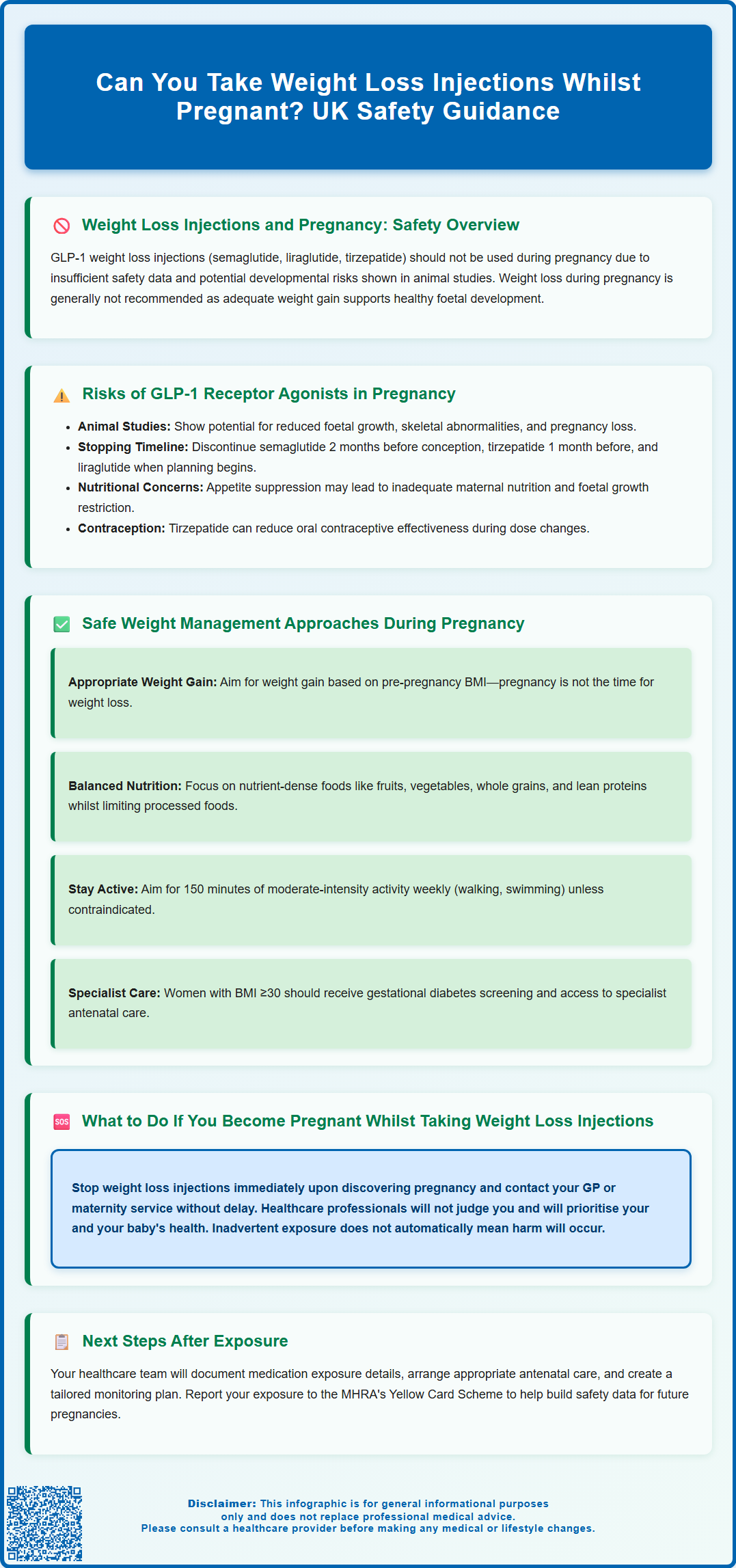
Weight loss injections such as semaglutide (Wegovy, Ozempic), liraglutide (Saxenda), and tirzepatide (Mounjaro) are not safe to use during pregnancy. The Medicines and Healthcare products Regulatory Agency (MHRA) advises discontinuing these GLP-1 receptor agonists if pregnancy is planned or confirmed. Limited human safety data and concerns from animal studies mean these medications should be stopped before conception—typically at least two months beforehand for semaglutide. If you are pregnant, planning pregnancy, or breastfeeding, speak to your GP immediately about safe alternatives for managing weight and metabolic health that prioritise both maternal and foetal wellbeing.
Summary: No, weight loss injections such as semaglutide, liraglutide, and tirzepatide should not be taken during pregnancy due to insufficient human safety data and potential developmental risks identified in animal studies.
- GLP-1 receptor agonists work by mimicking hormones that regulate appetite and blood glucose but are contraindicated in pregnancy.
- Semaglutide should be discontinued at least two months before planned conception; liraglutide when planning pregnancy.
- Animal studies have shown potential reproductive toxicity including reduced foetal growth and skeletal abnormalities at therapeutic doses.
- Pregnancy requires appropriate weight gain rather than weight loss to support healthy foetal development and maternal nutrition.
- If pregnancy occurs whilst taking these medications, stop immediately and contact your GP or maternity service for monitoring and support.
- Insulin remains the gold-standard treatment for diabetes management during pregnancy due to its established safety profile.
Table of Contents
Weight Loss Injections and Pregnancy: Safety Overview
Weight loss injections, particularly GLP-1 receptor agonists such as semaglutide (Wegovy, Ozempic), liraglutide (Saxenda), and tirzepatide (Mounjaro), should not be used during pregnancy. The Medicines and Healthcare products Regulatory Agency (MHRA) and manufacturers advise discontinuing these medications if pregnancy is planned or confirmed. Current evidence is insufficient to establish their safety profile in pregnant women, and animal studies have raised concerns about potential developmental risks.
These medications work by mimicking the hormone glucagon-like peptide-1 (GLP-1), which regulates appetite and blood glucose levels. They slow gastric emptying, increase feelings of fullness, and reduce food intake. Whilst effective for weight management in non-pregnant adults, pregnancy represents a unique physiological state where maternal nutrition directly impacts foetal development. Weight loss during pregnancy is generally not advised unless under specific medical supervision, as adequate maternal weight gain supports healthy foetal growth.
The primary concern centres on limited human data. Clinical trials systematically exclude pregnant women for ethical reasons, meaning safety information derives mainly from animal studies and inadvertent exposures reported through pharmacovigilance systems. UK product licences state these agents should not be used during pregnancy. Healthcare professionals emphasise that any woman of childbearing potential using weight loss injections should employ reliable contraception and discontinue treatment before attempting conception.
These medications are also generally not recommended during breastfeeding, as it's unknown whether they pass into breast milk or what effects they might have on the infant.
If you are pregnant, breastfeeding, or planning pregnancy, it is essential to discuss your medication regimen with your GP or specialist. Alternative approaches to managing weight and metabolic health exist that are compatible with pregnancy and prioritise both maternal and foetal wellbeing.
Risks of GLP-1 Receptor Agonists in Pregnancy
Animal studies have demonstrated potential reproductive toxicity with GLP-1 receptor agonists, though there is no official link definitively established in humans. In preclinical research, exposure during pregnancy resulted in reduced foetal growth, skeletal abnormalities, and increased pregnancy loss in some species at doses comparable to or higher than human therapeutic levels. These findings prompted regulatory agencies to advise against use in pregnancy, with manufacturers providing specific recommendations for discontinuation before planned conception.
For women planning pregnancy, discontinuation timing varies by medication:
-
Semaglutide (Wegovy, Ozempic): Stop at least 2 months before planned conception
-
Tirzepatide (Mounjaro): Follow SmPC guidance (typically around 1 month)
-
Liraglutide (Saxenda): No fixed period is specified, but discontinue when planning pregnancy
There are theoretical concerns related to these medications during pregnancy. GLP-1 receptors are found in various tissues, and some research suggests they may be present in placental tissue. It is theoretically possible these medications could affect placental function or nutrient transfer, though this remains speculative. Additionally, the appetite-suppressing effects may lead to inadequate maternal nutrition, which itself poses risks including intrauterine growth restriction, low birth weight, and developmental complications. Pregnancy requires increased caloric and nutritional intake to support foetal development, making intentional weight loss potentially harmful.
Women using tirzepatide should be aware it may reduce the effectiveness of oral contraceptives, particularly during dose initiation or escalation. Additional contraceptive methods may be advisable during these periods.
Limited human data exists from inadvertent exposures. Pregnancy registries and post-marketing surveillance have documented cases where women became pregnant whilst taking these medications, but numbers remain too small to draw definitive conclusions about safety. Available reports have not identified a consistent pattern of birth defects, but this does not confirm safety—merely reflects insufficient data. The absence of evidence is not evidence of absence.
Other considerations include the medications' effects on maternal glucose metabolism. Whilst glycaemic control is crucial in pregnancy, particularly for women with gestational or pre-existing diabetes, insulin remains the gold-standard treatment during pregnancy due to its established safety profile. NICE guidelines recommend insulin for diabetes management in pregnancy, with metformin considered in specific circumstances. GLP-1 agonists are not among recommended options for pregnant women, even those with diabetes.
Safe Weight Management Approaches During Pregnancy
Pregnancy is not an appropriate time for weight loss, but healthy weight management remains important. NICE guidance emphasises that women should aim for appropriate gestational weight gain based on their pre-pregnancy body mass index (BMI), rather than weight reduction. For women with obesity, this typically means gaining less weight than those starting at healthy weights, but still gaining some weight to support foetal development.
Recommended approaches include:
-
Balanced nutrition: Focus on nutrient-dense foods providing essential vitamins, minerals, protein, and healthy fats. The NHS Eatwell Guide offers pregnancy-specific advice emphasising fruits, vegetables, whole grains, lean proteins, and dairy products whilst limiting processed foods, added sugars, and saturated fats.
-
Regular physical activity: Unless contraindicated, pregnant women should aim for 150 minutes of moderate-intensity activity weekly, such as walking, swimming, or pregnancy-specific exercise classes. Physical activity supports healthy weight gain, reduces gestational diabetes risk, and improves overall wellbeing.
-
Portion awareness: Rather than restrictive dieting, focus on appropriate portion sizes and eating in response to hunger cues. Pregnancy increases caloric needs by approximately 200 calories daily in the third trimester, but requirements vary individually.
-
Professional support: Women with obesity or concerns about weight should access specialist antenatal care. Midwives, obstetricians, and dietitians can provide personalised guidance. Some NHS trusts offer specialist weight management services for pregnant women.
Gestational diabetes screening is particularly important for women with risk factors such as elevated BMI (≥30), previous gestational diabetes, family history of diabetes, or certain ethnic backgrounds. Testing is typically performed between 24-28 weeks. If diagnosed, dietary modifications and physical activity form first-line management, with insulin added if needed. This approach manages blood glucose without compromising foetal nutrition.
Avoid restrictive diets, fasting, or unproven supplements during pregnancy. Any nutritional changes should be discussed with healthcare professionals to ensure maternal and foetal nutritional needs are met.
What to Do If You Become Pregnant While Taking Weight Loss Injections
If you discover you are pregnant whilst taking weight loss injections, stop the medication immediately and contact your GP or maternity service as soon as possible. Do not delay seeking advice due to concern about judgement—healthcare professionals prioritise your health and your baby's wellbeing. Early disclosure allows appropriate monitoring and support throughout pregnancy.
Your healthcare team will likely:
-
Review your medication history: Document the type of injection, dosage, duration of use, and timing relative to conception. This information helps assess potential exposure during critical developmental periods.
-
Arrange appropriate antenatal care: Based on individual risk assessment, you may be referred to consultant-led care rather than midwife-led care, particularly if you have additional risk factors such as obesity or diabetes. Your care plan, including whether additional ultrasound scans are needed, will be tailored to your specific situation.
-
Provide reassurance and information: Whilst these medications are not recommended in pregnancy, inadvertent exposure does not automatically indicate harm will occur. Your healthcare team will explain what is known about risks and what monitoring is appropriate for your situation.
-
Optimise your health: Focus shifts to supporting healthy pregnancy through nutrition, appropriate physical activity, and management of any underlying conditions such as diabetes or hypertension.
Report your exposure to the MHRA's Yellow Card Scheme (yellowcard.mhra.gov.uk), which collects information about suspected side effects and medication use in pregnancy. This pharmacovigilance data helps build understanding of medication safety profiles. Your healthcare provider can assist with this reporting.
Plan for future contraception: If you wish to resume weight loss injections after pregnancy, discuss reliable contraception with your GP. These medications should be discontinued before any future planned pregnancies, with specific timing depending on the medication:
-
Semaglutide: at least 2 months before conception
-
Tirzepatide: follow current SmPC guidance
-
Liraglutide: discontinue when planning pregnancy
Remember that many women have healthy pregnancies despite inadvertent medication exposures. The key is engaging with healthcare services early, attending all recommended appointments, and following professional guidance throughout your pregnancy and postpartum period.
Frequently Asked Questions
How long before trying to conceive should I stop weight loss injections?
For semaglutide (Wegovy, Ozempic), stop at least two months before planned conception. Liraglutide (Saxenda) should be discontinued when planning pregnancy, whilst tirzepatide (Mounjaro) typically requires around one month—follow current SmPC guidance and consult your GP for personalised advice.
What should I do if I discover I'm pregnant whilst taking weight loss injections?
Stop the medication immediately and contact your GP or maternity service as soon as possible. Your healthcare team will arrange appropriate antenatal monitoring, provide reassurance, and help you report the exposure to the MHRA Yellow Card Scheme to contribute to safety data.
Are there safe alternatives for managing weight during pregnancy?
Yes—focus on balanced nutrition following the NHS Eatwell Guide, regular moderate physical activity (150 minutes weekly unless contraindicated), and appropriate gestational weight gain based on your pre-pregnancy BMI. Specialist antenatal care and dietitian support are available through the NHS for women with obesity or metabolic concerns.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript