continued monitoring. NICE guidance for obesity management acknowledges this uncertainty whilst supporting the use of these agents when clinically appropriate, emphasising the importance of patient selection and monitoring.
Recognising Symptoms of Pancreatitis During Treatment
Early recognition of pancreatitis symptoms is crucial for patients receiving weight loss injections. Acute pancreatitis typically presents with sudden-onset, severe upper abdominal pain that may radiate to the back. This pain is often described as constant and boring in nature, worsening after eating, and may be partially relieved by leaning forward. The intensity usually distinguishes it from common gastrointestinal side effects of GLP-1 medications such as nausea or mild abdominal discomfort.
Associated symptoms that should prompt immediate medical attention include:
-
Persistent nausea and vomiting that prevents oral intake
-
Abdominal tenderness and distension
-
Fever and rapid heart rate
-
Jaundice (yellowing of skin or eyes) in cases involving biliary obstruction
If severe, persistent upper abdominal pain occurs, patients should stop their GLP-1 injection immediately and seek urgent medical assessment.
It is important to differentiate pancreatitis from the expected gastrointestinal side effects of GLP-1 receptor agonists, which are common, particularly during dose titration. Mild-to-moderate nausea, occasional vomiting, and transient abdominal discomfort affect up to 40% of patients but typically improve within weeks. These symptoms are generally manageable and do not indicate pancreatic inflammation.
Timing considerations: Pancreatitis can theoretically occur at any point during treatment, though case reports suggest onset within the first few months is more common. Patients should not dismiss persistent or worsening abdominal symptoms as merely drug-related side effects. Any severe abdominal pain lasting more than a few hours warrants urgent medical assessment.
Healthcare professionals should provide clear safety netting advice when initiating weight loss injections, ensuring patients understand which symptoms require immediate evaluation. Written information reinforcing these warning signs supports informed decision-making and appropriate help-seeking behaviour.
Risk Factors and Precautions for Patients
Patient selection is fundamental to minimising potential pancreatitis risk with weight loss injections. UK SmPCs advise that GLP-1 receptor agonists should be used with caution in patients with a history of pancreatitis. Patients should be educated about symptoms, treatment should be discontinued if pancreatitis is suspected, and should not be restarted if pancreatitis is confirmed.
Additional risk factors that warrant cautious evaluation include:
-
Gallstone disease: Cholelithiasis is a leading cause of pancreatitis, and rapid weight loss can paradoxically increase gallstone formation risk
-
Hypertriglyceridaemia: Triglyceride levels above 10 mmol/L significantly elevate pancreatitis risk; lipid profiles should be optimised before treatment
-
Excessive alcohol consumption: Alcohol is a major pancreatitis trigger and should be addressed as part of comprehensive lifestyle modification
-
Concurrent medications: Certain drugs (e.g., azathioprine, sodium valproate, thiazide diuretics) are associated with drug-induced pancreatitis
Pre-treatment assessment should include a thorough medical history and physical examination. Baseline investigations should be guided by clinical indication and comorbidities. For patients with diabetes, dyslipidaemia or other relevant conditions, appropriate tests may include renal function, HbA1c, and lipid profiles as clinically indicated and per local protocols. Whilst routine pancreatic enzyme testing is not indicated in asymptomatic patients, clinicians should maintain a low threshold for investigation if symptoms develop.
Ongoing monitoring involves regular clinical review, particularly during the first three months of treatment. Patients should be educated about symptom recognition and encouraged to report any concerning abdominal symptoms promptly. Dose escalation should follow licensed schedules to minimise gastrointestinal adverse effects. For patients with multiple risk factors, shared decision-making should weigh potential benefits against theoretical risks, considering alternative pharmacological or surgical weight loss options where appropriate.
What to Do If You Suspect Pancreatitis
Immediate action is essential if pancreatitis is suspected during weight loss injection therapy. Patients experiencing severe, persistent abdominal pain should discontinue the medication immediately and seek urgent medical assessment. For severe symptoms or signs of systemic illness (such as severe dehydration or shock), call 999 or go directly to an emergency department. For less severe but concerning symptoms, contact NHS 111 for advice.
Clinical evaluation for suspected pancreatitis involves several key steps. Healthcare professionals will conduct a thorough history and examination, assessing pain characteristics, associated symptoms, and risk factors. Diagnostic investigations typically include:
-
Serum amylase and lipase: Pancreatic enzyme levels elevated to three times the upper limit of normal support the diagnosis, with lipase being more sensitive and specific. Note that normal enzyme levels do not fully exclude pancreatitis
-
Liver function tests: To identify biliary causes and assess hepatic involvement
-
Full blood count and inflammatory markers: Elevated white cell count and C-reactive protein indicate inflammation
-
Imaging studies: Abdominal ultrasound or CT scanning to visualise pancreatic inflammation, identify complications, and exclude alternative diagnoses
Management of confirmed pancreatitis requires hospital admission in most cases. Treatment is primarily supportive, including intravenous fluid resuscitation, analgesia, antiemetics, and nutritional support. The GLP-1 receptor agonist should not be restarted, and alternative weight management strategies should be considered once recovery is complete.
Follow-up care is important after a pancreatitis episode. Patients require investigation to identify and address underlying causes such as gallstones or hypertriglyceridaemia. Lifestyle modifications including alcohol cessation and dietary fat reduction are recommended. For ongoing obesity management, patients should discuss alternative options with their GP or specialist, which may include other pharmacological agents (such as orlistat), behavioural interventions, or referral for bariatric surgery assessment in appropriate cases.
Suspected adverse reactions to GLP-1 receptor agonists should be reported through the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk), which contributes to ongoing pharmacovigilance and patient safety.
Frequently Asked Questions
Should I stop my weight loss injection if I have abdominal pain?
If you experience severe, persistent upper abdominal pain whilst taking a GLP-1 receptor agonist, stop the medication immediately and seek urgent medical assessment. Mild nausea or discomfort is common and usually improves, but severe pain warrants immediate evaluation to exclude pancreatitis.
Can I use weight loss injections if I've had pancreatitis before?
UK guidance advises caution in patients with a history of pancreatitis. GLP-1 receptor agonists should not be restarted if pancreatitis is confirmed during treatment, and alternative weight management options should be discussed with your GP or specialist.
How common is pancreatitis with medications like Wegovy or Saxenda?
Clinical trials report pancreatitis as uncommon, occurring in 0.1–1% of patients taking GLP-1 receptor agonists. Recent comprehensive studies have not confirmed an increased risk compared to placebo after adjusting for factors such as obesity and diabetes, which themselves increase pancreatitis risk.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript