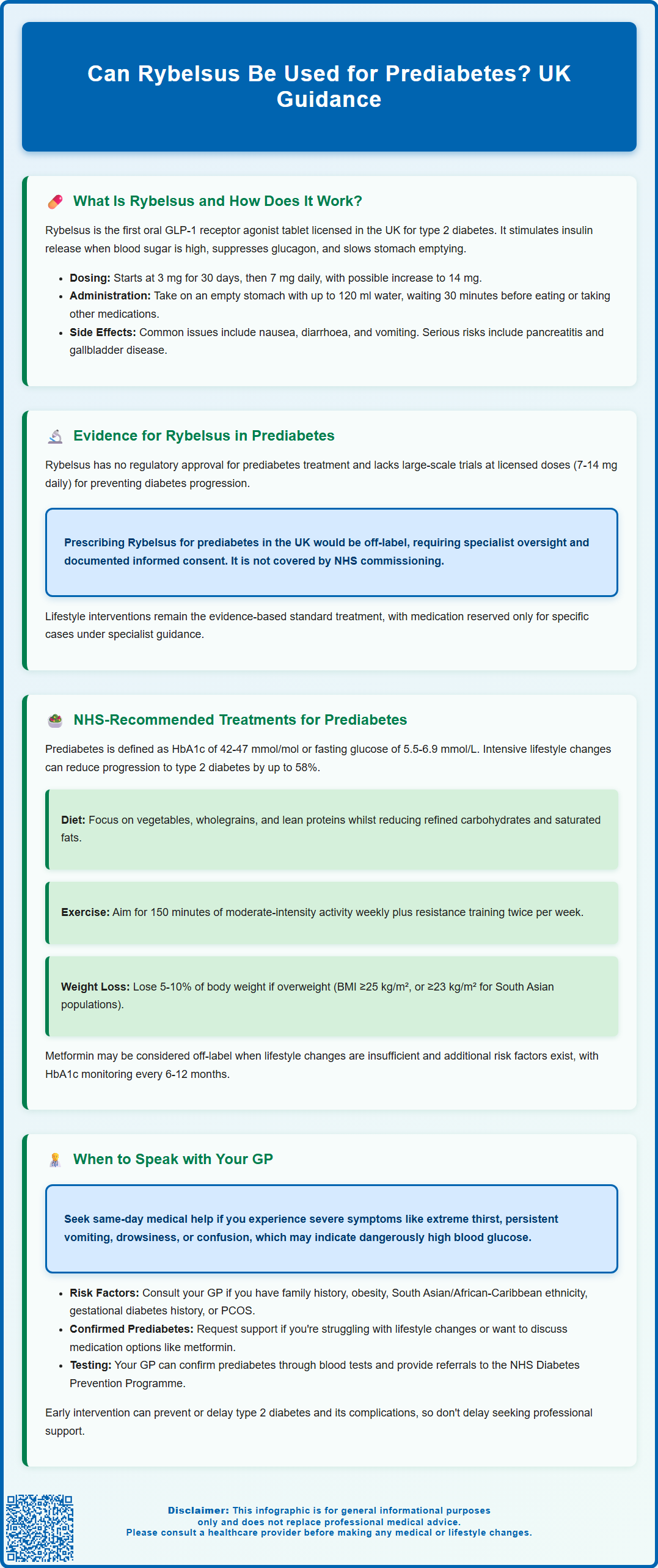
Rybelsus (semaglutide) is an oral GLP-1 receptor agonist licensed in the UK exclusively for treating type 2 diabetes mellitus in adults. Whilst some research has explored whether GLP-1 medications might delay progression from prediabetes to diabetes, Rybelsus is not currently approved by the MHRA or recommended by NICE for prediabetes management. Prescribing it for this purpose would be off-label, and evidence specific to Rybelsus at licensed doses in prediabetic populations remains limited. This article examines the current evidence, NHS-recommended treatments for prediabetes, and when to seek professional advice about blood sugar control.
Summary: Rybelsus is not licensed or recommended for prediabetes treatment in the UK and prescribing it for this purpose would be off-label.
- Rybelsus (semaglutide) is a GLP-1 receptor agonist licensed exclusively for type 2 diabetes mellitus in adults.
- No large-scale trials have evaluated Rybelsus at licensed doses (7 mg or 14 mg daily) specifically for prediabetes prevention.
- NICE recommends intensive lifestyle modification as first-line management for prediabetes, with metformin considered only in specific high-risk circumstances.
- Off-label prescribing requires specialist guidance, documented informed consent, and is not commissioned by the NHS for prediabetes.
- Common adverse effects include gastrointestinal symptoms, with rare but serious risks including pancreatitis and gallbladder disease.
- Regular HbA1c monitoring every 6–12 months is advised to detect progression to diabetes and adjust management accordingly.
Table of Contents
What Is Rybelsus and How Does It Work?
Rybelsus (semaglutide) is an oral medication licensed in the UK for the treatment of type 2 diabetes mellitus in adults. It belongs to a class of drugs called glucagon-like peptide-1 (GLP-1) receptor agonists, which mimic the action of a naturally occurring hormone that regulates blood glucose levels. Rybelsus is the first GLP-1 receptor agonist available in tablet form, offering an alternative to injectable formulations such as Ozempic (which contains the same active ingredient but differs in route of administration and dosing).
The mechanism of action involves several complementary pathways. Semaglutide stimulates insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning it only promotes insulin release when blood sugar levels are elevated. This reduces the risk of hypoglycaemia compared with some other diabetes medications, although the risk increases if used alongside insulin or sulfonylureas. Simultaneously, it suppresses the release of glucagon—a hormone that raises blood glucose—thereby preventing excessive glucose production by the liver.
Additionally, Rybelsus slows gastric emptying, which moderates the rate at which glucose enters the bloodstream after meals. Many patients also experience reduced appetite and modest weight loss, which can further improve glycaemic control.
Rybelsus must be taken in a specific way: once daily in the morning on an empty stomach with up to 120 ml of water, followed by waiting at least 30 minutes before consuming food, drink or other medicines. Treatment starts with a 3 mg dose for 30 days (for tolerability, not glycaemic control), then increases to 7 mg daily, with a further increase to 14 mg if needed for optimal glycaemic control.
Common side effects include gastrointestinal symptoms (nausea, diarrhoea, vomiting). Serious but less common adverse reactions include pancreatitis and gallbladder disease; patients should seek urgent medical advice for severe, persistent abdominal pain or vomiting. Rapid improvement in blood glucose control may worsen diabetic retinopathy in some patients.
Currently, Rybelsus is licensed exclusively for type 2 diabetes management and is not licensed by the Medicines and Healthcare products Regulatory Agency (MHRA) or recommended by NICE for the treatment of prediabetes.
Evidence for Rybelsus in Prediabetes Management
While Rybelsus has demonstrated robust efficacy in type 2 diabetes, there is currently no official indication or regulatory approval for its use in prediabetes. Prediabetes—defined as impaired fasting glucose (IFG) or impaired glucose tolerance (IGT)—represents an intermediate metabolic state where blood glucose levels are elevated but not yet high enough to meet diagnostic criteria for diabetes.
Some clinical research has explored whether GLP-1 receptor agonists, including semaglutide, might delay or prevent progression from prediabetes to type 2 diabetes. However, it's important to note that most supportive evidence comes from studies using different semaglutide formulations and doses than those in Rybelsus. The STEP trials evaluated injectable semaglutide 2.4 mg weekly (Wegovy) for obesity, while the OASIS trials studied high-dose oral semaglutide (50 mg) for weight management—both substantially different from Rybelsus doses (7 mg or 14 mg daily) used in diabetes. Specific large-scale trials evaluating Rybelsus at its licensed doses for prediabetes prevention are lacking, and the medication has not been assessed by NICE or the MHRA for this purpose.
The absence of a licensed indication means that prescribing Rybelsus for prediabetes would be off-label in the UK. Off-label prescribing should be exceptional, specialist-led, and consistent with GMC guidance, requiring documented informed consent. Rybelsus is not commissioned by the NHS for prediabetes management.
Key considerations include:
-
The lack of long-term safety and efficacy data specifically in prediabetic populations at Rybelsus licensed doses
-
Potential adverse effects, including gastrointestinal symptoms (nausea, vomiting, diarrhoea), pancreatitis and gallbladder disease
-
Cost implications, as Rybelsus is not commissioned by the NHS for prediabetes
Patients with prediabetes should be aware that lifestyle interventions remain the cornerstone of evidence-based management, with pharmacological options reserved for specific circumstances under specialist guidance.
NHS-Recommended Treatments for Prediabetes
The National Institute for Health and Care Excellence (NICE) provides clear guidance on managing prediabetes, formally termed non-diabetic hyperglycaemia (NDH). In the UK, NDH is defined as an HbA1c of 42-47 mmol/mol (6.0-6.4%) or fasting plasma glucose of 5.5-6.9 mmol/L. The primary focus is on intensive lifestyle modification, which has been shown in landmark trials to reduce the risk of progression to type 2 diabetes by up to 58%, with the NHS Diabetes Prevention Programme showing meaningful but variable results in routine practice.
NICE-recommended lifestyle interventions include:
-
Dietary modification: Adopting a balanced diet rich in vegetables, wholegrains, and lean proteins while reducing intake of refined carbohydrates, sugary foods, and saturated fats. Referral to a dietitian or participation in structured education programmes such as the NHS Diabetes Prevention Programme (NHS DPP) can provide tailored support.
-
Physical activity: Aiming for at least 150 minutes of moderate-intensity aerobic exercise per week, combined with resistance training on two or more days. Activities such as brisk walking, cycling, or swimming are effective and accessible.
-
Weight management: Achieving and maintaining a healthy body weight, particularly for individuals with a BMI ≥25 kg/m² (or ≥23 kg/m² for people of South Asian, Chinese, or other Asian origin). Even modest weight loss (5–10% of body weight) can significantly improve insulin sensitivity and glycaemic control.
-
Smoking cessation and alcohol moderation: Addressing these modifiable risk factors further reduces cardiovascular risk, which is elevated in prediabetes.
Pharmacological intervention is not routinely recommended for prediabetes in the UK. However, metformin may be considered in specific circumstances, such as when lifestyle measures have been insufficient and the individual has additional risk factors (e.g., BMI ≥35 kg/m², age under 60, a history of gestational diabetes, or rising HbA1c despite lifestyle changes). Metformin is an off-label use in this context but has evidence supporting its role in diabetes prevention.
Regular monitoring—typically HbA1c testing every 6-12 months depending on risk factors and previous results—is advised to detect progression to diabetes early (HbA1c ≥48 mmol/mol or fasting plasma glucose ≥7.0 mmol/L) and adjust management accordingly.
When to Speak with Your GP About Blood Sugar Control
If you have been diagnosed with prediabetes or are concerned about your blood sugar levels, early engagement with your GP or practice nurse is essential. Prediabetes often presents without symptoms, so many individuals are unaware of their elevated glucose levels until identified through routine screening or health checks.
You should arrange a consultation if:
-
You have risk factors for type 2 diabetes, including a family history, obesity (BMI ≥30 kg/m², or ≥23 kg/m² for South Asian, Chinese or other Asian backgrounds), South Asian or African-Caribbean ethnicity, a history of gestational diabetes, or polycystic ovary syndrome (PCOS)
-
You have been told you have prediabetes (HbA1c 42-47 mmol/mol or fasting glucose 5.5-6.9 mmol/L) but have not received structured advice on lifestyle modification or follow-up monitoring
-
You are struggling to implement dietary or physical activity changes and would benefit from referral to specialist services such as the NHS Diabetes Prevention Programme
-
You experience symptoms suggestive of hyperglycaemia, such as increased thirst, frequent urination, unexplained weight loss, fatigue, or recurrent infections (these may indicate progression to diabetes)
-
You are interested in discussing pharmacological options and wish to understand whether metformin or other interventions might be appropriate in your individual circumstances
Seek same-day medical help if you experience severe symptoms such as extreme thirst, persistent vomiting, drowsiness or confusion, which could indicate very high blood glucose levels requiring urgent attention.
Your GP can:
-
Arrange blood tests (fasting glucose, HbA1c, or oral glucose tolerance test) to confirm your metabolic status
-
Provide personalised advice on diet, exercise, and weight management
-
Refer you to dietetic services, structured education programmes, or specialist diabetes clinics if needed
-
Monitor your progress with regular follow-up appointments and repeat blood tests
Early intervention in prediabetes offers a valuable opportunity to prevent or delay the onset of type 2 diabetes and reduce associated complications. Do not delay seeking professional advice—your primary care team is well-equipped to support you in making sustainable, evidence-based changes to protect your long-term health.
If you experience any side effects from medications, report them through the MHRA Yellow Card scheme (yellowcard.mhra.gov.uk).
Frequently Asked Questions
Is Rybelsus approved for prediabetes in the UK?
No, Rybelsus is not approved by the MHRA or recommended by NICE for prediabetes treatment. It is licensed exclusively for type 2 diabetes mellitus in adults, and prescribing it for prediabetes would be off-label.
What is the recommended treatment for prediabetes in the UK?
NICE recommends intensive lifestyle modification as first-line treatment, including dietary changes, at least 150 minutes of weekly physical activity, weight management, and smoking cessation. Metformin may be considered off-label in specific high-risk circumstances when lifestyle measures are insufficient.
When should I see my GP about prediabetes?
Consult your GP if you have risk factors such as family history, obesity, South Asian or African-Caribbean ethnicity, gestational diabetes history, or PCOS. Also seek advice if you have been diagnosed with prediabetes but lack structured support, or if you experience symptoms such as increased thirst, frequent urination, or unexplained weight loss.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript