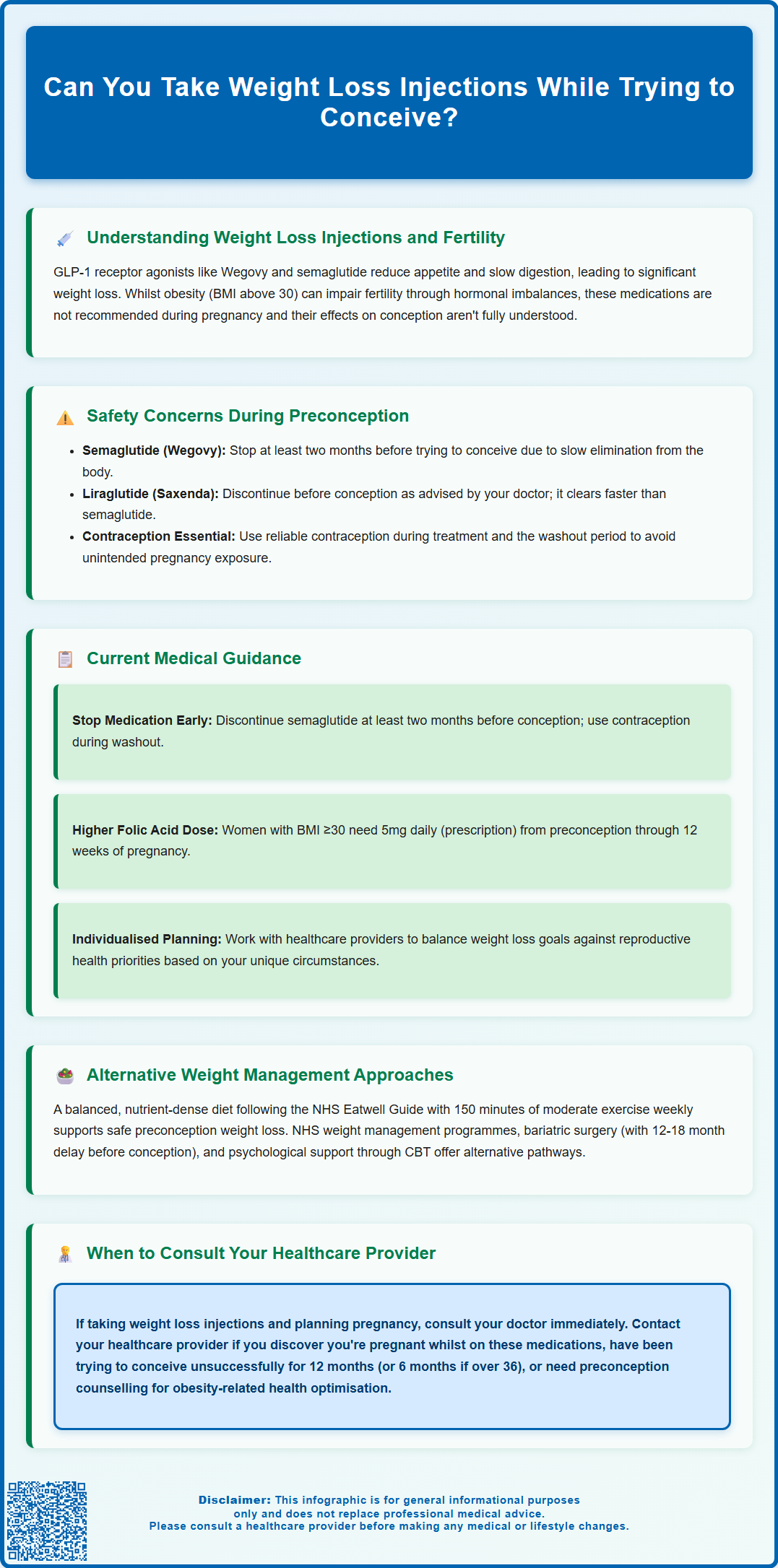
Can you take weight loss injections while trying to conceive? This is an important question for women using GLP-1 receptor agonists such as semaglutide (Wegovy) or liraglutide (Saxenda) who are planning pregnancy. Current UK medical guidance advises against using these medications during the preconception period due to potential risks to early pregnancy. Semaglutide should be discontinued at least two months before attempting conception, whilst liraglutide should be stopped before trying to conceive. Whilst achieving a healthier weight can improve fertility outcomes, the timing and method of weight loss require careful consideration. This article explores the safety concerns, current medical guidance, and alternative approaches for women planning pregnancy.
Summary: Weight loss injections such as semaglutide and liraglutide should not be taken whilst trying to conceive and must be discontinued before attempting pregnancy.
- Semaglutide (Wegovy) is contraindicated in pregnancy and must be stopped at least two months before attempting conception due to its long half-life.
- Liraglutide (Saxenda) is not recommended during pregnancy and should be discontinued before trying to conceive, following clinician advice.
- GLP-1 receptor agonists work by mimicking hormones that regulate appetite and blood sugar, facilitating weight reduction when combined with lifestyle changes.
- Reliable contraception is essential whilst taking these medications and during the washout period to prevent unintended foetal exposure.
- Women with obesity planning pregnancy should receive preconception counselling and higher-dose folic acid supplementation (5mg daily on prescription).
- Alternative weight management approaches including dietary modifications, physical activity, and NHS-supported programmes can be safely continued during preconception.
Table of Contents
Understanding Weight Loss Injections and Fertility
Weight loss injections, particularly GLP-1 receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), have become increasingly popular for managing obesity in the UK. These medications work by mimicking the glucagon-like peptide-1 hormone, which regulates appetite and blood sugar levels. By slowing gastric emptying and enhancing feelings of satiety, they facilitate significant weight reduction when combined with lifestyle modifications.
In the UK, Wegovy is licensed for adults with a BMI of 30 kg/m² or greater (obesity), or from 27 kg/m² to less than 30 kg/m² (overweight) in the presence of at least one weight-related comorbidity. Saxenda has similar indications. Importantly, semaglutide is contraindicated in pregnancy, while liraglutide is not recommended during pregnancy or breastfeeding.
The relationship between body weight and fertility is well-established in medical literature. Obesity can adversely affect reproductive health through various mechanisms, including hormonal imbalances, insulin resistance, and disruption of ovulatory cycles. Women with a body mass index (BMI) above 30 may experience reduced fertility and increased pregnancy complications. Consequently, achieving a healthier weight before conception is often recommended by healthcare professionals.
However, the timing and method of weight loss become crucial considerations when planning pregnancy. Whilst weight reduction can improve fertility outcomes, the use of pharmacological interventions during the preconception period requires careful evaluation. The effects of GLP-1 receptor agonists on reproductive function and early pregnancy are not fully characterised, making this a complex clinical decision.
Key considerations include:
-
The mechanism by which these medications affect metabolic and hormonal pathways
-
Potential direct or indirect effects on conception and early embryonic development
-
The duration these medications remain in the body after discontinuation
-
Individual patient factors, including BMI, underlying health conditions, and fertility status
It's important to note that improved weight and metabolic control may restore ovulation in some women, particularly those with obesity or polycystic ovary syndrome (PCOS). Therefore, effective contraception is essential while using GLP-1 receptor agonists, and they should be discontinued appropriately before attempting conception.
Safety Concerns During Preconception
The primary safety concern regarding weight loss injections during preconception relates to potential foetal exposure during early pregnancy. Current evidence from animal studies has raised questions about possible risks, though human data remains limited. The Medicines and Healthcare products Regulatory Agency (MHRA) and manufacturers advise discontinuing GLP-1 receptor agonists before attempting conception due to these uncertainties.
Semaglutide (Wegovy) is contraindicated in pregnancy and has a particularly long half-life of approximately one week, meaning it takes several weeks to be eliminated from the body completely. The manufacturer recommends discontinuing Wegovy at least two months before planned conception to ensure adequate washout. This extended timeframe accounts for the medication's pharmacokinetic properties and allows the body to return to its baseline metabolic state.
Liraglutide (Saxenda) is not recommended during pregnancy and has a shorter half-life of approximately 13 hours, clearing from the system more rapidly. The Saxenda SmPC (Summary of Product Characteristics) does not specify a two-month washout period but advises stopping before trying to conceive. Women should follow their clinician's advice regarding the appropriate timing of discontinuation.
Reliable contraception should be used while taking these medications and during the washout period to prevent unintended pregnancy exposure.
Additional concerns include the potential for rapid weight loss to affect nutritional status during the critical periconceptional period. Adequate nutrition, particularly folic acid and other essential nutrients, is vital for preventing neural tube defects and supporting early foetal development. Rapid weight reduction may compromise nutrient stores or eating patterns, potentially affecting preconception health.
There is also consideration of weight regain after discontinuation. Many individuals experience increased appetite and weight regain after stopping these medications, which could impact metabolic health during the conception period without ongoing lifestyle support. Furthermore, the hormonal changes associated with significant weight fluctuations may temporarily affect menstrual regularity and ovulation, though this typically normalises after medication cessation.
Current Medical Guidance for Women Trying to Conceive
The National Institute for Health and Care Excellence (NICE) provides comprehensive guidance on weight management and fertility. NICE recommends that women with obesity who are planning pregnancy should be offered support to achieve weight loss before conception, as this improves both fertility and pregnancy outcomes. However, the guidance emphasises that any pharmacological interventions should be carefully timed and discontinued appropriately.
Current manufacturer recommendations, endorsed by UK regulatory authorities, advise women to:
-
Discontinue semaglutide (Wegovy) at least two months before attempting to conceive
-
Stop liraglutide (Saxenda) before trying to conceive (following SmPC and clinician advice)
-
Use reliable contraception whilst taking these medications and during the washout period
-
Consult with their GP or fertility specialist before stopping medication to ensure appropriate planning
-
Consider the timing of weight loss efforts in relation to their fertility journey
The Royal College of Obstetricians and Gynaecologists (RCOG) emphasises the importance of preconception counselling for women with obesity. This should include discussion of optimal timing for weight loss, the role of lifestyle modifications, and the potential need to discontinue certain medications. Healthcare providers should adopt an individualised approach, considering each woman's specific circumstances, including her BMI, fertility status, age, and any underlying medical conditions.
For women already taking weight loss injections who discover they are pregnant, guidance recommends immediate discontinuation and prompt contact with healthcare providers. Due to limited human data, the risk to the developing foetus cannot be ruled out. Women should discuss any exposure with their clinician and consider contacting the UK Teratology Information Service (UKTIS) for individual risk assessment.
NHS guidance also stresses the importance of achieving optimal health before conception, including:
-
Maintaining a balanced diet rich in essential nutrients
-
Taking 400 micrograms of folic acid daily (higher doses of 5mg daily on prescription for women with BMI ≥30, to be taken from preconception until 12 weeks' gestation)
-
Addressing any underlying health conditions such as diabetes or hypertension
-
Avoiding alcohol and smoking
Women should work collaboratively with their healthcare team to develop a personalised preconception plan that balances weight management goals with reproductive health priorities.
Alternative Weight Management Approaches
For women trying to conceive who need to manage their weight, several evidence-based alternatives to pharmacological interventions are available. These approaches can be safely continued throughout the preconception period and often into pregnancy with appropriate modifications.
Dietary modifications form the cornerstone of safe preconception weight management. A balanced, nutrient-dense diet that creates a modest caloric deficit can facilitate gradual weight loss without compromising nutritional status. The NHS Eatwell Guide provides a framework for healthy eating, emphasising:
-
Plenty of fruits and vegetables (at least five portions daily)
-
Whole grain carbohydrates for sustained energy
-
Lean proteins including fish, poultry, beans, and pulses
-
Limited intake of foods high in saturated fat, salt, and sugar
-
Adequate hydration with water as the primary beverage
Referral to a registered dietitian can provide personalised nutritional guidance tailored to preconception needs, ensuring adequate intake of folate, iron, calcium, and other essential nutrients whilst supporting weight management goals.
Physical activity offers multiple benefits for women planning pregnancy. The UK Chief Medical Officers recommend at least 150 minutes of moderate-intensity aerobic activity weekly, which can be safely continued during preconception and adapted during pregnancy. Activities such as brisk walking, swimming, cycling, and pregnancy-safe exercise classes can support weight management whilst improving cardiovascular fitness and metabolic health.
Behavioural interventions addressing eating patterns, emotional eating, and lifestyle habits can produce sustainable results. NHS-supported programmes such as the NHS Weight Loss Plan and NHS Tier 2/3 weight management services (available via GP referral) offer structured support combining dietary advice, physical activity guidance, and behavioural strategies. The NHS Digital Weight Management Programme may also be available for eligible patients. These programmes can be particularly effective when combined with peer support or professional counselling.
For women with significant obesity (BMI ≥40 or ≥35 with comorbidities), bariatric surgery may be considered, though conception should typically be delayed for 12–18 months post-surgery to allow for weight stabilisation and nutritional optimisation. Effective contraception is essential during this period. Women who have undergone bariatric surgery require ongoing micronutrient supplementation and monitoring, and should receive specialist antenatal care when pregnant. This option requires careful discussion with specialist teams.
Psychological support should not be overlooked, as the emotional aspects of weight management and fertility can be challenging. Cognitive behavioural therapy (CBT) and other therapeutic approaches can address underlying factors contributing to weight gain and support sustainable lifestyle changes.
When to Consult Your Healthcare Provider
Navigating weight management whilst trying to conceive requires professional guidance to ensure both safety and effectiveness. Women should consult their GP or healthcare provider in several specific circumstances to receive personalised advice and appropriate support.
If you are currently taking weight loss injections and planning to conceive, contact your prescribing doctor promptly to discuss:
-
The appropriate timeline for discontinuation (at least two months before attempting conception for semaglutide; before trying to conceive for liraglutide)
-
Contraceptive measures during the washout period
-
Alternative weight management strategies to maintain progress
-
Monitoring plans to assess metabolic health before conception
Your healthcare provider can help coordinate care between different specialists, including fertility consultants, endocrinologists, and dietitians, ensuring a comprehensive approach to your preconception health.
Seek medical advice if you:
-
Have been trying to conceive for 12 months without success (or 6 months if aged 36 or over)
-
Experience irregular menstrual cycles or absent periods
-
Have underlying health conditions such as polycystic ovary syndrome (PCOS), diabetes, or thyroid disorders
-
Are concerned about rapid weight regain after stopping medication
-
Discover you are pregnant whilst taking weight loss injections
-
Experience any unusual symptoms after discontinuing medication
If you have taken weight loss injections during early pregnancy before knowing you were pregnant, contact your healthcare provider immediately. You may also contact the UK Teratology Information Service (UKTIS) for individual risk assessment regarding medication exposure during pregnancy.
Preconception counselling is particularly important for women with obesity, as this provides an opportunity to:
-
Assess overall health status and identify any conditions requiring management
-
Optimise control of existing medical conditions
-
Review all medications for safety during conception and pregnancy
-
Discuss realistic weight management goals and timelines
-
Ensure appropriate supplementation, including higher-dose folic acid (5mg daily on prescription for women with BMI ≥30, to be taken from preconception until 12 weeks' gestation)
-
Address any concerns about fertility or pregnancy risks
Your GP can provide referrals to specialist services, including fertility clinics, weight management programmes, or maternal medicine services as appropriate. Early engagement with healthcare services allows for comprehensive planning and support, improving both your chances of conception and the health of your future pregnancy. Remember that healthcare professionals are there to support your journey without judgement, providing evidence-based guidance tailored to your individual circumstances and goals.
If you experience any suspected side effects from weight loss medications, report them through the MHRA Yellow Card scheme, which helps monitor the safety of medicines in the UK.
Frequently Asked Questions
How long should I stop taking Wegovy before trying to conceive?
You should discontinue Wegovy (semaglutide) at least two months before attempting to conceive. This extended washout period accounts for the medication's long half-life and allows your body to return to its baseline metabolic state.
What should I do if I become pregnant whilst taking weight loss injections?
If you discover you are pregnant whilst taking weight loss injections, stop the medication immediately and contact your healthcare provider promptly. You may also contact the UK Teratology Information Service (UKTIS) for individual risk assessment regarding medication exposure during pregnancy.
What are safe alternatives to weight loss injections when trying to conceive?
Safe alternatives include dietary modifications following the NHS Eatwell Guide, regular physical activity (at least 150 minutes weekly), NHS-supported weight management programmes, and behavioural interventions. These approaches can be safely continued throughout the preconception period with appropriate professional guidance.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript