Weight loss injections such as semaglutide (Wegovy) and liraglutide (Saxenda) are increasingly used for weight management, but their safety during breastfeeding remains a critical concern for new mothers. Current UK guidance is unequivocal: these medications should not be used whilst breastfeeding due to insufficient human safety data and unknown effects on nursing infants. The lack of robust clinical evidence regarding transfer into breast milk, combined with potential impacts on maternal nutrition and infant development, means healthcare professionals consistently advise against their use during lactation. This article examines the safety considerations, potential risks, and evidence-based alternatives for postpartum weight management that protect both maternal and infant health.
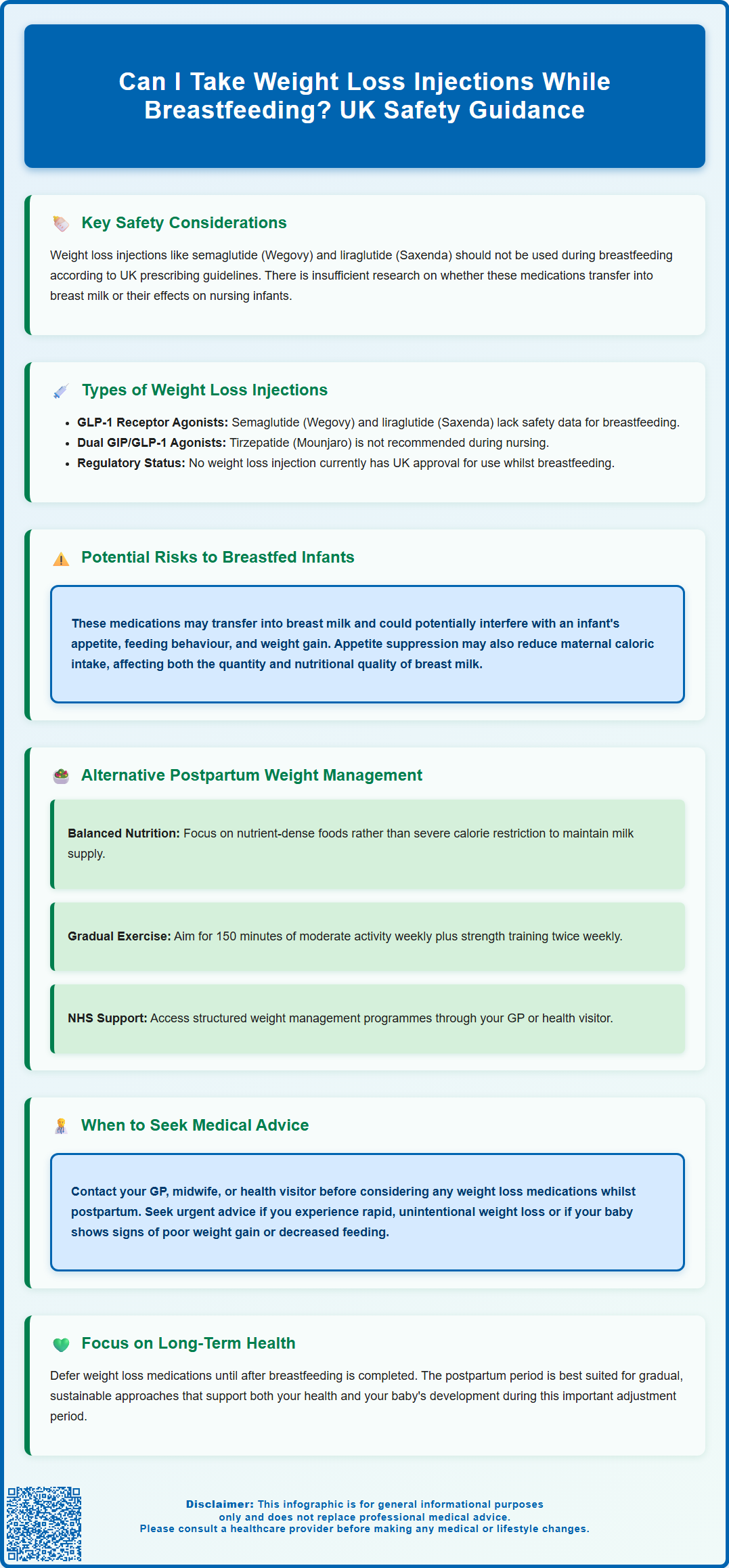
Summary: Weight loss injections including semaglutide and liraglutide should not be used during breastfeeding according to UK prescribing guidance due to lack of human safety data.
- GLP-1 receptor agonists (semaglutide, liraglutide, tirzepatide) are contraindicated during breastfeeding per UK Summary of Product Characteristics
- No weight loss injection currently has regulatory approval for use whilst breastfeeding in the UK
- Transfer into breast milk and effects on nursing infants remain unknown due to absence of human studies
- Appetite suppression from these medications may compromise maternal nutrition needed for adequate milk production
- Safe alternatives include gradual dietary modification, regular physical activity, and NHS weight management programmes
- Women should defer weight loss medications until breastfeeding is completed and seek GP advice for postpartum weight concerns
Table of Contents
- Weight Loss Injections and Breastfeeding: Key Safety Considerations
- Types of Weight Loss Injections and Their Use During Lactation
- Potential Risks to Breastfed Infants
- Alternative Approaches to Postpartum Weight Management
- When to Seek Medical Advice About Weight Loss While Breastfeeding
- Frequently Asked Questions
Weight Loss Injections and Breastfeeding: Key Safety Considerations
Weight loss injections, particularly GLP-1 receptor agonists such as semaglutide (Wegovy) and liraglutide (Saxenda), have become increasingly popular for weight management. However, their use during breastfeeding raises significant safety concerns that require careful consideration.
Current guidance from UK product information is clear: these medications should not be used during breast-feeding. The UK Summary of Product Characteristics (SmPC) for semaglutide, liraglutide and tirzepatide specifically states they should not be used during breast-feeding due to lack of human data. The manufacturers' prescribing information explicitly advises against their use whilst breastfeeding.
The primary concern centres on the lack of robust clinical data . Studies examining the transfer of weight loss injections into human breast milk are extremely limited, and there is no established safety profile for exposed infants. Given that breastfeeding provides crucial nutritional and immunological benefits to infants, any medication that could potentially compromise infant health or milk supply requires thorough evaluation.
Additionally, these medications work by suppressing appetite and slowing gastric emptying, which could theoretically affect maternal nutrition and, consequently, breast milk quality and quantity. Adequate maternal nutrition is essential for maintaining milk production, and significant calorie restriction—whether medication-induced or dietary—may potentially compromise lactation. Healthcare professionals consistently advise that the postpartum period, particularly whilst breastfeeding, is not the optimal time to pursue aggressive weight loss interventions.
Types of Weight Loss Injections and Their Use During Lactation
Several types of weight loss injections are currently available in the UK, each with distinct mechanisms of action and safety profiles. Understanding these differences is important when considering their compatibility with breastfeeding.
GLP-1 receptor agonists represent the most commonly prescribed weight loss injections. Semaglutide (Wegovy) and liraglutide (Saxenda) work by mimicking the glucagon-like peptide-1 hormone, which regulates appetite and food intake. These medications are administered via subcutaneous injection, typically weekly (semaglutide) or daily (liraglutide). According to their UK SmPCs, these medications should not be used during breast-feeding. Animal studies have shown excretion into milk, but human data remains absent.
Tirzepatide (Mounjaro), a dual GIP/GLP-1 receptor agonist approved for type 2 diabetes, similarly lacks safety data for breastfeeding women. The UK SmPC advises that tirzepatide should not be used during breast-feeding due to unknown transfer into breast milk and potential effects on the nursing infant.
Other injectable medications occasionally used for metabolic management include liraglutide at lower doses for type 2 diabetes (Victoza), though this is primarily indicated for glycaemic control rather than weight loss. The breastfeeding guidance remains consistent: these medications should not be used during breast-feeding. For women requiring diabetes management during breastfeeding, alternative agents such as insulin or metformin may be considered under specialist supervision.
It is worth noting that no weight loss injection currently has regulatory approval for use during breastfeeding in the UK. Women who become pregnant whilst taking these medications are advised to discontinue them, and this guidance extends through the breastfeeding period. Any woman considering these treatments should complete breastfeeding first or choose alternative weight management strategies.
Potential Risks to Breastfed Infants
The potential risks to breastfed infants from maternal use of weight loss injections remain largely theoretical due to the absence of comprehensive human studies. However, several concerns warrant serious consideration based on the pharmacological properties of these medications.
Transfer into breast milk is the primary concern. Whilst GLP-1 analogues are large peptide molecules that theoretically have limited transfer into milk, animal studies have demonstrated their presence in the milk of lactating rats. The extent of human milk transfer, bioavailability to the infant, and potential systemic effects remain unknown. Given that infants' gastrointestinal and metabolic systems are immature, even small exposures could theoretically affect glucose regulation, growth, or feeding patterns.
Impact on infant feeding and growth represents another significant concern. If these medications do reach the infant through breast milk, they could potentially affect the baby's appetite, feeding behaviour, or weight gain. Normal infant weight gain and feeding patterns are critical indicators of health during the first year of life, and any interference with these processes could have developmental consequences.
Maternal nutritional status may be indirectly compromised by these medications' appetite-suppressing effects. Breastfeeding women require additional calories to support milk production. If a mother's caloric intake becomes severely restricted due to medication-induced appetite suppression, this could theoretically affect both milk quantity and nutritional quality, potentially impacting infant nutrition.
Hypoglycaemia risk in the infant, whilst theoretical, cannot be excluded. It's worth noting that GLP-1 receptor agonists typically have a low risk of causing hypoglycaemia in adults when used alone, but any transfer to the infant could potentially influence blood sugar regulation in vulnerable newborns.
The precautionary principle underpins the SmPC statements that these medications should not be used during breast-feeding. Until robust safety data becomes available, avoiding these medications during breastfeeding is the recommended approach to protect infant health.
Alternative Approaches to Postpartum Weight Management
Breastfeeding women seeking to manage their weight have several evidence-based alternatives that do not pose risks to their nursing infants. These approaches align with NHS and NICE guidance on postpartum care and healthy weight management.
Gradual, balanced dietary modification represents the safest first-line approach. Rather than severe calorie restriction, aim for gradual, sustainable weight loss without compromising milk supply. Focus on nutrient-dense foods including fruits, vegetables, whole grains, lean proteins, and healthy fats. The NHS Eatwell Guide provides an excellent framework for balanced nutrition during lactation. Avoid fad diets or extreme restrictions, as these may affect milk production and maternal wellbeing.
Regular physical activity offers numerous benefits for postpartum women. The UK Chief Medical Officers' guidelines recommend at least 150 minutes of moderate-intensity activity weekly when you feel ready, along with pelvic floor exercises and muscle-strengthening activities on two or more days per week. Exercise supports weight management, improves mood, enhances cardiovascular health, and does not adversely affect breast milk composition or volume when combined with adequate nutrition and hydration. Start gradually, particularly after caesarean delivery, and seek guidance from a physiotherapist if experiencing pelvic floor concerns.
Breastfeeding itself contributes to postpartum weight loss, as lactation requires additional calories daily. Many women find that exclusive breastfeeding facilitates gradual return to pre-pregnancy weight, though individual responses vary considerably.
Behavioural support programmes such as those offered through NHS weight management services can provide structure, accountability, and evidence-based strategies. These programmes typically address eating behaviours, activity levels, and psychological factors affecting weight management. Availability varies by region, so discuss referral options with your GP or health visitor. NHS-endorsed resources like the NHS Weight Loss Plan can also provide structured guidance compatible with breastfeeding needs.
When to Seek Medical Advice About Weight Loss While Breastfeeding
Certain situations warrant prompt medical consultation to ensure both maternal and infant health are appropriately supported during the postpartum period.
Contact your GP, midwife or health visitor if you are struggling with postpartum weight concerns and considering weight loss medications. A healthcare professional can assess your individual circumstances, discuss realistic timelines for weight management, screen for underlying conditions affecting weight (such as thyroid disorders), and provide referrals to appropriate services. They can also evaluate whether any weight retention relates to medical conditions requiring specific treatment.
Seek urgent advice if you experience rapid, unintentional weight loss whilst breastfeeding, as this may indicate inadequate caloric intake, illness, or postpartum thyroid dysfunction. Similarly, if your infant shows signs of poor weight gain, decreased feeding, fewer wet nappies, not regaining birth weight by 2 weeks, unusual lethargy, or other concerning symptoms, immediate medical assessment is essential. For urgent concerns, contact your GP, NHS 111, or emergency services if appropriate.
Discuss with your healthcare provider before starting any weight loss programme, supplement, or medication whilst breastfeeding. This includes over-the-counter products, herbal preparations, or medications obtained privately, as many substances can transfer into breast milk. Your GP can advise on safety and appropriateness for your specific situation.
Consider specialist referral if you have significant weight concerns affecting your physical or mental health. This might include referral to a dietitian for personalised nutritional guidance, a weight management service for structured support, or mental health services if body image concerns or disordered eating patterns are present. Postpartum mental health is intrinsically linked to physical wellbeing, and addressing both aspects holistically optimises outcomes.
Remember: the postpartum period is a time of significant physical and emotional adjustment. Prioritising gradual, sustainable approaches to weight management that support both your health and your baby's development is far more beneficial than pursuing rapid weight loss through medications that should not be used during breast-feeding. Any decision regarding weight loss medicines should be deferred until breastfeeding is completed.
If you experience any suspected adverse effects from medications, report them via the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Frequently Asked Questions
Are weight loss injections like Wegovy safe during breastfeeding?
No, weight loss injections including Wegovy (semaglutide) and Saxenda (liraglutide) should not be used during breastfeeding according to UK prescribing information. There is insufficient human safety data regarding transfer into breast milk and potential effects on nursing infants.
What are safe alternatives for weight loss whilst breastfeeding?
Safe alternatives include gradual dietary modification following the NHS Eatwell Guide, regular physical activity (150 minutes weekly of moderate-intensity exercise), and NHS weight management programmes. Breastfeeding itself supports postpartum weight loss through increased caloric expenditure.
When can I start weight loss injections after having a baby?
Weight loss injections should only be considered after you have completely finished breastfeeding. Discuss timing and suitability with your GP, who can assess your individual circumstances and ensure any underlying health conditions are addressed first.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript