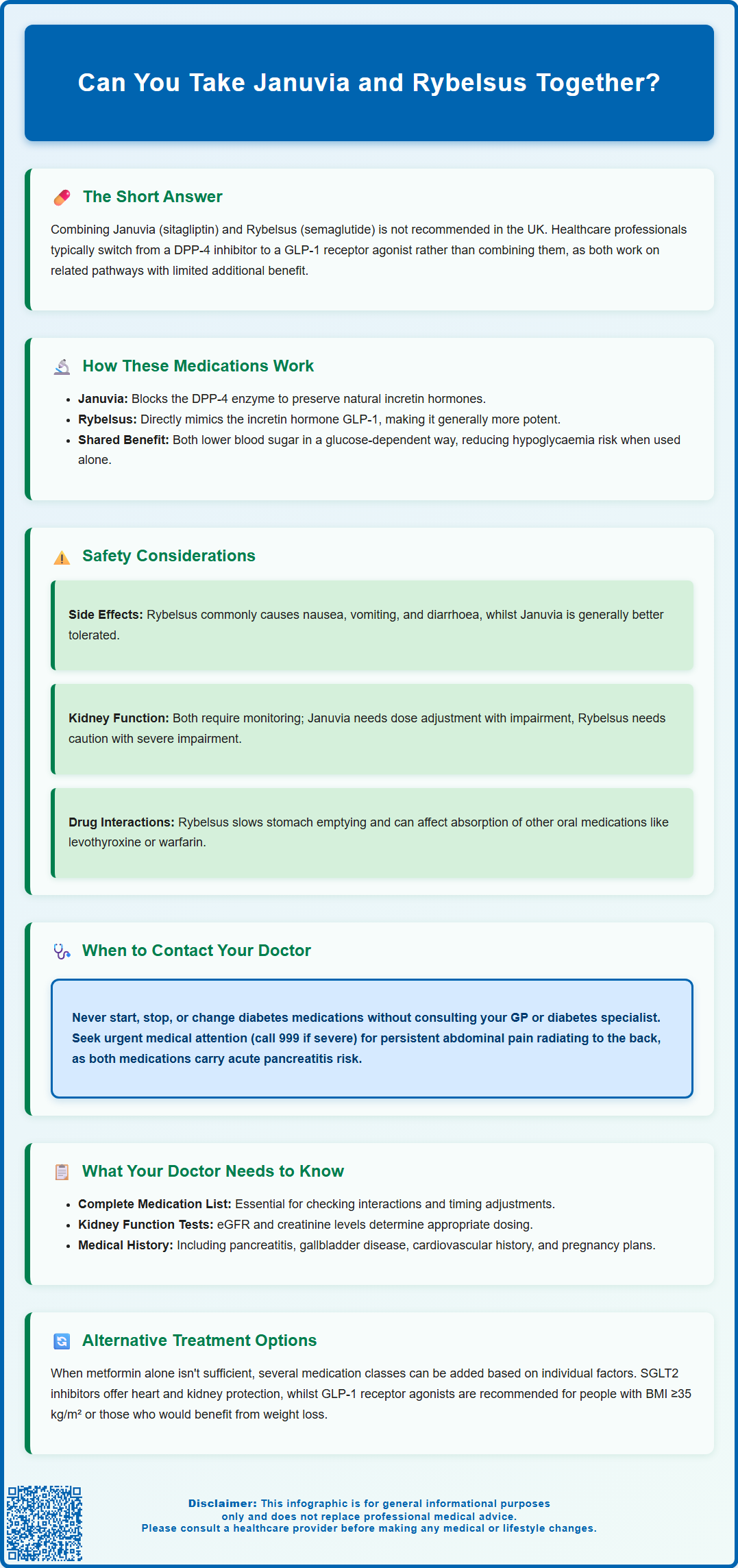
Can you take Januvia and Rybelsus together for type 2 diabetes? In the UK, combining Januvia (sitagliptin) and Rybelsus (semaglutide) is generally not recommended according to current clinical guidance. These medications belong to different classes—DPP-4 inhibitors and GLP-1 receptor agonists—that work on related pathways. UK guidance from NICE and the NHS Specialist Pharmacy Service advises against this combination due to limited additional benefit and poor cost-effectiveness. Healthcare professionals typically consider switching from one medication to the other, rather than combining them, when treatment intensification is needed. Any changes to your diabetes medication regimen should only be made under medical supervision.
Summary: Combining Januvia (sitagliptin) and Rybelsus (semaglutide) is generally not recommended in the UK due to limited additional benefit and poor cost-effectiveness.
- Januvia is a DPP-4 inhibitor that blocks the enzyme breaking down natural incretin hormones, whilst Rybelsus is a GLP-1 receptor agonist that directly mimics incretin action.
- NICE guidance (NG28) and NHS Specialist Pharmacy Service advise against combining these medications as they work on related pathways.
- Healthcare professionals typically switch from a DPP-4 inhibitor to a GLP-1 receptor agonist when treatment intensification is needed, rather than combining them.
- Both medications require consideration of kidney function, with Januvia requiring dose adjustment when eGFR falls below 45 mL/min/1.73m².
- Alternative treatment options include SGLT2 inhibitors, which offer cardiovascular and renal protective benefits alongside glucose control.
- Any changes to diabetes medication regimens must be made under medical supervision to avoid dangerous blood sugar fluctuations.
Table of Contents
Can You Take Januvia and Rybelsus Together?
In the UK, combining Januvia (sitagliptin) and Rybelsus (semaglutide) is generally not recommended according to current clinical guidance. These medications belong to different classes—DPP-4 inhibitors and GLP-1 receptor agonists respectively—that work on related pathways. UK guidance (NICE NG28) and NHS Specialist Pharmacy Service advise against this combination due to limited additional benefit and poor cost-effectiveness.
Rather than combining these medications, healthcare professionals typically consider switching from a DPP-4 inhibitor to a GLP-1 receptor agonist when intensification of treatment is needed. Alternative approaches might include adding an SGLT2 inhibitor to existing therapy, in line with NICE recommendations and local formulary guidelines.
The decision about which diabetes medications are appropriate for you depends on several factors, including your current blood glucose control, other medications you're taking, existing health conditions (particularly kidney function), and your overall treatment goals. Your treatment should be individualised based on these considerations.
It is essential to understand that diabetes medication regimens require careful monitoring and should only be adjusted under medical supervision. Both Januvia and Rybelsus affect how your body manages blood sugar, and any changes to your treatment plan should be made by your healthcare team.
Never start, stop, or change diabetes medications without consulting your GP or diabetes specialist. Self-adjusting your diabetes treatment can lead to dangerous blood sugar fluctuations, either too high (hyperglycaemia) or too low (hypoglycaemia), both of which can have serious health consequences. Always discuss any concerns about your diabetes management with a qualified healthcare professional.
How Januvia and Rybelsus Work in Type 2 Diabetes
Januvia (sitagliptin) belongs to a class of medications called DPP-4 inhibitors (dipeptidyl peptidase-4 inhibitors). It works by blocking the DPP-4 enzyme, which normally breaks down incretin hormones in the body. Incretins are natural substances that help regulate blood sugar by stimulating insulin release when glucose levels are elevated and reducing the amount of glucose produced by the liver. By inhibiting DPP-4, Januvia prolongs the action of these incretins, leading to improved blood glucose control. The medication is typically taken once daily as a 100mg tablet (or 50mg or 25mg in people with reduced kidney function).
Rybelsus (semaglutide) is a GLP-1 receptor agonist (glucagon-like peptide-1 receptor agonist), which mimics the action of the natural incretin hormone GLP-1. Unlike Januvia, which prevents the breakdown of natural incretins, Rybelsus directly activates GLP-1 receptors. This activation stimulates insulin secretion in a glucose-dependent manner, suppresses glucagon release (which reduces glucose production by the liver), slows gastric emptying, and promotes satiety. Rybelsus is the first oral GLP-1 receptor agonist and requires specific administration: it must be taken on an empty stomach with up to 120ml of water, swallowed whole, and followed by at least 30 minutes before eating, drinking or taking other oral medications.
The key difference between these medications lies in their mechanisms: Januvia enhances your body's own incretin system, whilst Rybelsus provides a synthetic incretin-like effect that is generally more potent. Both medications have a glucose-dependent action, meaning they work primarily when blood sugar levels are elevated, which reduces the risk of hypoglycaemia when used alone.
According to NICE guidance (NG28), both medications are recommended as treatment options for type 2 diabetes in specific circumstances, typically as second- or third-line therapies when metformin alone is insufficient or not tolerated. However, despite their different mechanisms, NICE does not recommend using them together. For Rybelsus, treatment typically starts with a 3mg daily dose for 30 days, then increases to 7mg daily, with a possible further increase to 14mg daily if needed for glycaemic control.
Safety Considerations When Combining These Medications
Although combining Januvia and Rybelsus is not generally recommended in UK practice, understanding the safety profile of each medication is important. The most significant concern with Rybelsus is gastrointestinal side effects, including nausea, vomiting, diarrhoea, abdominal pain, and decreased appetite. These effects are usually most pronounced when starting treatment or increasing the dose. Januvia is generally well-tolerated but can occasionally cause gastrointestinal symptoms as well.
The risk of hypoglycaemia (low blood sugar) is generally low with either medication when used without other glucose-lowering agents, as both have glucose-dependent mechanisms of action. However, if you're also taking insulin or a sulphonylurea (such as gliclazide), the risk of hypoglycaemia increases significantly. Symptoms of hypoglycaemia include trembling, sweating, confusion, palpitations, and hunger. If you experience these symptoms, check your blood glucose if possible and consume fast-acting carbohydrates (such as glucose tablets or fruit juice).
Both medications require consideration of kidney function. Januvia doses must be adjusted in people with moderate to severe kidney impairment, whilst Rybelsus should be used with caution in those with severe renal impairment. Your doctor will check your kidney function (eGFR) before prescribing and periodically during treatment. Additionally, there have been reports of acute pancreatitis associated with both DPP-4 inhibitors and GLP-1 receptor agonists. If you experience severe, persistent abdominal pain, which may radiate to the back, with or without vomiting, seek urgent medical attention or call 999 if symptoms are severe.
Rybelsus has additional safety considerations including potential worsening of diabetic retinopathy (particularly with rapid improvement in blood glucose control), risk of dehydration from gastrointestinal effects, increased risk of gallbladder disease, and caution in people with severe gastrointestinal disease or gastroparesis. Animal studies have shown thyroid C-cell tumours with semaglutide, though the relevance to humans is unknown.
Rybelsus can affect the absorption of other medications due to delayed gastric emptying and may increase exposure to levothyroxine (thyroid medication), potentially requiring TSH monitoring. If you take warfarin, your doctor may recommend more frequent INR monitoring. If you experience any suspected side effects, report them to the MHRA Yellow Card scheme, which helps monitor medication safety.
What Your Doctor Needs to Know Before Prescribing Both
Before your doctor prescribes any diabetes medication, they will need comprehensive information about your medical history and current health status. This includes your complete medication list, as drug interactions can affect the safety and efficacy of treatment. Rybelsus, in particular, can affect the absorption of other oral medications due to its effect on gastric emptying. Medications that require rapid absorption may need to be taken at different times.
Your kidney function is a critical consideration. Your doctor will review recent blood tests showing your estimated glomerular filtration rate (eGFR) and serum creatinine levels. Januvia requires dose adjustment when eGFR falls below 45 mL/min/1.73m², with a reduced dose of 50mg daily for moderate impairment (eGFR 30-45) and 25mg daily for severe impairment (eGFR below 30). Rybelsus has limited data in severe renal impairment and is not recommended when eGFR is below 15 mL/min/1.73m² or in end-stage renal disease.
Your cardiovascular history and risk factors are also important. Some injectable GLP-1 receptor agonists (such as liraglutide, dulaglutide, and injectable semaglutide) have demonstrated cardiovascular benefits in clinical trials. While oral semaglutide has not yet demonstrated superiority in cardiovascular outcomes, your cardiovascular status may influence treatment decisions. Your doctor will also need to know about any history of pancreatitis, as both medication classes have been associated with this condition.
Information about your diabetes control and treatment goals is essential. Your doctor will review your recent HbA1c levels (a measure of average blood glucose over the previous 2-3 months), your current diabetes medications and doses, any history of hypoglycaemic episodes, and your ability to recognise and manage low blood sugar. They'll also consider practical factors such as your ability to take Rybelsus correctly (on an empty stomach, with water, 30 minutes before eating), any difficulties swallowing tablets, and your preferences regarding treatment.
Additional important information includes: your diabetic retinopathy status and recent eye screening results, any history of gallbladder disease, pregnancy status or plans (GLP-1 receptor agonists are not recommended during pregnancy or breastfeeding and should be discontinued at least two months before a planned pregnancy), and any history of severe gastrointestinal disease or gastroparesis. NICE recommends individualised HbA1c targets, typically 48 mmol/mol (6.5%) for most people, though this may be relaxed to 53 mmol/mol (7.0%) or higher in certain circumstances.
Alternative Treatment Options for Type 2 Diabetes
Several alternative treatment strategies are available for managing type 2 diabetes when current therapy is insufficient. The choice of treatment depends on multiple factors including your HbA1c level, body weight, cardiovascular risk, kidney function, risk of hypoglycaemia, and personal preferences. NICE provides comprehensive guidance on the stepwise approach to managing type 2 diabetes.
Metformin remains the first-line treatment for most people with type 2 diabetes, unless contraindicated or not tolerated. It works by reducing glucose production in the liver and improving insulin sensitivity. When metformin alone is insufficient, NICE recommends considering the addition of one of several medication classes:
-
SGLT2 inhibitors (such as dapagliflozin, empagliflozin, or canagliflozin) work by increasing glucose excretion through the kidneys. They offer cardiovascular and renal protective benefits and may promote modest weight loss. These are particularly recommended for people with established cardiovascular disease, heart failure, or chronic kidney disease.
-
GLP-1 receptor agonists are recommended by NICE when BMI is ≥35 kg/m² (or lower in people of Black African, African-Caribbean, or South Asian family origin) or for whom weight loss would benefit obesity-related comorbidities. NICE specifies that GLP-1 receptor agonists should only be continued if there is a reduction in HbA1c of at least 11 mmol/mol (1.0%) and weight loss of at least 3% at 6 months. Injectable formulations (such as dulaglutide, liraglutide, or exenatide) are alternatives to Rybelsus.
-
DPP-4 inhibitors (such as sitagliptin, linagliptin, or alogliptin) are weight-neutral and have a low risk of hypoglycaemia. They are often used as second-line therapy, particularly in older adults or those at risk of hypoglycaemia.
-
Thiazolidinediones (pioglitazone) improve insulin sensitivity but may cause weight gain and fluid retention, making them unsuitable for people with heart failure.
-
Sulphonylureas (such as gliclazide) stimulate insulin release but carry a risk of hypoglycaemia and weight gain. They are less commonly used as second-line agents now but remain an option, particularly where cost is a consideration.
For people requiring more intensive glucose control, triple therapy (metformin plus two other agents from different classes, but not combining DPP-4 inhibitors with GLP-1 receptor agonists) or insulin therapy may be necessary. Basal insulin (such as insulin glargine or insulin detemir) can be added to oral medications, with or without short-acting insulin at mealtimes depending on glucose control.
Lifestyle modifications remain fundamental to diabetes management regardless of medication choices. A healthy diet, regular physical activity, weight management (if appropriate), and smoking cessation all contribute significantly to glucose control and reduce cardiovascular risk. NICE recommends referral to structured education programmes (such as DESMOND for type 2 diabetes) to support self-management skills. If you're struggling to achieve your treatment goals or experiencing side effects from your current medications, discuss alternative options with your GP or diabetes specialist nurse.
Frequently Asked Questions
Why aren't Januvia and Rybelsus recommended together?
UK guidance advises against combining Januvia (a DPP-4 inhibitor) and Rybelsus (a GLP-1 receptor agonist) because they work on related pathways, offering limited additional benefit with poor cost-effectiveness. Healthcare professionals typically switch from one to the other rather than combining them.
What is the main difference between Januvia and Rybelsus?
Januvia blocks the DPP-4 enzyme to prolong the action of your body's natural incretin hormones, whilst Rybelsus directly mimics the action of the incretin hormone GLP-1. Rybelsus generally provides a more potent effect and may promote weight loss, whereas Januvia is weight-neutral.
What are the alternatives if my current diabetes medication isn't working?
Alternative options include SGLT2 inhibitors (which offer cardiovascular and renal benefits), switching from a DPP-4 inhibitor to a GLP-1 receptor agonist, adding insulin therapy, or considering other medication classes based on your individual circumstances. Your GP or diabetes specialist will recommend the most appropriate option for you.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript