Weight loss injections such as semaglutide (Wegovy), liraglutide (Saxenda), and tirzepatide (Mounjaro) are increasingly prescribed in the UK for weight management. As their use grows, many patients wonder whether these GLP-1 receptor agonists might affect their ability to conceive. Whilst obesity itself is a recognised risk factor for fertility problems, the relationship between weight loss medications and reproductive health requires careful consideration. This article examines current evidence, regulatory guidance from the MHRA and NICE, and clinical recommendations to help patients and healthcare professionals understand how these treatments may influence fertility, pregnancy planning, and reproductive outcomes.
Summary: Weight loss injections are not identified as causing infertility in UK product information, though they should be stopped before attempting conception.
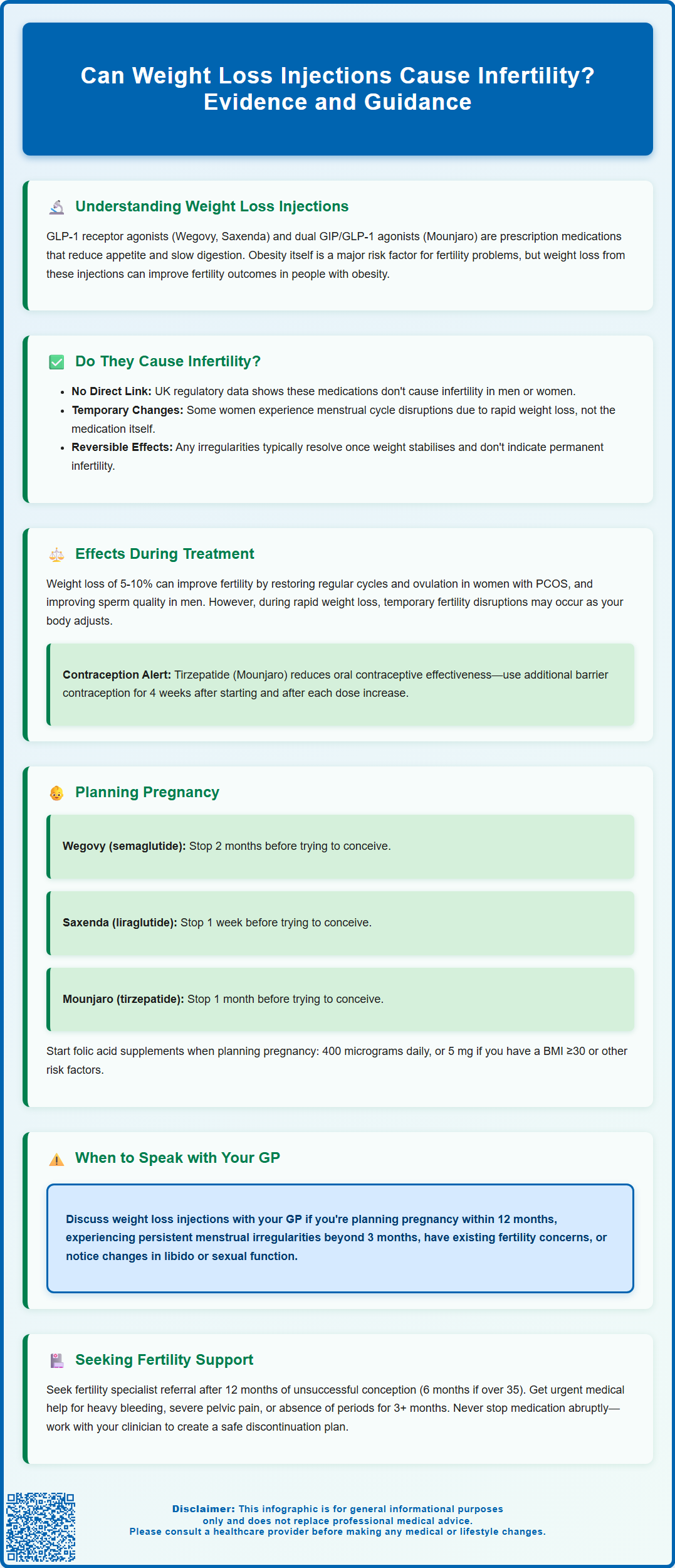
- GLP-1 receptor agonists (semaglutide, liraglutide, tirzepatide) do not list infertility as a recognised adverse effect in MHRA-approved product information.
- Temporary menstrual irregularities may occur during treatment due to rapid weight loss and metabolic changes, not direct reproductive toxicity.
- Weight loss achieved through these medications often improves fertility outcomes in individuals with obesity-related reproductive dysfunction such as PCOS.
- Medications must be discontinued before conception attempts: semaglutide 2 months before, liraglutide 1 week before, tirzepatide 1 month before.
- Tirzepatide may reduce oral contraceptive efficacy, requiring additional barrier contraception for 4 weeks after initiation and dose escalations.
- Patients planning pregnancy or experiencing persistent menstrual irregularities should discuss fertility implications with their GP for personalised guidance.
Table of Contents
Understanding Weight Loss Injections and Reproductive Health
Weight loss injections, particularly GLP-1 receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), as well as tirzepatide (Mounjaro, a dual GIP/GLP-1 receptor agonist), have become increasingly prescribed for weight management in the UK. These prescription-only medications work by mimicking the action of gut hormones that regulate appetite and blood glucose levels. By slowing gastric emptying and enhancing feelings of satiety, these injections help patients achieve clinically significant weight loss when combined with lifestyle modifications.
The relationship between body weight and reproductive health is well established in medical literature. Obesity is recognised as a significant risk factor for fertility problems in both men and women, affecting hormone production, ovulation, sperm quality, and overall reproductive function. NICE guidelines (NG156) acknowledge that weight reduction can improve fertility outcomes in individuals with obesity, making weight loss interventions a potential tool in addressing obesity-related reproductive challenges.
However, as these medications have gained popularity, questions have emerged regarding their direct effects on fertility and reproductive health. Patients considering or currently using weight loss injections often express concerns about whether these treatments might compromise their ability to conceive. Understanding the distinction between the medication's direct effects and the beneficial impact of weight loss itself is crucial for informed decision-making.
Can Weight Loss Injections Cause Infertility?
Weight loss injections are not identified as causing infertility in men or women in UK product information. The MHRA-approved Summaries of Product Characteristics (SmPCs) for semaglutide, liraglutide and tirzepatide do not list infertility as a recognised adverse effect, though clinical trials were not specifically designed to detect fertility issues. Animal studies have shown some fertility effects, but these are largely attributed to reduced food intake and weight loss rather than direct reproductive toxicity.
The mechanism of action of these medications centres on appetite regulation and glucose metabolism. While GLP-1 receptors are present throughout the body, including in the pancreas, brain, and gastrointestinal tract, there is limited evidence suggesting they directly disrupt the hormonal systems governing fertility.
What can occur during treatment is a temporary disruption to menstrual cycles in some women, particularly during the initial months of therapy. This is typically attributed to rapid weight loss and metabolic changes rather than a direct drug effect. Rapid weight reduction from any cause—whether through medication, surgery, or intensive lifestyle modification—can temporarily affect ovulation and menstrual regularity. These changes are generally reversible and do not indicate permanent fertility impairment.
It is important to distinguish between temporary menstrual irregularities and true infertility. While some women may experience delayed or missed periods during active weight loss, this does not equate to permanent reproductive damage. If you miss a period while taking weight loss injections, it's advisable to take a pregnancy test and consult your healthcare provider. For women with obesity-related fertility problems such as polycystic ovary syndrome (PCOS), the weight loss achieved through these medications may actually improve fertility outcomes by restoring more regular ovulation and hormonal balance.
Effects on Fertility During Treatment
The effects of weight loss injections on fertility during active treatment are complex and vary considerably between individuals. For many patients, particularly those with obesity-related reproductive dysfunction, weight loss can lead to improved fertility parameters. Women with PCOS, for instance, often experience restoration of regular menstrual cycles and ovulation as they lose weight, regardless of the method used to achieve that weight loss.
Research indicates that even modest weight reduction of 5-10% of body weight can significantly improve reproductive hormone profiles, including reductions in insulin resistance, androgens, and improvements in sex hormone-binding globulin levels. These metabolic improvements can enhance fertility potential. In men, weight loss has been associated with improved sperm parameters, including sperm count, motility, and morphology, alongside beneficial changes in testosterone levels.
However, during the active phase of rapid weight loss, some individuals may experience temporary fertility fluctuations. Women may notice irregular periods, changes in cycle length, or occasionally anovulatory cycles. These effects are generally attributed to the body's metabolic adaptation to significant weight change rather than direct medication toxicity. The endocrine system requires time to recalibrate following substantial weight loss, and temporary disruptions are not uncommon.
Regarding contraception during treatment, the advice varies by medication. For tirzepatide (Mounjaro), the SmPC advises that it can reduce the exposure to oral contraceptives, so additional barrier contraception is recommended for 4 weeks after initiation and after each dose escalation. For injectable semaglutide and liraglutide, there is no clinically relevant effect on oral contraceptive efficacy. However, if you experience vomiting or severe diarrhoea while taking oral contraceptives, follow the NHS 'missed pill' guidance. Long-acting reversible contraceptives (LARC) such as implants, injections, IUDs or IUS are not affected by these medications and may be more reliable options during treatment.
Importantly, women should be aware that improved fertility due to weight loss may increase the chance of unplanned conception if not using effective contraception.
Pregnancy Planning and Weight Loss Injections
Current UK product guidance provides specific recommendations for discontinuing weight loss injections before attempting to conceive. The timing varies by medication:
-
Semaglutide (Wegovy): Stop at least 2 months before attempting conception
-
Liraglutide (Saxenda): Stop at least 1 week before attempting conception
-
Tirzepatide (Mounjaro): Stop at least 1 month before attempting conception
These precautionary approaches reflect limited data on the safety of these medications during pregnancy rather than evidence of harm. None of these medications are recommended during pregnancy or breastfeeding.
For individuals planning pregnancy, the optimal approach involves:
-
Achieving target weight loss before conception attempts, allowing time to stabilise at a healthier weight
-
Discontinuing the injection according to the product-specific timeframe before trying to conceive
-
Transitioning to lifestyle-based weight maintenance strategies to preserve weight loss benefits
-
Commencing folic acid supplementation (400 micrograms daily for most women; some with higher risk factors such as BMI ≥30 or diabetes may be advised to take 5 mg daily by their GP)
-
Attending pre-conception counselling with a GP or fertility specialist to optimise overall health
The rationale for stopping treatment before conception is primarily precautionary. If you discover you are pregnant while taking weight loss injections, stop the medication immediately and contact your GP or maternity services promptly for advice.
It is important to recognise that the weight loss achieved during treatment can be maintained and continues to benefit fertility even after stopping the medication. Many patients find that the metabolic improvements, dietary habit changes, and weight reduction persist, supporting both natural conception and assisted reproduction outcomes. For those undergoing fertility treatments such as IVF, achieving a healthier BMI through weight loss injections prior to treatment cycles may improve success rates, provided the medication is discontinued appropriately beforehand.
When to Speak with Your GP About Fertility Concerns
Patients using or considering weight loss injections should discuss fertility implications with their GP, particularly in the following circumstances:
-
Planning to conceive within the next 12 months – early discussion allows appropriate timing of treatment cessation and optimisation of pre-conception health
-
Experiencing persistent menstrual irregularities beyond the first three months of treatment – whilst some cycle changes are expected, prolonged amenorrhoea warrants investigation
-
Existing fertility concerns or previous difficulty conceiving – a comprehensive fertility assessment may be needed alongside weight management
-
Considering fertility preservation – individuals planning delayed parenthood may wish to discuss options such as egg or sperm freezing
-
Unexplained changes in libido or sexual function – though not common, any concerning symptoms should be evaluated
Your GP can provide personalised advice based on your individual circumstances, medical history, and reproductive goals. In line with NICE guidance (NG156), initial fertility investigations typically include semen analysis for men and mid-luteal progesterone to confirm ovulation for women with regular cycles. Additional hormone tests (FSH, LH, oestradiol, testosterone, prolactin, thyroid function) may be recommended selectively based on symptoms and menstrual patterns rather than as routine baseline tests.
For couples who have been trying to conceive for 12 months without success (or 6 months if the woman is over 35), referral to fertility services is appropriate regardless of weight loss injection use. Consider seeking advice earlier if you're 36 years or older, and expect expedited assessment if you're over 40. The NHS provides fertility investigation and treatment services, with eligibility criteria varying by local integrated care board (ICB).
Seek urgent medical advice if you experience: heavy or unusual vaginal bleeding, severe one-sided pelvic pain (especially with bleeding or shoulder-tip pain which could indicate ectopic pregnancy), absence of periods for 3 months or more, unusual breast discharge, or any severe symptoms while using weight loss injections.
Do not stop prescribed weight loss medication without medical guidance. Abrupt discontinuation should be discussed with your prescribing clinician, who can provide a structured plan for stopping treatment safely whilst maintaining weight loss through lifestyle measures. If you experience side effects from your medication, report them through the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk).
Frequently Asked Questions
Do weight loss injections like Wegovy or Saxenda cause permanent infertility?
No, weight loss injections are not identified as causing permanent infertility in UK product information. Temporary menstrual irregularities may occur during treatment due to rapid weight loss, but these are generally reversible and do not indicate permanent reproductive damage.
How long should I stop weight loss injections before trying to conceive?
The recommended timeframe varies by medication: stop semaglutide (Wegovy) at least 2 months before conception, liraglutide (Saxenda) at least 1 week before, and tirzepatide (Mounjaro) at least 1 month before attempting to conceive.
Can weight loss injections actually improve fertility?
Yes, for individuals with obesity-related fertility problems such as PCOS, the weight loss achieved through these medications may improve fertility outcomes by restoring regular ovulation, improving hormonal balance, and enhancing metabolic health.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript












