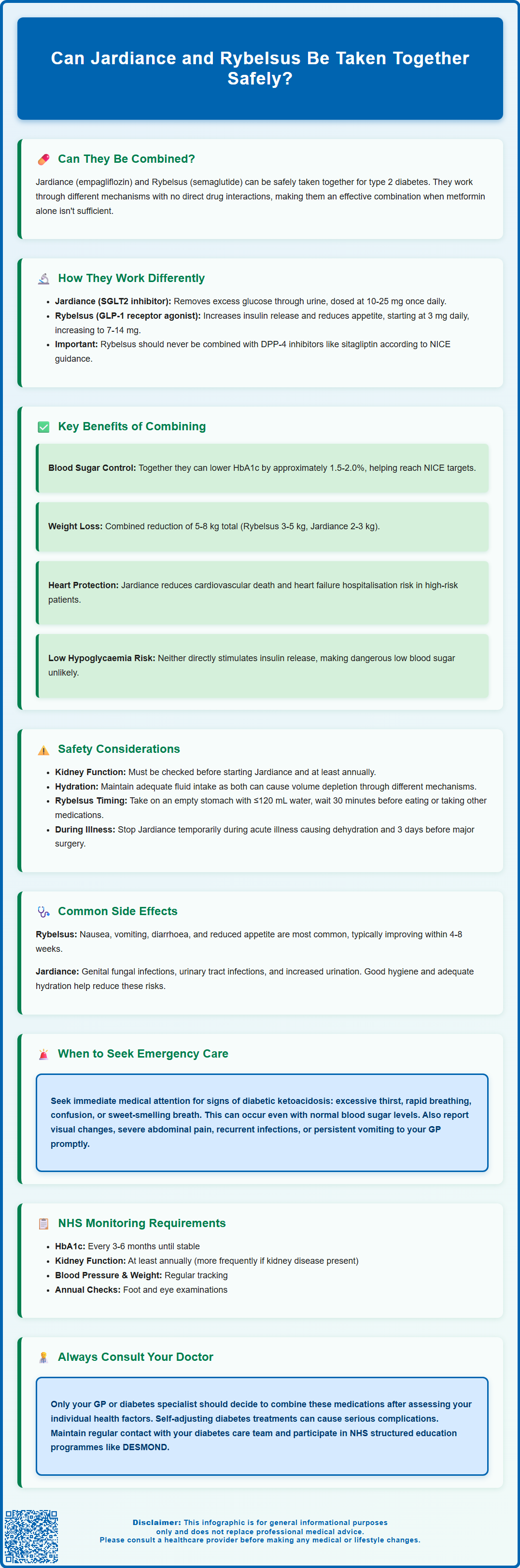
Can Jardiance and Rybelsus be taken together for type 2 diabetes? Yes, these two medications are commonly prescribed in combination to improve blood glucose control in adults with type 2 diabetes mellitus. Jardiance (empagliflozin) is an SGLT2 inhibitor that works in the kidneys to remove excess glucose through urine, whilst Rybelsus (semaglutide) is a GLP-1 receptor agonist that enhances insulin secretion and reduces appetite. Their complementary mechanisms make them effective partners in diabetes management, particularly when metformin alone proves insufficient. This article explores the safety, benefits, side effects, and NHS guidance on using these medications together.
Summary: Jardiance and Rybelsus can be safely taken together for type 2 diabetes, as they work through different mechanisms with no significant drug interactions.
- Jardiance is an SGLT2 inhibitor that promotes urinary glucose excretion; Rybelsus is a GLP-1 receptor agonist that enhances insulin secretion and delays gastric emptying.
- The combination offers complementary glycaemic control, cardiovascular benefits, and weight reduction without significantly increasing hypoglycaemia risk.
- Common side effects include gastrointestinal symptoms (nausea, vomiting) from Rybelsus and genitourinary infections from Jardiance.
- Renal function should be monitored at least annually, and Jardiance should be temporarily stopped during acute illness or before major surgery.
- NICE guidance supports this combination when dual therapy is needed to achieve individualised HbA1c targets in type 2 diabetes management.
Table of Contents
Can Jardiance and Rybelsus Be Taken Together?
Yes, Jardiance (empagliflozin) and Rybelsus (semaglutide) can be taken together, and this combination is used for adults with type 2 diabetes mellitus. Both medications work through different mechanisms to improve glycaemic control, making them complementary in their actions. Jardiance belongs to the sodium-glucose co-transporter 2 (SGLT2) inhibitor class, whilst Rybelsus is a glucagon-like peptide-1 (GLP-1) receptor agonist—the first oral formulation of semaglutide available in the UK.
Clinical evidence supports the concurrent use of these agents, and there are no direct pharmacological interactions that would contraindicate their combined administration. The Medicines and Healthcare products Regulatory Agency (MHRA) has approved both medications for use in type 2 diabetes, and prescribing information for each drug acknowledges their potential use alongside other glucose-lowering therapies. Many patients require combination therapy to achieve optimal HbA1c targets, particularly when metformin monotherapy proves insufficient.
Jardiance is typically prescribed as 10 mg once daily, which may be increased to 25 mg if needed for glycaemic control. Rybelsus starts at 3 mg once daily for 30 days, then increases to 7 mg daily, with a further increase to 14 mg possible if needed for glycaemic control.
It's important to note that GLP-1 receptor agonists like Rybelsus should not be used in combination with DPP-4 inhibitors (such as sitagliptin or linagliptin), as per NICE guidance.
It is essential that any decision to combine these medications is made by your prescribing clinician, typically a GP or diabetes specialist. They will assess your individual circumstances, including current glycaemic control, renal function, cardiovascular risk profile, and any contraindications. Self-adjusting diabetes medications or adding new treatments without medical supervision can lead to complications, including hypoglycaemia or metabolic disturbances. If you are currently taking one of these medications and your healthcare provider suggests adding the other, this represents standard clinical practice aligned with NICE guidance on intensifying diabetes management when treatment targets are not met with existing therapy.
Safety and Drug Interactions Between Jardiance and Rybelsus
From a pharmacological perspective, Jardiance and Rybelsus do not exhibit significant drug-drug interactions that would preclude their concurrent use. Jardiance works primarily in the kidneys by inhibiting SGLT2 transporters in the proximal tubule, promoting urinary glucose excretion independently of insulin. Rybelsus acts systemically by mimicking endogenous GLP-1, enhancing glucose-dependent insulin secretion, suppressing glucagon release, and slowing gastric emptying. These distinct mechanisms mean the drugs do not compete for the same metabolic pathways or receptor sites.
However, certain safety considerations warrant attention when using both medications together. Jardiance increases urinary glucose excretion, which can elevate the risk of genitourinary infections, including vulvovaginal candidiasis and urinary tract infections. Rybelsus commonly causes gastrointestinal adverse effects, particularly nausea, which may be more pronounced during treatment initiation. When combined, patients should be monitored for cumulative side effects, though these typically reflect the individual safety profiles rather than synergistic toxicity.
Renal function monitoring is important with this combination. For Jardiance, renal function should be assessed before starting treatment and at least annually thereafter (more frequently in those with chronic kidney disease or at risk of renal impairment). For glycaemic control, Jardiance's efficacy diminishes with declining renal function. However, Jardiance may be used at lower eGFR levels (≥20 mL/min/1.73m²) for heart failure or chronic kidney disease indications per the SmPC. It is not recommended in end-stage renal disease or for patients on dialysis. Rybelsus does not require renal dose adjustment but should be used cautiously in severe renal impairment.
Both medications can contribute to volume depletion—Jardiance through osmotic diuresis and Rybelsus through reduced oral intake due to nausea—so adequate hydration is essential. Importantly, Jardiance should be temporarily stopped during periods of acute illness causing dehydration and usually 3 days before major surgery to reduce the risk of diabetic ketoacidosis (DKA). Treatment can be restarted when eating and drinking normally.
Rybelsus may increase the exposure of levothyroxine, so thyroid function should be monitored if both are used. For patients on warfarin, INR monitoring is advised when starting or changing Rybelsus dosage. Rybelsus should be taken on an empty stomach with no more than 120 mL of water, waiting at least 30 minutes before eating, drinking, or taking other oral medications.
Patients with diabetic retinopathy should be monitored closely when using Rybelsus, as rapid improvement in glucose control may temporarily worsen retinopathy, particularly in those with pre-existing disease.
Neither medication is indicated for type 1 diabetes or for the treatment of diabetic ketoacidosis.
Patients taking other medications should inform their healthcare provider, as both drugs may interact with diuretics, antihypertensives, or insulin/sulphonylureas, potentially increasing hypoglycaemia risk or affecting blood pressure. Regular review by your GP or diabetes team ensures safe, effective combination therapy tailored to your clinical needs.
Benefits of Combining Jardiance and Rybelsus
The combination of Jardiance and Rybelsus offers multiple therapeutic advantages beyond glycaemic control alone, addressing several aspects of type 2 diabetes management. Jardiance has proven cardiovascular benefits, reducing the risk of cardiovascular death and hospitalisation for heart failure in high-risk patients, as recognised in NICE guidance (NG28). While injectable semaglutide has demonstrated cardiovascular risk reduction in clinical trials, it's important to note that Rybelsus (oral semaglutide) does not currently have a specific cardiovascular risk reduction indication in its UK licence, though research in this area continues to evolve.
Weight management represents another significant benefit of this combination. Rybelsus typically promotes weight loss through appetite suppression and delayed gastric emptying, with patients often experiencing 3-5 kg reductions over several months. Jardiance contributes modest weight loss (typically 2-3 kg) through caloric loss via glycosuria. For patients with type 2 diabetes and obesity—a common comorbidity—this dual weight-reducing effect can improve metabolic parameters, reduce insulin resistance, and enhance overall cardiovascular risk profiles.
Glycaemic control improvements are often substantial when combining these agents. Clinical studies of SGLT2 inhibitors and GLP-1 receptor agonists together have demonstrated HbA1c reductions of approximately 1.5-2.0% (16-22 mmol/mol), depending on baseline values. This allows many patients to achieve NICE-recommended HbA1c targets (typically ≤53 mmol/mol or ≤58 mmol/mol depending on individual circumstances) without requiring insulin therapy. The complementary mechanisms—Jardiance providing insulin-independent glucose lowering and Rybelsus enhancing physiological insulin response—create additive effects whilst maintaining a low hypoglycaemia risk, as neither drug directly stimulates insulin release in the absence of elevated glucose levels. This safety profile represents a considerable advantage over older diabetes medications such as sulphonylureas.
Side Effects When Taking Both Medications
When taking Jardiance and Rybelsus together, patients may experience side effects attributable to either medication individually, though serious adverse events remain uncommon. Understanding the potential side effect profile helps patients recognise normal treatment responses versus concerning symptoms requiring medical attention.
Gastrointestinal symptoms are the most frequently reported adverse effects with this combination, primarily attributable to Rybelsus. These include:
-
Nausea (affecting up to 20% of patients initially, usually diminishing over 4-8 weeks)
-
Vomiting and diarrhoea (less common but can occur during dose escalation)
-
Reduced appetite (often considered therapeutically beneficial but may be troublesome for some)
-
Abdominal discomfort or bloating
These effects typically improve with continued use. Taking Rybelsus correctly—on an empty stomach with no more than 120 mL water, waiting 30 minutes before eating—optimises absorption and may reduce gastrointestinal symptoms.
Genitourinary effects primarily relate to Jardiance and include:
-
Genital fungal infections (vulvovaginal candidiasis in women, balanitis in men)
-
Urinary tract infections
-
Increased urination frequency (due to glycosuria)
-
Symptoms of volume depletion (dizziness, particularly on standing)
Maintaining good genital hygiene and adequate hydration helps minimise these risks. Recurrent infections should be reported to your GP.
Other important considerations include:
-
Diabetic retinopathy: Rybelsus may temporarily worsen existing diabetic retinopathy, particularly with rapid HbA1c improvement. Report any visual changes promptly.
-
Gallbladder disease: GLP-1 receptor agonists like Rybelsus may increase the risk of gallstones. Seek medical advice if you experience right upper abdominal pain, fever, or yellowing of the skin/eyes.
-
Sick day management: Jardiance should be temporarily stopped during periods of acute illness with dehydration or reduced food/fluid intake, and usually 3 days before major surgery, to reduce diabetic ketoacidosis risk. Restart when eating and drinking normally.
Rare but serious adverse effects require immediate medical attention:
-
Diabetic ketoacidosis (DKA)—even with near-normal blood glucose (euglycaemic DKA) associated with SGLT2 inhibitors—seek emergency care (999/A&E) if you experience excessive thirst, rapid breathing, confusion, unusual fatigue, or sweet-smelling breath
-
Severe pancreatitis (persistent severe abdominal pain radiating to the back)—requires urgent medical assessment
-
Acute kidney injury (reduced urine output, swelling, confusion)
-
Fournier's gangrene (necrotising fasciitis of the perineum—extremely rare but requires emergency treatment)
Contact your GP promptly if you experience persistent vomiting, severe abdominal pain, signs of dehydration, genital pain or swelling, or feeling generally unwell. Most patients tolerate this combination well, but individualised monitoring ensures early detection and management of any adverse effects.
Suspected adverse reactions should be reported via the MHRA Yellow Card Scheme (yellowcard.mhra.gov.uk or via the Yellow Card app).
NHS Guidance on Using Jardiance with Rybelsus
NICE guidance on type 2 diabetes management (NG28, updated regularly) provides the framework for prescribing decisions regarding Jardiance and Rybelsus within the NHS. According to current recommendations, treatment intensification beyond metformin should be individualised based on patient factors including HbA1c levels, cardiovascular risk, presence of chronic kidney disease, heart failure, and patient preferences regarding weight management and hypoglycaemia risk.
SGLT2 inhibitors like Jardiance are specifically recommended for patients with type 2 diabetes and established cardiovascular disease or heart failure, regardless of baseline HbA1c, due to their proven cardiovascular and renal protective effects. GLP-1 receptor agonists such as Rybelsus are recommended when additional glucose lowering is needed, particularly for patients who would benefit from weight loss or where avoiding hypoglycaemia is a priority. The combination of both drug classes is explicitly supported when dual therapy proves insufficient to achieve individualised HbA1c targets. Importantly, NICE guidance advises against combining GLP-1 receptor agonists (like Rybelsus) with DPP-4 inhibitors (such as sitagliptin or linagliptin).
NHS prescribing of Rybelsus specifically may be subject to local formulary decisions, as it represents a newer option compared to injectable GLP-1 receptor agonists. Some integrated care boards (ICBs) may have specific criteria or pathways for Rybelsus prescribing, which may vary by region. Availability and access to both medications may differ depending on local NHS formularies and prescribing guidelines.
Monitoring requirements under NHS care typically include:
-
HbA1c assessment every 3-6 months until stable, then at least annually
-
Renal function testing (eGFR and urine albumin:creatinine ratio) at baseline and at least annually, or more frequently in those with chronic kidney disease or at risk of renal impairment
-
Blood pressure monitoring as both medications can affect cardiovascular parameters
-
Weight tracking to assess therapeutic response
-
Foot examination annually as part of comprehensive diabetes care
-
Eye screening annually, with more frequent monitoring if pre-existing diabetic retinopathy, particularly when starting Rybelsus
Patients should maintain regular contact with their diabetes care team, whether through GP surgeries or specialist diabetes clinics. Any concerns about medication effectiveness, side effects, or changes in health status should be discussed promptly. The NHS also provides structured diabetes education programmes (such as DESMOND for type 2 diabetes) that can help patients understand their medications and optimise self-management alongside pharmacological therapy.
Frequently Asked Questions
Do Jardiance and Rybelsus interact with each other?
No, Jardiance and Rybelsus do not have significant drug-drug interactions as they work through different mechanisms—Jardiance acts in the kidneys whilst Rybelsus works systemically on insulin secretion and appetite regulation.
What are the main side effects when taking both medications together?
The most common side effects include gastrointestinal symptoms such as nausea and vomiting from Rybelsus, and genitourinary infections including thrush and urinary tract infections from Jardiance. Most side effects are manageable and diminish over time.
Is this combination recommended by NICE for type 2 diabetes?
Yes, NICE guidance supports combining SGLT2 inhibitors like Jardiance with GLP-1 receptor agonists like Rybelsus when dual therapy is needed to achieve individualised HbA1c targets, particularly for patients requiring cardiovascular protection or weight management.
The health-related content published on this site is based on credible scientific sources and is periodically reviewed to ensure accuracy and relevance. Although we aim to reflect the most current medical knowledge, the material is meant for general education and awareness only.
The information on this site is not a substitute for professional medical advice. For any health concerns, please speak with a qualified medical professional. By using this information, you acknowledge responsibility for any decisions made and understand we are not liable for any consequences that may result.
Heading 1
Heading 2
Heading 3
Heading 4
Heading 5
Heading 6
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur.
Block quote
Ordered list
- Item 1
- Item 2
- Item 3
Unordered list
- Item A
- Item B
- Item C
Bold text
Emphasis
Superscript
Subscript